 J Clin Aesthet Dermatol. 2020;13(12):E53–E55
J Clin Aesthet Dermatol. 2020;13(12):E53–E55
by Jihan Muhaidat, MD; Firas Al-Qarqaz, MD; and Diala Alshiyab, MD
All authors are with the Department of Dermatology, Faculty of Medicine at Jordan University of Science and Technology in Irbid, Jordan.
FUNDING: No funding was provided.
DISCLOSURES: The authors declare no conflicts of interest related to the content of this article.
ABSTRACT: Scleredema is an idiopathic condition with specific clincopathological findings, including symmetrical and diffuse nonpitting induration of the upper body and thickened dermis due to deposition of acid mucopolysaccharides. Here, we report a case of linear scleredema in a healthy female patient, who presented with firm induration of the skin over her right shoulder and arm in a Blaschkolinear distribution. The onset was insidious in childhood and stable over several years. While the clinical picture has closely mimicked linear morphea, the diagnosis of scleredema was confirmed by the typical histopathological findings. To the best of our knowledge, linear scleredema is a unique presentation that has not been previously reported.
KEYWORDS: Scleredema, linear, Blaschko’s lines
Scleredema is a cutaneous sclerosing disorder that affects all age groups. It is usually differentiated by its characteristic clinical features, particularly its predilection to central and upper body parts, including the neck, upper trunk, face, and the proximal upper extremities, with classical sparing of the hands and feet. It’s generally described as symmetrical and diffuse. The histopathological findings are diagnostic and include a normal epidermis and thickened dermis up to four times the normal, due to mucin deposition between edematous nonsclerotic collagen bundles.1–4
The first description of scleredema adultorum dates back to 1902. Since then, several cases have been described in the literature. In 1968, scleredema was classified into the three main groups according to the age of onset and associated or preceding illnesses. Type 1 has an abrupt onset in children, usually triggered by febrile illness, and resolves gradually within a few months up to two years. Type 2 affects adults, with a female preponderance of 2:1. The onset is insidious and the course is prolonged; it is associated with paraproteinemia. Type 3 also has an insidious onset and protracted course. It is often seen in adult male patients with poorly controlled diabetes mellitus.1–3 While all types differ in course and prognosis, they essentially share the same clinical features and histological findings.
Here, we present a case of unilateral linear scleredema. To our knowledge, the distribution of this disease along the Blaschko’s lines has not been previously reported.
Case Report
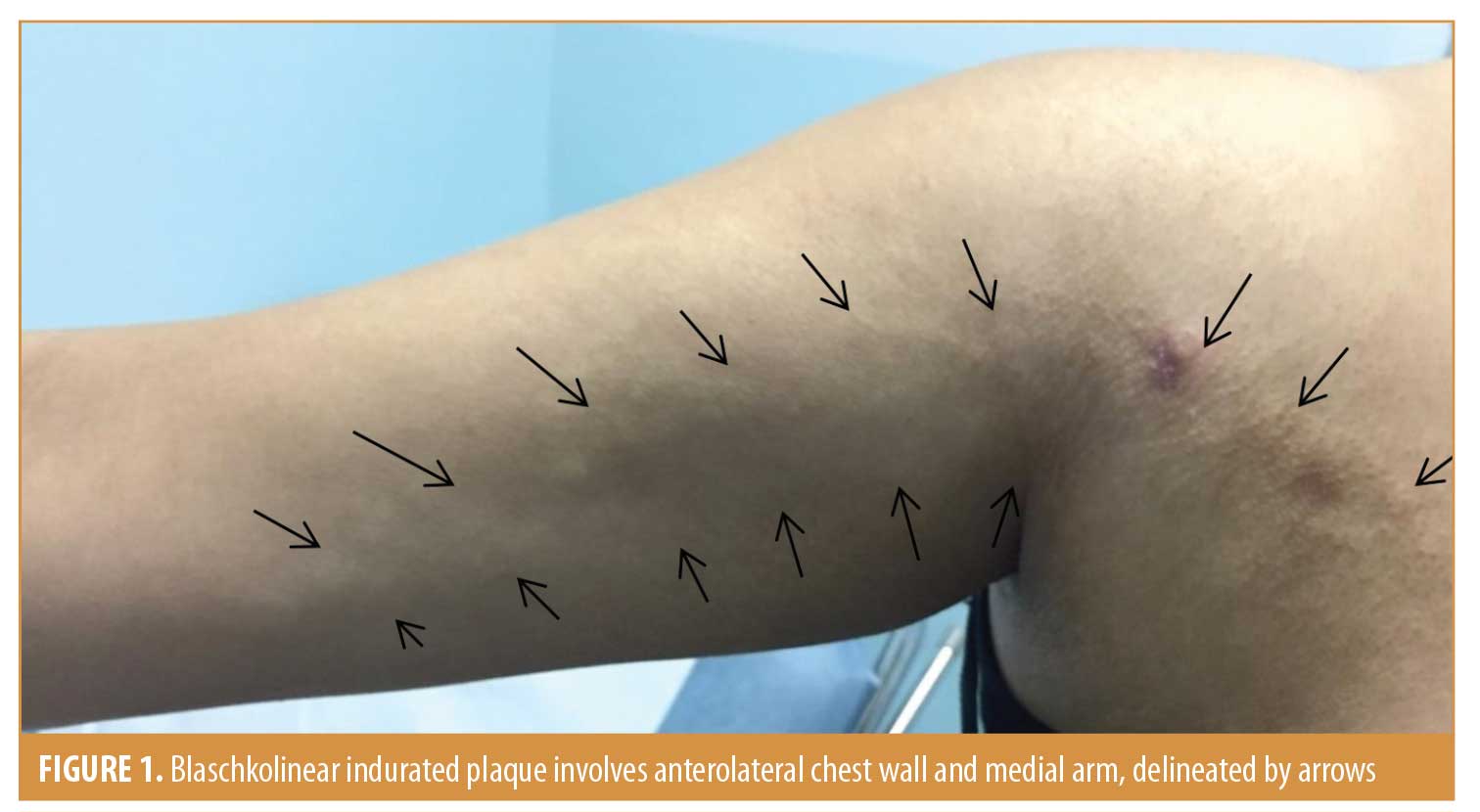
A 22-year-old otherwise healthy female patient presented with an asymptomatic streak of hard textured skin over her right shoulder and arm. The patient reported having the condition for 14 years. The onset was insidious in childhood and stable over several years. The patient nor her parents could recall any particular preceding illness or trauma. The patient was otherwise healthy and no family members reported having the same condition. The induration had reportedly been almost the same size and distribution since it was first noticed. There was no history of Raynaud’s phenomena nor restriction in the movement of the shoulder. The indurated skin followed a Blaschkolinear distribution and extended over the right upper chest wall and shoulder and down the medial aspect of the arm. It ended proximal to the antecubital fossa. The margins were distinct by palpation but not by inspection. The overlying skin was slightly dyspigmented with follicular prominence (Figure 1).
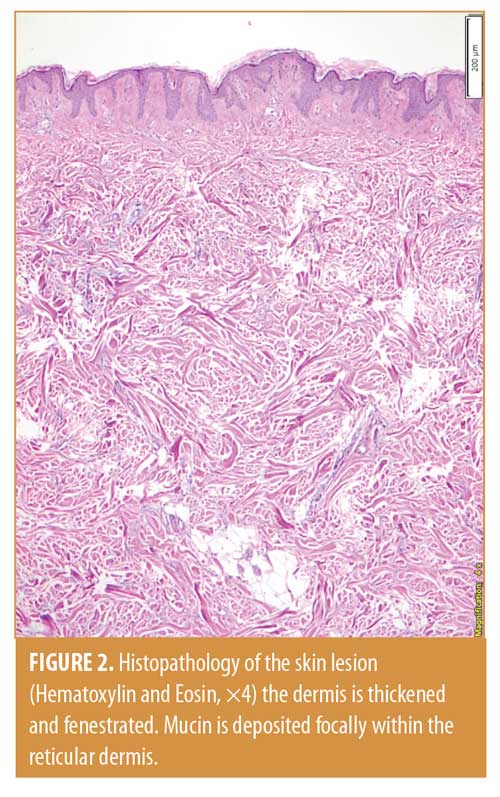
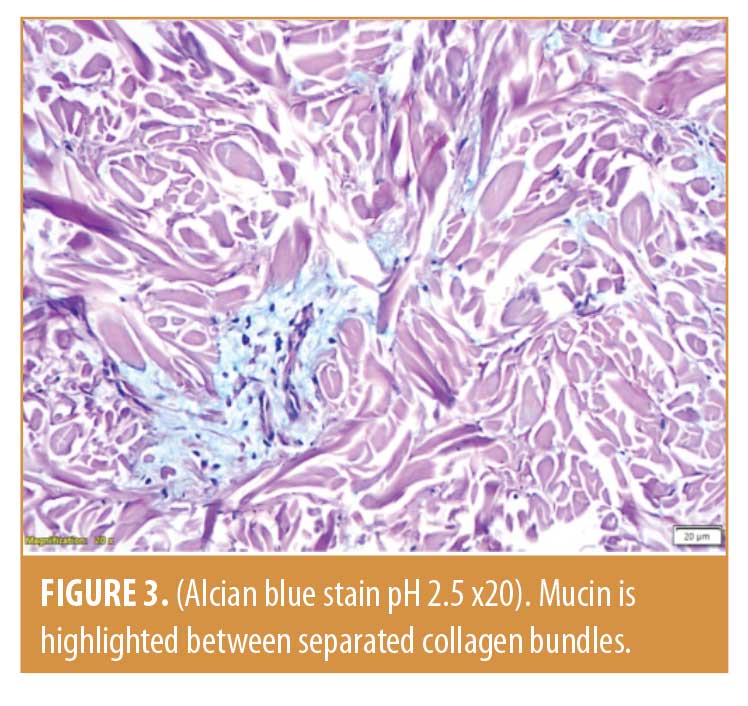
Full range of movement of the right shoulder was observed and no discrepancy in the diameter of the arms was noted. Ultrasonography examination of the affected area confirmed diffuse thickening without evidence of soft tissue masses. There was a difference in thickness of nearly 11mm between the right lateral side of the chest wall compared to the contralateral left side. Skin biopsy sections had shown a normal epidermis. The dermis was thickened with edematous collagen bundles that were separated with clear spaces. Mucin was present focally in the reticular dermis. The collagen bundles were not sclerotic, and the appendages were preserved. No inflammatory cells were seen, and the number of fibroblasts was not increased (Figure 2). Mucin was also highlighted by Alcian blue stain (pH2.5) (Figure 3).
Elastic fibers were mildly fragmented in the mid dermis as demonstrated by Verhoeff-Van Gieson stain. The patient was diagnosed with linear scleredma. The following investigations were ordered and were either normal or negative: complete blood count, blood glucose, glycosylated hemoglobin(Hb A1c), urinalysis, thyroid function tests, serum protein electrophoresis and immunnoserology (anti-nuclear antibody, extractable nuclear antigen antibody screen, double stranded deoxyribonucleic acid [DNA] antibodies). The patient used potent topical steroids for one month without any softening of her skin, and she refused any further treatment options due to lack of demonstrated efficacy.
Discussion
The causes of skin induration are various, and diagnosis can be challenging. The site and distribution are among factors that provide helpful clues to the underlying disease, but unusual sites of involvement can hinder a correct diagnosis.
Our case represents a unique presentation of scleredema as a unilateral Blaschkolinear distribution over the upper extremity. In fact, the diagnosis of scleredema was not suspected clinically and, considering the disease onset during childhood, the patient was initially thought to have linear morphea. However, unlike linear morphea, there was no lilac border of the overlying skin, no deep tissue involvement (as demonstrated by full range of movement), and the induration had been constant without amelioration.5 The diagnosis could not be confirmed without considering the histological features, which were consistent with a scleredema diagnosis and ruled out the diagnosis of morphea, as there were no sclerosis or inflammation and the appendages were intact.
A review of the literature for unusual presentation of scleredema revealed few cases. We categorized them into two groups. The first group comprised patients with classical scleredema that was more pronounced or extended to unusual sites. This included three patients with diabetes and prominent periorbital swelling, three postinfectious cases with hand and finger involvement, and one case of frontal scalp nonscarring alopecia in a child.2,4,6–10 Involvement of the genitals was only reported in two cases with widespread disease.4,11
The second group comprised patients who presented with scleredema that was confined to an unusual site. Establishing the diagnosis in these cases was understandably challenging. This group included a child with scleredema confined to the scalp, upper face, and periorbital area, a male patient with progressive periorbital swelling, a patient with unilateral periorbital swelling, a patient with diabetes and scleredma limited to thighs, and a pregnant woman with induration of the lower abdomen and proximal thighs.12–16
Asymmetry is not a common feature of scleredma; we found reports of four patients who were described with asymmetrical disease. This included one patient out of a total of 44 patients who were included in a multicenter study3 and three children who were reported to have asymmetrical scleredma that involved one side of the trunk and/or lower limb in a diffuse pattern that was associated with abnormal gait.17,18 Interestingly, two of the children had mixed features of stiff skin syndrome.
Conclusion
We presented a unique presentation of scleredma in a unilateral Blaschkolinear distribution of the upper extremities. We assert this could be considered a separate subtype of scleredema. We suggest scleredema to be included in the differential diagnosis of any woody, nonpitting induration of the skin, including those with a linear distribution.
References
- Knobler R, Moinzadeh P, Hunzelmann N, et al. European dermatology forum S1 guideline on the diagnosis and treatment of sclerosing diseases of the skin, Part 2: Scleromyxedema, scleredema and nephrogenic systemic fibrosis. J Eur Acad Dermatol Venereol. 2017; 31(10):1581–1594.
- Venencie PY, Powell FC, Su WP, Perry HO. Scleredema: a review of thirty-three cases. J Am Acad Dermatol. 1984;11(1):128–134.
- Rongioletti F, Kaiser F, Cinotti E, et al. Scleredema. A multicentre study of characteristics, comorbidities, course and therapy in 44 patients. J Eur Acad Dermatol Venereol. 2015;29(12):2399–2404.
- Curtis AC, Shulak BM. Scleredema adultorum: Not always a benign self-limited disease. Arch Dermatol. 1965;92(5):526–541.
- Kunzler E, Florez-Pollack S, Teske N, et al. Linear morphea: Clinical characteristics, disease course, and treatment of the morphea in adults and children cohort. J Am Acad Dermatol. 2019;80(6):1664–1670.
- Chatterjee S. Neck pain, stiffness, and periorbital edema in a man with diabetes. JAMA. 2016;315(11):1159–1160.
- Mohamed M, Belhadjali H, Béchir AB, et al. Scleredema adultorum of Buschke with prominent periorbital edema in a Tunisian patient with diabetes mellitus: a case report. Int J Dermatol. 2016;55(2):e100–102.
- Fania L, Colonna L, Pagnanelli G, et al. Scleredema of Buschke with prominent periorbital edema. Int J Dermatol. 2017;56(10):e193–194.
- Lewis CM, Sanchez AT, Davis LS. Atypical scleredema involving the hands in an adolescent. Pediatr Dermatol. 2016;33(6):e342–343.
- Singal A, Gandhi V, Bhattacharya SN. Scleredema adultorum of buschke associated with non-scarring alopecia of scalp. Indian J Dermatol Venereol Leprol. 1999; 65(1):38–39.
- Paz RA, Badra RE, Marti HM, Maxit MJ. Systemic Buschke’s scleredema with cardiomyopathy, monoclonal IgG kappa gammopathy and amyloidosis. Case report with autopsy. Medicina. 1998;58(5 Pt 1):501–503.
- Burke MJ, Seguin J, Bove KE. Scleredema: an unusual presentation with edema limited to scalp, upper face, and orbits. J Pediatr. 1982;101(6):960–963.
- Ioannidou DI, Krasagakis K, Stefanidou MP, et al. Scleredema adultorum of Buschke presenting as periorbital edema: a diagnostic challenge. J Am Acad Dermatol. 2005;52(2 Suppl 1):41–44.
- Jung JY, Ryu DJ, Chung KY, Kwon YS. Scleredema presenting as unilateral periorbital edema. J Am Acad Dermatol 2009;60(3): AB51–AB51.
- Farrell AM, Branfoot AC, Moss J, et al. Scleredema diabeticorum of Buschke confined to the thighs. Br J Dermatol. 1996;134(6):1113–1115.
- Vinod CS, Ambika H, Ambika H, et al. Scleredema adultorum of Buschke over an unusual site associated with pregnancy. Indian Dermatol Online J. 2014;5(4):466–468.
- Morrell DS, Challgren E, Nijhawan A, et al. Two cases for diagnosis: asymmetric childhood scleredema or stiff skin syndrome? Pediatr Dermatol. 2003;20(4):350–355.
- Galan-Gutierrez M, Ruiz-Villaverde R, Márquez-Lobo B, et al. Asymmetric childhood scleredema. Eur J Dermatol. 2012;22(1): 127–128.

