 J Clin Aesthet Dermatol. 2022;15(1):48–52.
J Clin Aesthet Dermatol. 2022;15(1):48–52.
by Bharathi Ravikumar, MD; Indradevi R, MD; and Dhivya Pillai, MD
All authors are with Mahatma Gandhi Medical College and Research Institute in Pondicherry, Pondicherry India.
FUNDING: No funding was provided for this study
DISCLOSURES: The author reports no conflicts of interest relevant to the content of this article.
ABSTRACT: Background. Acne is one of the most commonly faced dermatological complaints in our day-to-day practice. Among the various treatment modalities for acne and postacne pigmentation, chemical peeling is a promising and emerging treatment modality. Although various peeling agents are available, there is a lack of research comparing their efficacy. In addition, only a few studies have compared the efficacy of combined peels in the South Indian population. The present study aimed to compare the efficacy of alpha and beta hydroxy acid peels in the treatment of postacne pigmentation.
Methods: Forty patients with postacne pigmentation were divided into two groups of 20 patients each. Patients were randomized into one of the two treatment groups consecutively based on block randomization technique with block size 4. Patients of GA peel group was treated with 50% glycolic acid (GA) and the salicylic acid (SA) peel group was treated with 30% salicylic acid. The procedure was repeated every two weeks up to six weeks and the primary outcome was assessed every two weeks. The assessment with photographic documentation was done by a blinded evaluator from our department of dermatology.
Results: The mean age of the study population was 21±2.29 years. Out of 40 patients, 24 were females and 16 were males. GA and SA peel groups showed significant improvement from first follow-up onwards in the study. However, GA peel showed higher percentage of postacne pigmentation reduction than SA peel in all the four follow-ups. In GA peel group, >75% reduction in postacne pigmentation was observed in 45 percent of the patients. Whereas in the SA peel group, none of the patients achieved >75% reduction of postacne pigmentation. Pairwise comparison between both groups were statistically significant (P<0.0001)
Conclusion: Our results suggest that the GA peel was more effective than SA peel in improving postacne pigmentation.
Keywords: Cutaneous lesions, field cancerization, photosensitizing agent, protoporphyrin, lesion count
Acne vulgaris is an inflammatory multifactorial disease caused by hormonal, microbiological, and immunological factors. It affects various age groups, with teenagers being most common (85%) followed by 25 to 34 year-olds (8%) and 35 to 44 year-olds (3%).1 In recent meetings, the AAB has sought to address ways in which to improve assessment and management of postacne pigmentation, which is a prevalent problem in the Asian population.3
Chemical peeling is a popular, relatively inexpensive modality and also gives good therapeutic efficacy which is performed in dermatology out-patient procedure in the treatment of active acne lesions, postacne hyperpigmentation, and to refresh and rejuvenate skin. A wide range of peels is available with different mechanisms of action, which can be modulated by altering concentrations. Today, the most common agents used for postacne pigmentation among alpha hydroxy acids (AHA) is glycolic acid (GA), and beta hydroxy acids (BHA), is salicylic acid (SA).4
Many studies have previously been conducted by using chemical peeling as a treatment for active acne lesions only or for acne scars and pigmentation. There are few studies on postacne pigmentation through chemical peeling combined with laser or topical medication. There is no report on the efficacy of chemical peeling alone to treat postacne pigmentation. The present study aimed to compare the efficacy of alpha and beta hydroxy acid peels in the treatment of postacne pigmentation.
Methods
Study population and design. This double-blinded randomized control trial was conducted in the department of DVL OPD over a period of 18 months from May 2019 to October 2020. This study was approved by the Institutional ethics committee and was registered in Clinical Trials Registry (India Reg no.CTRI/2019/05/019315). Based on the prevalence in previous studies, hospital records, and considering a dropout rate of 10 percent, the sample size was taken as 20 patients for each group, a total of 40 patients.
All consecutive consenting patients irrespective of age and sex presenting with postacne pigmentation were included in the study. Pregnant and lactating women, female patients using oral contraceptives, patients with active herpes simplex infection or active acne lesions, patients with a history of keloidal tendency (i.e., any history of vaccination/surgery-induced scars), patients who could not adhere to the follow-up schedule, and patients with unrealistic expectations were excluded from the study.
Study protocol. All patients with postacne pigmentation were screened for eligibility and enrolled after providing informed written consent. We allocated patients using computer-generated random sequence to a glycolic acid group and a salicylic acid group. The intervention was carried out by the dermatology resident and the chemical peel which is selected for the procedure was not informed either to the observer (consultant from the DVL department) or to the patient. Finally, Physician’s Global Assessment (PGA) scores were calculated, and digital photographs using the same positioning, lighting, and camera settings in all cases were taken.
Treatment procedure. Initially, the patient’s face was prepared by cleansing. After masking the eye, a chemical peel was applied to respective patients over the pigmented areas with a help of a thin brush. After the endpoint was observed (i.e., pseudofrosting, a white precipitate) in case of salicylic acid and after applying neutralizer 3 to 5 minutes later in case of glycolic acid, patients were advised to rinse the face with water and apply ice packs if any erythema was present. After the procedure, photographs were taken and sunscreen was applied all over the face. They were advised to prevent unnecessary sun exposure. The patient was also advised to abstain from any cosmetic procedures during the study period. The same procedure was repeated for three more sessions with an interval of two weeks for a total period of six weeks.
Evaluation and follow-up. The evaluation of each patient by a blinded dermatologist was performed by PGA score calculation and the assessment of standardized digital photographs taken at baseline, each treatment session, at the end of treatment, and finally at the end of the follow-up period. Physician’s Global Assessment (PGA) based on clinical and photographic records were scored as a good response if more than 50-percent improvement, moderate response if 25 to 50-percent improvement and poor response if less than 25-percent improvement. Documentation of side effects was done during every session by asking the patient if there was any discomfort that had appeared since the last session and noticing whether it was still present.
Statistical analyses. Statistical analyses were performed with SPSS version 22.0 (IBM SPSS, US) software. Baseline categorical variables were exhibited as percentages and the continuous variables were exhibited as mean ± standard deviation.The statistical significance of mean differences was compared using an unpaired t-test. All values were considered significant if the P-value was <0.05. All data obtained were entered into a Data collection proforma sheet (Annexure 10.1) and digital master sheet (Annexure 10.5), using Microsoft Excel (MS Excel 2010)
Results
Baseline characteristics of the study population were described in Table 1. A total number of 40 patients age ranged from 18 to 26 years were enrolled in the present study. The mean age was 21±2.29 years. Out of 40 study patients, 16 (40%) were male and 24 (60%) were female. In the present study maximum of 55 percent of patients presented with pigmentation over the cheeks followed by 40 percent of patients having pigmentation all over the face. Only five percent of patients had pigmentation on forehead and cheeks. Fifty percent of the study population underwent treatment for pigmentation previously and 50 percent did not take any treatment for the same. Two patients had side effects due to the chemical peel therapy observed in the present study.
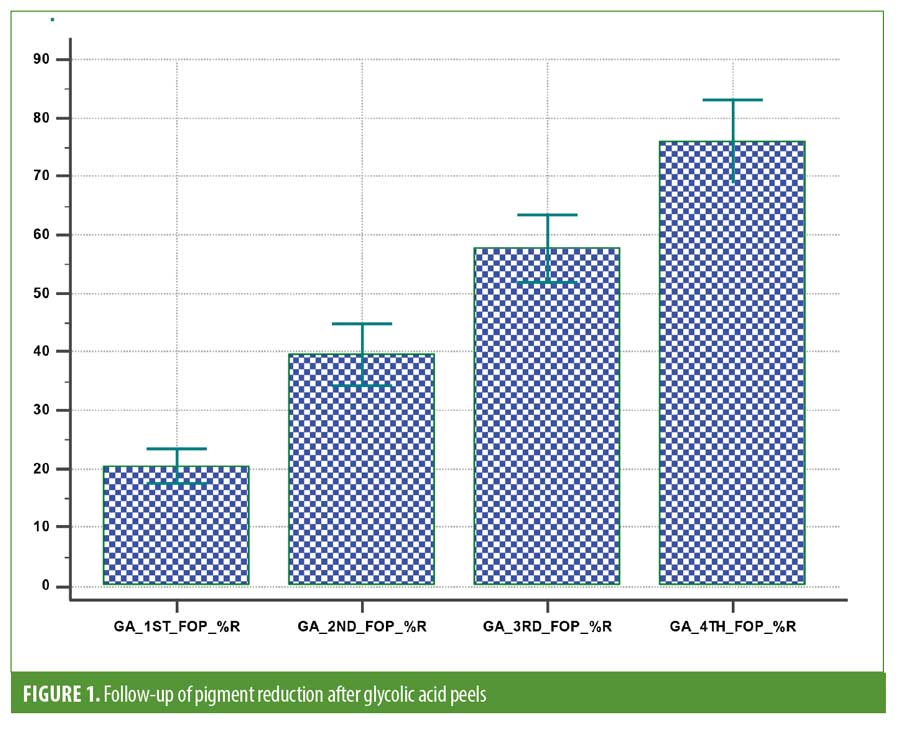
GA peel group. In this group, the patient’s age ranged from 18 to 25 years, and the mean age was 21.1±2.29 years. Out of 20 patients, 60 percent were female and 40 percent were male participants. In this group, one patient had erythema as the side effect of GA peel. Except this, none of the patients observed the side effects. The present study had four regular follow-ups to look at the progress of the treatment (percentage of reduction of pigmentation). The first follow-up was compared with another three follow-ups to describe the percentage of pigmentation reduction due to GA peel. Within this group, significant improvement was observed in all the follow-up periods constantly (Figure 1).
SA peel group. In this group, the patient’s age ranged from 18 to 26 years, and the mean age was 20.9±2.35 years . Out of 20 patients, 60 percent were female and 40 percent were male. In this group, one patient had burning sensation as the side effect of SA peel. Otherwise, none of the patients reported any other side effects. The present study had four regular follow-ups to look at the progress of the treatment (percentage of reduction of pigmentation). The first follow-up was compared with another three follow-ups to describe the percentage of pigmentation reduction due to SA peel. Within this group, significant improvement was observed in all the follow-up periods constantly (Figure 2).
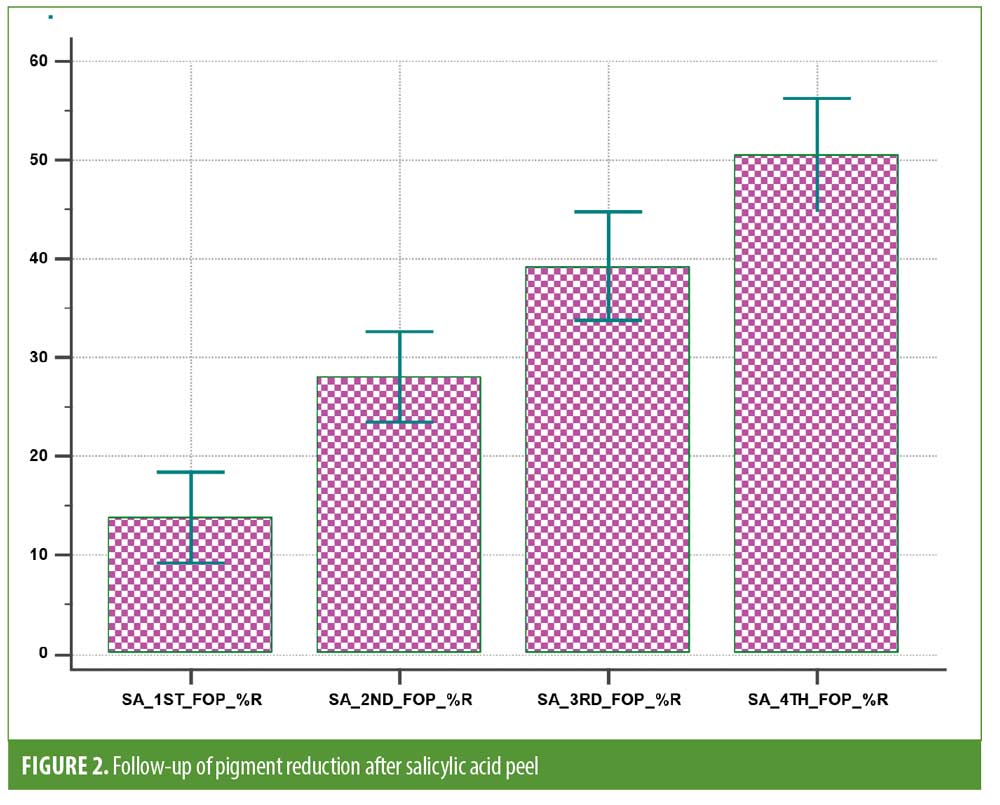
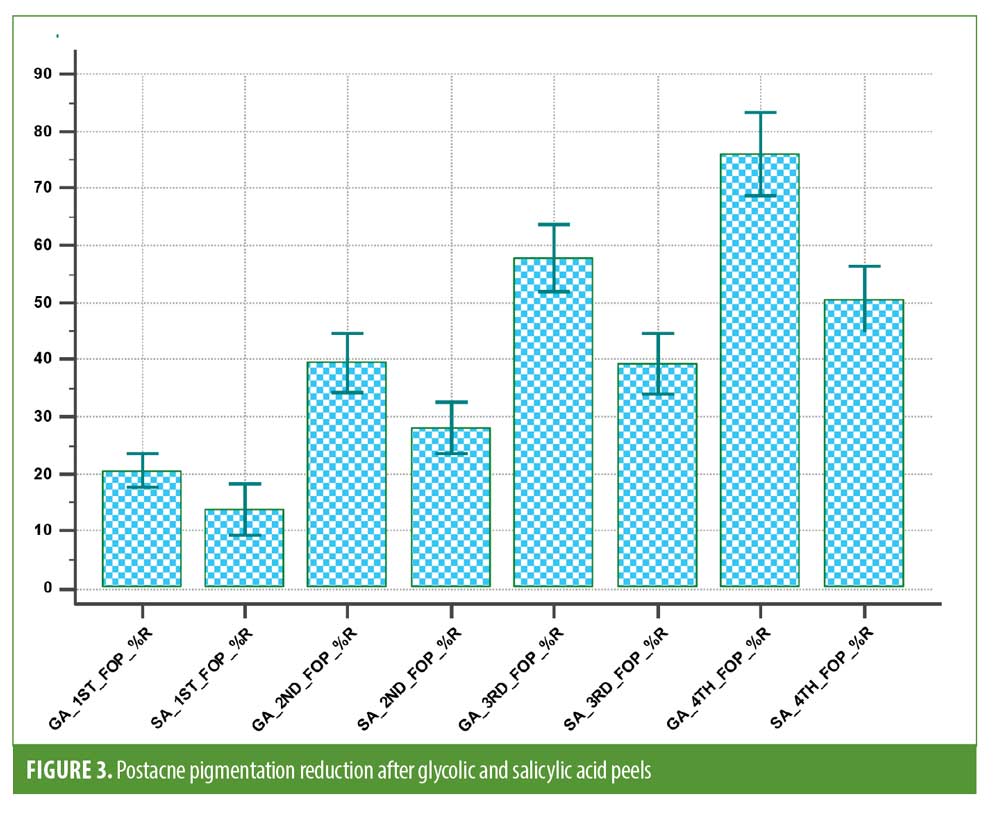
Comparison of GA and SA chemical peel efficacy on postacne pigmentation. The efficacy of both GA and SA chemical peel was analyzed (Table 2). The GA peel showed excellent outcomes in terms of reduction of postacne pigmentation than SA chemical peel. In all the four follow-ups, GA peel had shown significant improvement compred to the SA peel. In the first follow-up, GA peel was reduced by about 20 percent of the pigmentation than SA peel (13%) (P=0.0137). During the second follow-up, in both the groups, the reduction was one-fold higher than the first follow-up. However, the GA peel group showed a higher percentage than the SA peel group (P=0.0013). In third and fourth follow-up were dramatically improved in the GA peel group than SA peel group. The reduction of pigmentation was about 75 percent in the fourth follow-up in the GA peel group whereas participants in the SA peel group achieved 50-percent reduction (Figure 3). During these two follow-up periods, GA peel showed a higher statistical significance than the SA peel group (P<0.0001)
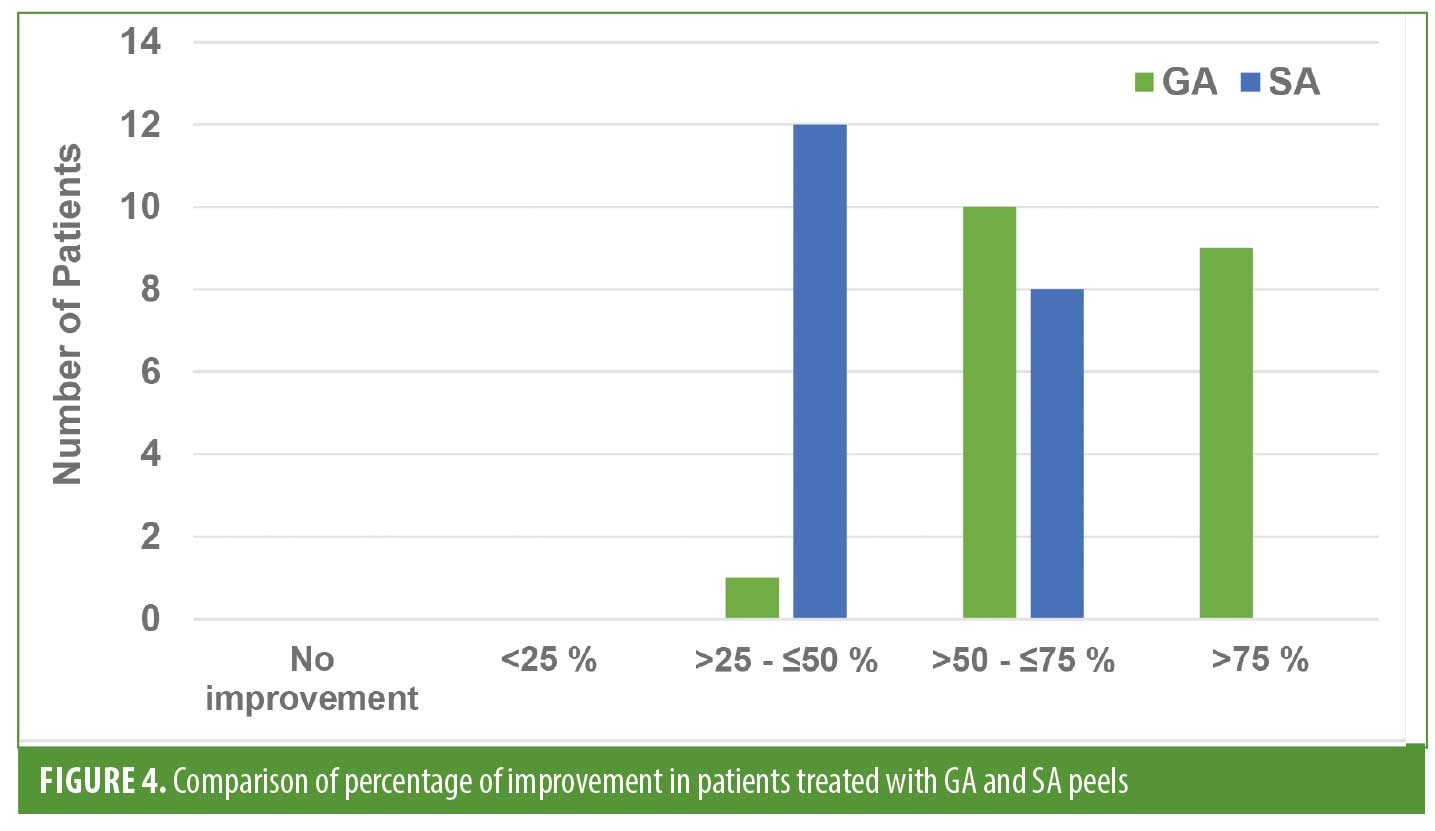
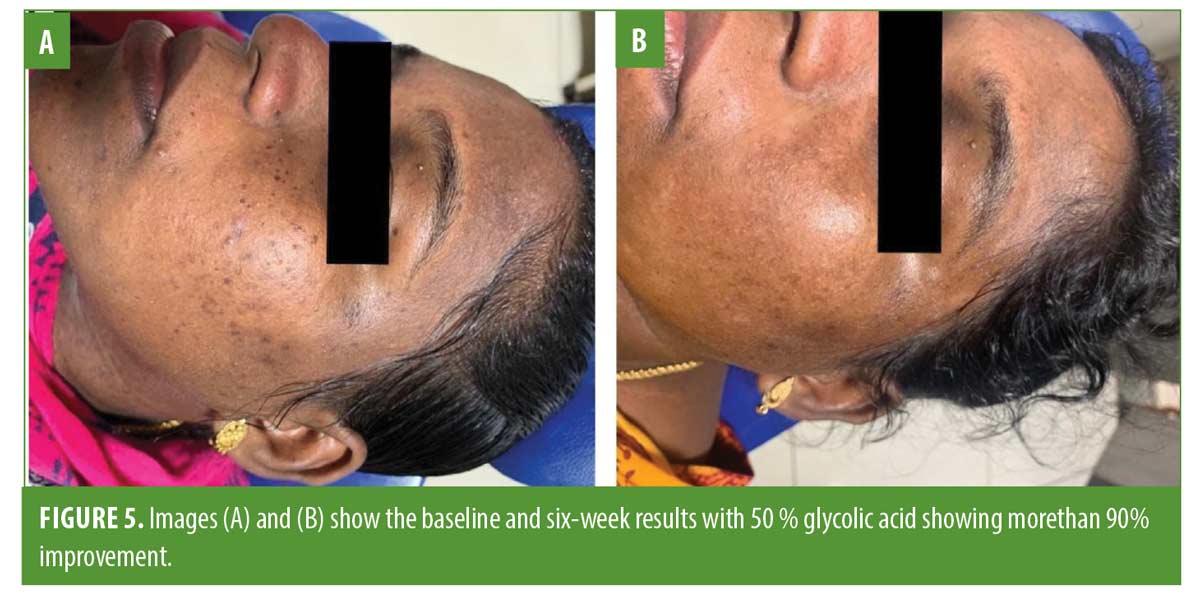
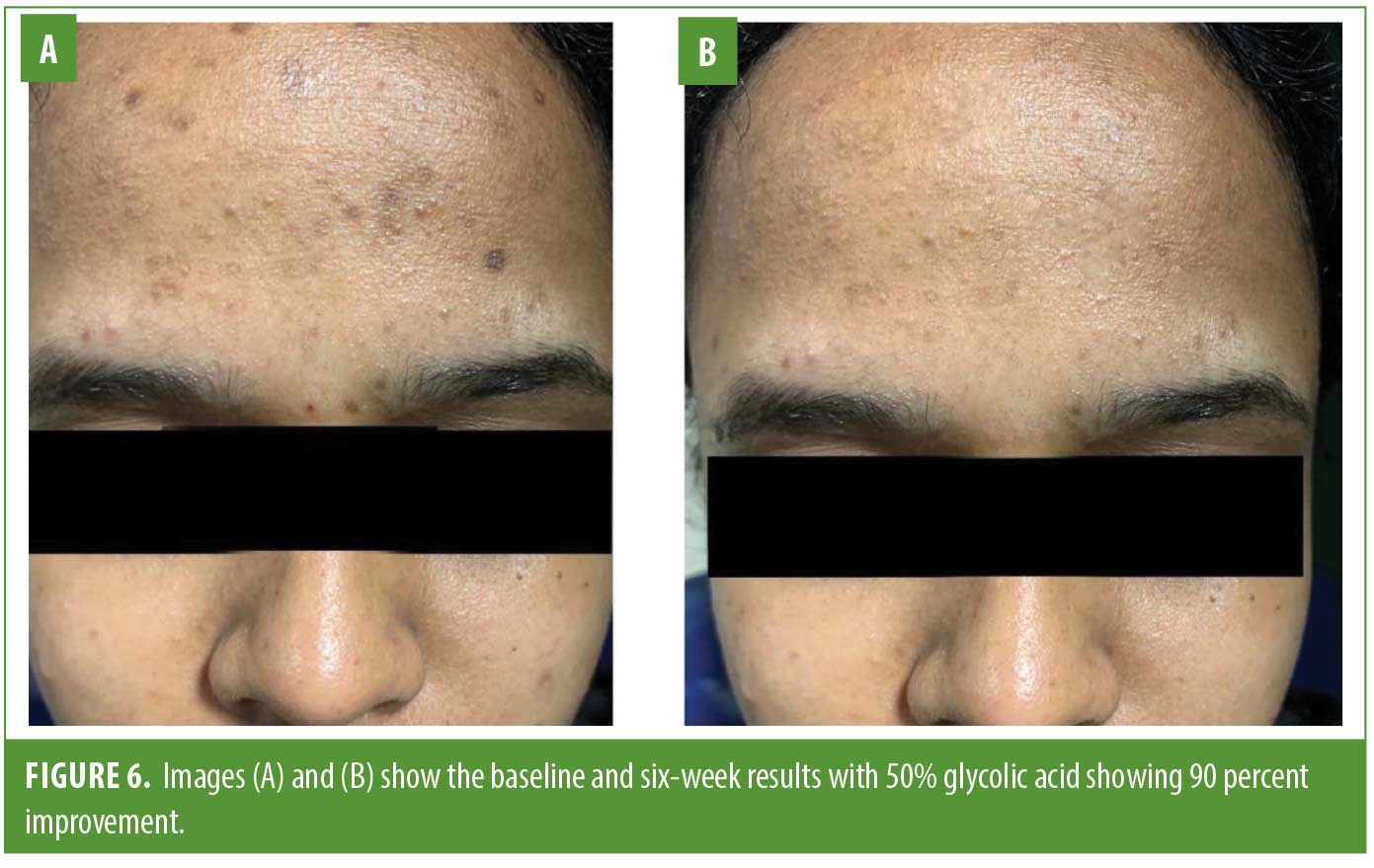
Comparison of percentage of pigmentation reduction. In the GA peel group, nine patients1 had reduced their postacne pigmentation >75 %. In the SA peel group, none of the patients were improved more than 75 percent pigment reduction. Similarly, >50 to ?75-percent reduction was higher in GA peel group than SA peel group (Figure 4). Figures 5, 6 and 7 present some clinical photographs of patients in both groups.

Discussion
This study compared the efficacy of alpha and beta hydroxy acid peel in the treatment of postacne pigmentation. The results showed a significant improvement from the first follow-up onwards in both groups. However, GA peel showed a higher percentage of postacne pigmentation reduction than SA peel in all four follow-ups and was statistically significant.
Choosing the appropriate depth of the chemical peel is an important component for the best outcome. Superficial peels like 50% glycolic acid and 35% salicylic acid were selected in this study as they affect the epidermis and dermal-epidermal junction. Also owing to its superficial action, superficial peels can be used in nearly all skin types.
Both glycolic acid and salicylic acid peels help in managing postacne pigmentation in their unique ways. In GA peel the epidermis of pigment cells is decomposed, and then the cells with reduced pigment are epithelialized.5,6 Whereas in SA peel the self-precipitation effect of the peeling agent is not easy to penetrate and has good safety, so it reduces the risk of pigmentation after peeling.7,8
Many studies have compared glycolic acid with other peels where they found GA peel showing better results. Kim et al9 evaluated GA in patients with moderate acne, whereas two other studies compared it with other peeling agents such as Jessner’s solution and a blend of SA and mandelic acid (MA). In that study, the initial results were not satisfactory, but after several peels, most of the acne and inflammatory lesions were better improved. In a randomized trial, 70 percent of GA was compared with JS, and it was observed that both peeling agents were effective in reducing acne scores. However, the peeling time on the side treated with JS is longer, which is problematic for some patients. Therefore, for this reason, more patients prefer GA to JS. The present study results also coincide with the above-mentioned studies that in the GA peel group, the postacne pigmentation was significantly reduced.
In another study by Burns et al,10 dark-skinned patients who received glycolic acid chemical peels showed rapid and greater improvement compared with the control group. In addition, the latest study by Sarkar et al11 compared the safety and effectiveness of GA peel in combination with a modified Kligman formula (MKF), which contains 2% hydroquinone, 0.05% vitamin D formic acid, and hydrogenated cortisone 1, where using GA with MKF showed a better improvement than MKF alone. In our study, significant improvement was noted in GA peel after the first session in the postacne hyperpigmentation.
Similarly few studies have compared salicylic acid with other peels where SA peel showed a better efficacy. A double-blind, split-face RCT by Kessler et al12 where they compared 30 percent GA with 30 percent SA for mild to moderate acne vulgaris among 20 patients. Eventhough the two peels showed no significant differences, the SA peel had sustained effectiveness and had fewer side effects.
Studies have also shown the beneficial effects of salicylic acid peels on pigmentation in dark-skinned individuals.13 Salicylic acid reduces postacne pigmentation through its anti-inflammatory effects. In a study, 20 percent to 30 percent of SA peel was compared with 0.1% topical retinoic acid solution between three groups. In the first and second groups, SA peel and retinoid were used alone respectively whereas both were used in the third group. Compared to groups 1 and 2, the combination therapy (third group) had a significantly better effect.14 Similarly a study by Ahn and Kim15 found that salicylic acid also has a whitening effect on the skin. However, the present study results were observed contradictory results of the above-mentioned studies as the GA peel showed significant improvement on postacne pigmentation than the SA peel. As the different ethnicities may respond uncertainly to chemical peeling nonetheless of skin phenotype could be the reason for these conflicting results.
Conclusion
In summary, both glycolic and salicylic acid peels were shown to be effective in the treatment of postacne pigmentation. However, the GA peel was highly efficient than the SA peel and considered a superior peel. It appears to be a promising chemical agent in treating postacne pigmentation which is cost-effective compared to other interventional procedures and overcomes the abuse of hydroquinone and steroid preparations by the patients which have their array of side effects.
References
- Skroza N, Tolino E, Mambrin A, Zuber S, Balduzzi V, Marchesiello A, Bernardini N, Proietti I, Potenza C. Adult acne versus adolescent acne: a retrospective study of 1,167 patients. The Journal of clinical and aesthetic dermatology. 2018 Jan;11(1):21.
- Zaenglein AL, Thiboutot DM. Acne Vulgaris. Bolognia JL, Jorizzo JL, Schaffer JV. Dermatology, 3rd ed., China: Elsevier Saunders. 2012;36:545-60.
- Woolery-Lloyd H, Kammer JN. Treatment of hyperpigmentation. Semin Cutan Med Surg 2011; 30: 171–175
- Kornhauser A, Coelho SG, Hearing VJ. Applications of hydroxy acids: classification, mechanisms, and photoactivity. Clinical, cosmetic and investigational dermatology: CCID. 2010;3:135.
- Handog EB, Datuin MS, Singzon IA. Chemical peels for acne and acne scars in Asians: evidence based review. J Cutan Aesthet Surg 2012;5:239-46.
- Sharad J. Glycolic acid peel therapy—a current review.Clin.Cosmet. Investig. Dermatol. 2013;6: 281–8
- Arif T. Salicylic acid as a peeling agent: a comprehensive review. Clinical, cosmetic and investigational dermatology. 2015;8:455.
- Dayal S, Sahu P, Sangal B, Sharma S. Role of chemical peels in postinflammatory hyperpigmentation: a comprehensive review. Pigment Int 2019;6:59-66
- Kim SW, Moon SE, Kim JA, Eun HC. Glycolic acid versus Jessner’s solution: Which is better for facial acne patients? A randomized prospective clinical trial of split-face model therapy. Dermatol Surg. 1999;25:270–3.
- Burns RL, Prevost-Blank PL, Lawry MA, Lawry TB, Faria DT, Fivenson DP. Glycolic acid peels for postinflammatory hyperpigmentation in black patients. A comparative study. Dermatol Surg 1997;23:171-4; discussion 175.
- Sarkar R, Parmar NV, Kapoor S. Treatment of postinflammatory hyperpigmentation with a combination of glycolic acid peels and a topical regimen in dark-skinned patients: a comparative study. Dermatol Surg 2017;43:566-73.
- Kessler E, Flanagan K, Chia C, Rogers C, ANNA GLASER DE. Comparison of ?-and ?-Hydroxy Acid Chemical Peels in the Treatment of Mild to Moderately Severe Facial Acne Vulgaris. Dermatologic surgery. 2008 Jan;34(1):45-51.
- Joshi SS, Boone SL, Alam M, Yoo S, White L, Rademaker A, et al. Effectiveness, safety, and effect on quality of life of topical salicylic acid peels for treatment of postinflammatory hyperpigmentation in dark skin. Dermatol Surg 2009;35:638-44.
- Ali BMM, Gheida SF, Mahdy NAE, Sadek SN. Evaluation of salicylic acid peeling in comparison with topical tretinoin in the treatment of postinflammatory hyperpigmentation. J Cosmet Dermatol 2016;16:52-6.
- Ahn HH, Kim IH. Whitening effect of salicylic acid peels in Asian patients. Dermatol Surg 2006;32:372-5

