 by Olabola Awosika MD, MS; Misty G. Eleryan MD; Monica Rengifo-Pardo MD; Lindsay Doherty MS; Lisa W. Martin, MD; and Alison Ehrlich MD, MHS
by Olabola Awosika MD, MS; Misty G. Eleryan MD; Monica Rengifo-Pardo MD; Lindsay Doherty MS; Lisa W. Martin, MD; and Alison Ehrlich MD, MHS
Drs. Awosika, Rengifo-Pardo, and Ehrlich are with the Department of Dermatology, The George Washington Medical Faculty Associates in Washington, DC. Dr. Martin is with the Department of Cardiology, The George Washington Medical Faculty Associates in Washington, DC. Drs. Eleryan, Rengifo-Pardo, Martin, and Ehrlich are also with The George Washington University School of Medicine & Health Sciences in Washington, DC. Ms. Doherty is with the Department of Epidemiology and Biostatistics, School of Public Health and Health Services, George Washington University in Washington, DC.
Funding: No funding was provided.
Disclosures: Dr. Olabola Awosika’s fellowship is funded by Janssen Biotech, Inc. The other authors have no conflicts of interest relevant to the content of this article.
Abstract: Objective. International case-control studies have demonstrated that psoriasis is associated with an increased prevalence of nonalcoholic fatty liver disease (NAFLD). The purpose of the present study was to establish an association of psoriasis and NAFLD in patients attending a dermatology clinic center in the United States.
Design. This was an observational, case-control study.
Setting. The study setting was an outpatient dermatology clinic of the George Washington Medical Faculty Associates in Washington DC.
Participants. One hundred fifty-one adult patients with psoriasis and 51 control subjects were recruited.
Measurements. NAFLD was diagnosed by ultrasonography after excluding secondary causes of liver disease. Regression analysis was used to assess the associations between: 1) NAFLD and psoriasis and 2) metabolic syndrome components and NAFLD among psoriasis patients.
Results. NAFLD was more prevalent in patients with psoriasis (21.2% vs. 7.8%, p<0.04). However, psoriasis was not associated with NAFLD when matching for age, sex, and body mass index (BMI) (odds ratio: 2.63, 95% confidence interval [CI]: 0.51–13.6; p=0.25). As compared to patients with psoriasis but without NAFLD, those with NAFLD were more likely to have obesity (BMI: 34.9 vs. 27.2, 95% CI: 32.4–37.5 vs. 25.9–28.5; p<0.01). NAFLD in patients with psoriasis was also associated with select components of metabolic syndrome, including hyperglycemia and hyperlipidemia.
Conclusion. Our findings show there is an association of psoriasis with NAFLD. Our findings also suggest an increased presence of metabolic syndrome components in patients with psoriasis and NAFLD.
Trial registry. NCT00930384.
Keywords: Nonalcoholic fatty liver disease, psoriasis, metabolic syndrome, comorbidity, liver disease
J Clin Aesthet Dermatol. 2018;11(6):33–37
Introduction
Nonalcoholic fatty liver disease (NAFLD) is the most common cause of elevated liver enzymes and is predicted to be the leading cause of liver transplantation by 2020.1,2 The prevalence of NAFLD in the United States is estimated to range from 10 to 35 percent.3 The condition is characterized by the presence of hepatic pathology resembling alcoholic fatty liver disease in individuals who do not consume excessive amounts of alcohol.4 A wide spectrum of hepatic lesions is encompassed within the term NAFLD, ranging from simple fatty liver to steatohepatitis with necroinflammatory changes and variable degrees of fibrosis, which could progress to liver cirrhosis and even hepatocellular carcinoma.2,4
Hepatic ultrasonography is widely used for screening of fatty liver disease in asymptomatic patients, carrying a positive predictive value of 62 percent and a sensitivity of 100 percent in the detection of steatosis of 33 percent or greater.5,6 Notably, the prevalence of hepatic cirrhosis and nonalcoholic steatohepatitis due to NAFLD is estimated to be one percent and five percent, respectively.7 However, the pathophysiology of the development and progression of NAFLD is still not completely understood.
Risk factors for NAFLD include obesity and metabolic syndrome.8 These same comorbidities have been associated with systemic inflammation in psoriasis.9,10 Both NAFLD and psoriasis are chronic inflammatory conditions resulting from a multifactorial pathogenesis comprising hereditary and environmental factors. Specific pro-inflammatory mediators, including interleukin-6, tumor necrosis factor alpha, and C-reactive protein (CRP), have been shown to cause a chronic inflammatory state in fatty liver, psoriasis, and metabolic syndrome.7 Given this similarity, patients with psoriasis might have a linked pathogenesis to NAFLD, thus a potential increased risk for advanced hepatic disease.
This relationship has prompted case-control investigations that report an association between psoriasis and NAFLD.7,10–12 In an Italian retrospective study,11 NAFLD was 19 percent more frequent in subjects with psoriasis and associated with a higher Psoriasis Area of Severity Index (PASI) score.11 These findings were further supported by a 10-percent increased prevalence of NAFLD in patients with psoriasis in an Indian cohort7 and a 70-percent increased likelihood of NAFLD in those over the age of 55 years in the Netherlands.12 However, in an American study,13 the frequency of NAFLD in patients with psoriasis was nonstatistically significantly different from in controls. To our knowledge, there have been no published reports in the United States confirming a significantly higher prevalence of NAFLD in patients with psoriasis compared to healthy controls.
The aim of this study was to investigate the association of psoriasis and the presence of NAFLD in patients with psoriasis who attended a tertiary dermatology clinic center in the United States in comparison to a nonpsoriatic population. Specifically, we examined 1) the association between psoriasis and NAFLD and 2) the association of baseline characteristics (including presence of components of the metabolic syndrome, severity of psoriasis, and body mass index [BMI]) and NAFLD in patients with psoriasis.
Methods
The psoriasis clinic at the Department of Dermatology at the George Washington Medical Faculty Associates (GW MFA) receives a higher than average number of psoriatic cases in the Washington, DC, area, which enabled us to consider a large array of patients with mild, moderate, or severe phenotypes of psoriasis for this study.
Sample size estimation. As the incidence rate of NAFLD in patients with psoriasis within the United States is unknown, power analysis done to determine sample size was based on previously reported prevalence estimates.11 Gisondi et al11 performed a study estimating the prevalence of NAFLD among patients with psoriasis from Italy, documenting a prevalence of 47 percent versus 28 percent among controls. Assuming a similar prevalence of approximately 45 percent in patients with psoriasis, we calculated a sample size of 101 cases and 51 controls in order to detect a 15-percent difference in the prevalence of NAFLD between subjects with or without psoriasis. The larger case population of 101 patients with psoriasis in comparison with the control group of 51 participants provided at least an 80-percent power with an ? risk of 0.05.
Study population. Subjects ranging from 18 to 80 years in age were recruited from the GW MFA between December 1, 2009, and September 30, 2014. The two cohorts included patients with moderate-to-severe psoriasis attending the dermatology clinic and age-, sex-, and BMI-matched healthy controls without psoriasis. Patients with psoriasis were included if confirmed to have moderate-to-severe psoriasis based on the following criteria: 1) body surface area (BSA) involvement greater than 10 percent and 2) a PASI score greater than 10.14 Patients with excess daily alcohol intake; chronic liver disease; presence of hepatitis B virus surface antigen and/or hepatitis C virus antibodies; history of specific oral or injectable medications associated with fatty liver (including methotrexate, systemic corticosteroids, amiodarone, tamoxifen, estrogens, or nifedipine); pregnancy; and/or conditions hindering data collection and follow-up were excluded. This study was approved by the institutional review board of The George Washington University. Written informed consent was provided by all patients prior to participation, and all patient data were deidentified.
Diagnosis of NAFLD and metabolic syndrome components. NAFLD was evaluated by hepatic ultrasonography performed by a staff radiologist. Subjects were considered as screening positive for NAFLD if fatty liver was present as defined by the standard criteria accepted by the American Gastroenterological Association.15 Specifically, the liver was considered normal if there was homogeneous echotexture with no acoustic attenuation, the portal veins and diaphragm were well visualized, and the echogenicity was similar to or slightly higher than that of the renal parenchyma. A clinical diagnosis of NAFLD was made when there were areas of increased echogenicity relative to the renal parenchyma, increased attenuation of the ultrasound beam with the diaphragm indistinct, or if there was lack of differentiation in periportal intensity and the vesicular wall.1,15
In addition to NAFLD, components of metabolic syndrome were measured. We adopted the definition of the National Cholesterol Education Program’s Adult Treatment Panel III (ATP III), in which metabolic syndrome is diagnosed as the presence of three or more of the following components: 1) fasting serum glucose level of at least 100mg/dL or previous diagnosis of Type 2 diabetes mellitus; 2) blood pressure of at least 130/85mmHg or treatment for hypertension; 3) serum triglyceride level of at least 150mg/dL; 4) serum high-density lipoprotein (HDL) cholesterol concentration of less than 40mg/dL in men and less than 50mg/dL in women; and 5) abdominal obesity, defined as waist circumference exceeding 102cm in men and 88cm in women.16 A BMI of at least 30 was used to classify levels of obesity based on the American College of Endocrinology diagnostic approach to obesity.17
Biochemical analysis. All participants underwent fasting blood tests to determine levels of glucose, insulin, total cholesterol, total triglyceride, HDL cholesterol, low-density lipoprotein (LDL) cholesterol, very-low-density lipoprotein cholesterol (VLDL-Chol), high-sensitivity CRP (hs-CRP), aspartate aminotransferase (AST), and alanine aminotransferase (ALT). Additional blood tests in participants found to have evidence of fatty liver disease on ultrasound included hepatitis B antigen and antihepatitis C viral infection antibodies.
Statistical analysis. The two cohorts were matched for age, sex, and BMI. Baseline characteristics and components of fatty liver disease were examined, and significant differences were detected using the Wilcoxon two-sample test for continuous variables and the chi-squared test or Fisher’s exact test for categorical variables. Wilcoxon two-sample tests were executed to observe differences in the raw data between psoriasis cases and controls. Conditional logistic regression models were performed, and odds ratios (OR) were computed to examine the association between the presence of NAFLD and psoriasis. Linear regression and chi-squared values were performed to assess the association between variables of interest and PASI score among patients with psoriasis. PASI scores were log-transformed to meet normality assumptions of linear regression, and parameter estimates were then back-transformed to obtain the true parameter estimate. Adjusted least-squared means and corresponding 95-percent confidence intervals (CIs) were also computed to assess the associations between baseline covariates and NAFLD among psoriasis patients. All analyses were performed using SAS version 9.3 (SAS Institute Inc., Cary, North Carolina) and p<0.05 was considered to be statistically significant.
Results
Characteristics of study groups. A total of 161 individuals participated in the study, including 101 patients with psoriasis and 51 controls (Table 1). The mean age of the participants was 44.2 years±13.6 years in the psoriasis group and 44.7 years±14.5 years in the control group. There were 49 male subjects (48.5%) and 18 male subjects (35.2%) in the psoriasis and control cohorts, respectively. Patients with psoriasis had significantly higher BMI values than the control patients (29.2 vs. 25.4kg/m2; p<0.01), with both groups being overweight on average.
Patients with psoriasis had mean values of HDL, triglycerides, and glucose below the minimum criteria for metabolic syndrome as defined by the ATP III (Table 2).15 However, the mean waist circumference was 96.1±18cm, which is between the values for risk of obesity for men (102cm) and women (88cm), according to the ATP III. Only two patients with psoriasis were found to have metabolic syndrome.
Prevalence of NAFLD. The occurrence of NAFLD on ultrasound was greater in patients with psoriasis than the reference population (21.2% vs. 7.8%, p<0.04) (Table 3). Patients with psoriasis also had greater incidence of impaired visualization of the diaphragm (8.1% vs. 0%, p<0.04). There were no statistically significant differences between patients with psoriasis and controls with respect to all other ultrasound findings.
Conditional logistic regression analysis was performed to assess the association between ultrasound components of NAFLD and psoriasis in patients with psoriasis matched to controls by age, sex, and BMI (Table 4). Patients with psoriasis were more likely to have ultrasound findings consistent with NAFLD by 263 percent, but this difference was not significant (OR: 2.63; 95% CI: 0.51–13.6; p=0.25). There were no significant associations detected between NAFLD ultrasound components and psoriasis.
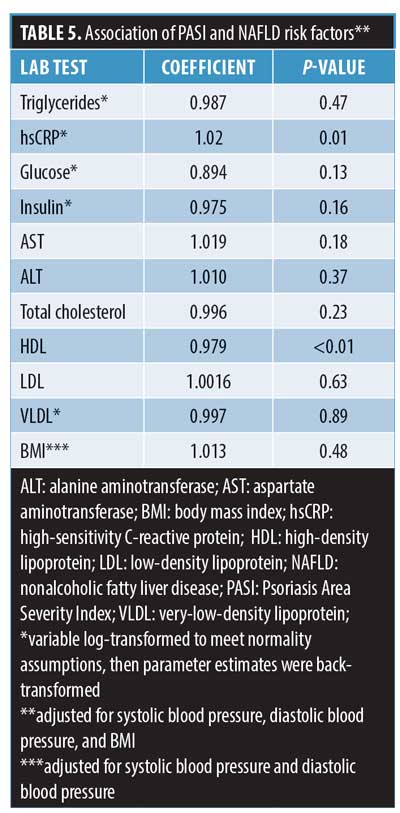
Association of PASI and risk factors of NAFLD. Adjusted linear regression analysis showed that PASI score was significantly associated with hsCRP and HDL after adjusting for systolic and diastolic blood pressure and BMI (Table 5). For every 10-percent increase in hsCRP, PASI score was found to increase by two percent (R=1.02, p=0.01). Similarly, for every one-unit increase in HDL, PASI score decreased significantly by 2.1 percent (R=0.979, p<0.01). Correlations of PASI with the remaining risk factors were not statistically significant.
Patients with psoriasis with or without NAFLD. After adjusting for systolic and diastolic blood pressure and BMI, adjusted least-square means analysis demonstrated that patients with psoriasis and NAFLD had significantly higher levels of glucose, AST, ALT, triglycerides, and VLDL (Table 6). In comparison to patients with psoriasis who did not have NAFLD, those with NAFLD were more likely to have obesity (BMI: 34.9 vs. 27.2, 95% CI: 32.4–37.5 vs. 25.9–28.5; p<0.01). All other characteristics did not significantly differ between the groups.
Discussion
Psoriasis is a common inflammatory disorder of the skin that has been shown to be associated with comorbid diseases. International studies suggest an increased prevalence of NAFLD in psoriasis. This increased risk of NAFLD was explained by an increased occurrence of metabolic syndrome and insulin resistance promoting the development of hepatic steatosis.4 This risk is important given that patients with psoriasis are often candidates to be treated with hepatotoxic agents such as methotrexate, and underlying liver disease could be exacerbated by these medications.10,18 Discernment of factors predisposing this population to NAFLD is pertinent for the implementation of screening and treatment in high-risk psoriasis patients. In this case-control study, we evaluated the association of NAFLD with psoriasis in patients at a United States urban-based tertiary dermatology clinic center.
The prevalence of NAFLD in our patients with psoriasis was significantly higher than in our reference population (21.2% vs. 7.8%). This prevalence estimate is comparable to the results of an Indian hospital-based study in which the occurrence of NAFLD was 17.4 percent and 7.9 percent in psoriasis patients and age-, sex-, and BMI-matched controls, respectively.12 The lower NAFLD occurrence in this Indian population could be explained by the use of an alternative definition of NAFLD (i.e., evidence of steatosis on liver ultrasound and elevation of liver enzymes and triglycerides) and ethnic differences in risk factors. In contrast, three prior case-control studies conducted involving Italian and Netherlands populations found higher NAFLD prevalence rates of 46 to 59.2 percent in their patients with psoriasis.7,10,11 This difference is likely attributable to the extensive list of hepatotoxic agents in the exclusion criteria for our study. None of these studies specify exclusion based on a history of estrogen or nifedipine use, which could have led to an overestimation in the prevalence of NAFLD in these studies. Additionally, the mean age for participants in the Netherlands study was 76.2 years, and the prevalence of NAFLD increases with age.7,19
In this study, psoriasis was not associated with NAFLD when our patients were matched by age, sex, and BMI. This finding is consistent with a cross-sectional study of 388 military patients in which there was no significant difference in risk of NAFLD among patients with psoriasis versus controls (OR: 1.03, 95% CI: 0.59–1.78).13,20 In contrast, in a recent meta-analysis of seven case-control studies, patients with psoriasis had an increased risk of NAFLD compared to the nonpsoriatic reference populations in six studies (n=267,761; OR: 2.15, 95% CI: 1.57–2.94).20 This association remained significant when only high-quality studies were analyzed (n=3,345; OR: 2.07, 95% CI: 1.62–2.64).20 Metabolic syndrome was also more common in the psoriatic populations for these studies, particularly in the two high-quality studies, which matched for age, sex, and BMI (n=1,053; OR: 1.39, 95% CI: 1.03–1.87).20 As compared to the prevalence of metabolic syndrome in patients with psoriasis of prior case-control studies (28–62%), our patients were far less likely to have metabolic syndrome (2%).7,10,11 It is presumed that the association of NAFLD with patients with psoriasis in prior studies is due to the high rates of metabolic syndrome in these international populations. Moreover, a better conclusion might be that patients with psoriasis and metabolic syndrome are more likely to have NAFLD than are patients without psoriasis.
We found that patients with psoriasis and NAFLD were more likely to have elevation of components of metabolic syndrome than patients without NAFLD. Both BMI (34.9), and triglycerides (134.9) were significantly elevated in the NAFLD group. AST and ALT were also significantly higher in this population. Both Miele et al10 and Madanagobalane12 reported similar findings with AST, ALT, and metabolic components in their patients with psoriasis and NAFLD versus patients with psoriasis but without NAFLD. These findings support that, despite normal liver function tests, liver ultrasound should be considered in patients with psoriasis who are within the range of criteria for metabolic syndrome.
Limitations. Several study limitations should be noted. First, ultrasonography and exclusion of secondary causes of chronic liver disease were used to make a clinical diagnosis of NAFLD. Though ultrasonography has a high sensitivity for hepatic steatosis, characteristic features of steatosis, including blurring of vasculature and increased brightness, are also observed in fibrosis and early cirrhosis.8 Liver biopsy remains the gold standard for staging of liver disease.7 However, in a population-based study, we determined it unethical to perform a liver biopsy, given its associated morbidity and mortality.21 Additionally, because our study was done at a single tertiary center, referral bias should be considered. However, this is unlikely, given that many of the study participants were self-referred and encompassed a diverse geographic distribution.
Conclusion
In conclusion, NAFLD appears to occur more frequently in patients with psoriasis than in the general population. However, this occurrence is likely attributed to the presence of metabolic syndrome or an elevation of its components in patients with psoriasis and NAFLD. This study highlights that NAFLD might not be associated with psoriasis but rather with the increased levels of metabolic syndrome components in patients with psoriasis and NAFLD. Physicians should consider diagnostic imaging in patients with psoriasis who have or are at risk of developing metabolic syndrome.
References
- Williams CD, Stengel J, Asike MI, et al. Prevalence of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis among a largely middle-aged population utilizing ultrasound and liver biopsy: a prospective study. Gastroenterology. 2011;140(1):124–131.
- Musso G, Gambino R, Cassader M, Pagano G. Meta-analysis: natural history of non-alcoholic fatty liver disease (NAFLD) and diagnostic accuracy of non-invasive tests for liver disease severity. Ann Med. 2011;43(8):617–649.
- Vernon G, Baranova A, Younossi ZM. Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment Pharmacol Ther. 2011;34(3):274–285.
- Wenk KS, Arrington KC, Ehrlich A. Psoriasis and non-alcoholic fatty liver disease. J Eur Acad Dermatol Venereol. 2011;25(4):383–391.
- Saadeh S, Younossi ZM, Remer EM, et al. The utility of radiological imaging in nonalcoholic fatty liver disease. Gastroenterology. 2002;123(3):745–750.
- Charatcharoenwitthaya P, Lindor KD. Role of radiologic modalities in the management of non-alcoholic steatohepatitis. Clin Liver Dis. 2007;11(1):37–54.
- van der Voort EA, Koehler EM, Dowlatshahi EA, et al. Psoriasis is independently associated with nonalcoholic fatty liver disease in patients 55 years old or older: results from a population-based study. J Am Acad Dermatol. 2014;70(3):517–524.
- Rinella M. Nonalcholic fatty liver disease: a systematic review. JAMA. 2015;313(22):2263–2273.
- Hensler T, Christophers E. Disease concomitance in psoriasis. J Am Acad Dermatol. 1995;32(6):982–986.
- Miele L, Vallone S, Cefalo C, et al. Prevalence, characteristics, and severity of non-alcoholic fatty liver disease in patients with chronic plaque psoriasis. J Hepatol. 2009;51(4):778–786.
- 11. Gisondi P, Targher G, Zoppini G, Girolomoni G. Non-alcoholic fatty liver disease in patients with chronic plaque psoriasis. J Hepatol. 2009;51(4):
758–764. - Madanagobalane S, Anandan S. The increased prevalence of non-alcoholic fatty liver disease in psoriatic patients: a study from South India. Australas J Dermatol. 2012;53(3):190–197.
- Fewell A, Lamb PB, Roberts KK, et al. The prevalence of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH) among patients with psoriasis and psoriatic arthritis in a tertiary care dermatology and rheumatology clinic. Hepatology. 2012;56:897A.
- Menter A, Korman NJ, Elmets CA, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis. Section 3. Guidelines of care for the management and treatment of psoriasis with topical therapies. J Am Acad Dermatol. 2009;60(4):643–659.
- Sanyal AJ. AGA technical review on nonalcoholic fatty liver disease. Gastroenterology. 2002;123(5):1705–1725.
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the Third Report of the National Cholesterol Educaiton Program (NCEP) Expert Panel on Detection. JAMA. 2001;285(19):2486–2497.
- Garvey WT, Garber AJ, Mechanick JI, et al. The American Association of Clinical Endocrinologists and the American College of Endocrinology: 2014 advanced framework for a new diagnosis of obesity as a chronic disease. Endocr Pract. 2014;20(9):
977–989. - Rosenberg P, Urwitz H, Johannesson A, et al. Psoriasis patients with diabetes type 2 are at high risk of developing liver fibrosis during methotrexate treatment. J Hepatol. 2007;46(6):1111–1118.
- Amarapurkar D, Kamani P, Patel N, et al. Prevalence of non-alcoholic fatty liver disease: population based study. Ann Hepatol. 2007;6(3):161–163.
- Candia R, Ruiz A, Torres-Robles R, et al. Risk of non-alcoholic fatty liver disease in patients with psoriasis: a systemic review and meta-analysis. J Eur Acad Derm Ven. 2015;29(4):656–662.
- Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology. Gastroenterology. 2012;142(7):1592–1609.

