 by Brooke E. Vasicek, MD; Susanna M. Szpunar, PhD; and Lisa A. Manz-DUlac, MD
by Brooke E. Vasicek, MD; Susanna M. Szpunar, PhD; and Lisa A. Manz-DUlac, MD
Dr. Vasicek is with the Transitional Year Residency Program at St. John Hospital and Medical Center in Detroit, Michigan. Dr. Szpunar is with the Department of Graduate Medical Education at St. John Hospital and Medical Center.
Dr. Manz-Dulac is with Eastside Dermatology in Grosse Pointe Woods, Michigan.
Funding: No funding was provided for this study.
Disclosures: The authors have no conflicts of interest relevant to the content of this article.
Abstract: Background. Skin cancer and photodamage are problems commonly addressed by dermatologists. Despite the opportunities for chemoprevention with broad-spectrum sunscreen, there is little research investigating patient knowledge of proper sunscreen guidelines, or patient perception of physician counseling.
Objective. The author sought to determine patient knowledge of the American Academy of Dermatology guidelines for proper sunscreen use and to obtain patient-reported rates of physician counseling regarding sunscreen.
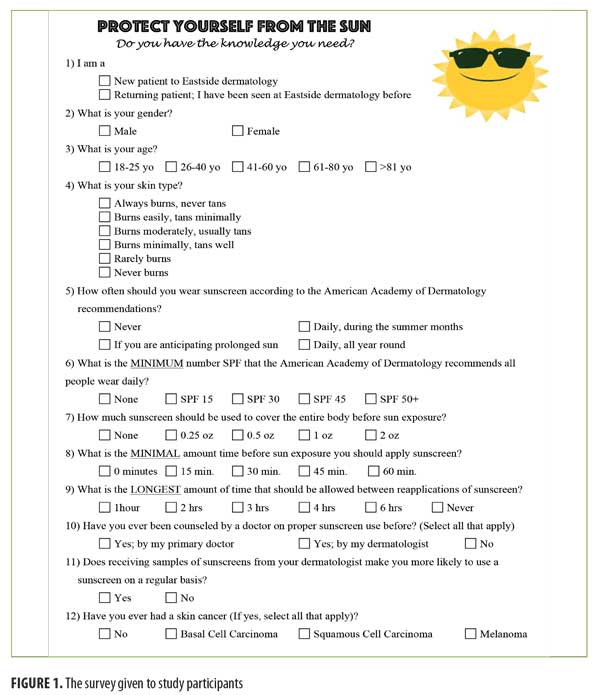
Design. We used a 12-question, multiple choice, anonymous survey to collect data.
Setting. The study setting was a private dermatology clinic near Detroit, Michigan.
Participants. Two hundred ninety- four adult patients presenting for routine office visits were included in the study.
Results. About 59 percent of the subjects selected the recommended frequency of proper sunscreen use and 60 percent selected the recommended minimum sun protection factor. The minimum amount of sunscreen to cover the body, time of application before sun exposure, and time between reapplications of sunscreen did not receive a majority response. Differences in knowledge were seen between the sexes and skin types. Forty-four percent of patients previously received sunscreen counseling. Patients older than 40 years of age (39.3% vs. 18.4%, p=0.04), those who were fair skinned (62.5% vs. 23.8%), established patients (40.7% vs. 8.3%, p<0.0001), and those with a skin cancer (58.3% vs. 28%, p<0.0001) were more likely to report previous counseling.
Conclusions. The majority of the study subjects never received counseling and lacked adequate knowledge of sunscreen guidelines. In order to obtain adequate primary prevention of skin cancer, it is essential to provide patients with further counseling and education on proper sunscreen use.
Keywords: Sunscreen, broad spectrum, photoprotection, sun protection factor, patient education, prevention, skin cancer
J Clin Aesthet Dermatol. 2018;11(1):35–40
Introduction
Ultraviolet radiation (UVR) has many acute and chronic harmful effects on the skin.1 It is a modifiable risk factor for the development of skin cancers, such as squamous cell carcinoma (SCC), basal cell carcinoma (BCC), and melanoma, and is associated with 90 percent of all BCCs and SCCs.1–5 Skin cancer is the most common cancer in the United States, affecting one in five adults during their lifetime.4–7 The incidence of BCC and SCC is higher than that of breast, prostate, and colon cancers combined.4,6,8 Despite well-established interventions to decrease UVR, the incidence of skin cancer has been rising for decades, while the incidence of many other cancers has been steadily decreasing.5 Skin cancer poses a significant burden to health care resources, costing $8.1 billion dollars annually.9
Melanoma is the deadliest form of skin cancer, and its incidence has doubled over the last 30 years.5,8,10 Ultraviolet (UV) exposure is positively correlated with melanoma risk and is currently one of the only known modifiable risk factors.5,10,11 Advanced melanoma is difficult to treat and carries a poor prognosis, making prevention of melanoma imperative. Broad-spectrum sunscreen use is currently the only data-supported method for the prevention of melanoma.10
Exposure to UVR can be effectively limited through avoidance. Avoidance can be achieved through the use of UVB- and UVA-blocking glass, the employment of tightly woven, darkly colored or UV-protection-factor-rated fabric, and the application of sunscreens.5,12,13 Only about 30 percent of adults routinely follow such photoprotective behaviors, resulting in approximately 35 percent of adults and 69 percent of children in the United States experiencing sunburn each year.14 Patients rely upon physicians to provide preventive counseling that will minimize high-risk behaviors. Great variation is reported in the literature on how frequently this counseling occurs, with 1.6 to 58 percent of dermatologists discussing sunscreen use with patients at office visits.15,16 The data on the extent of this counseling are also limited. Often, only the recommended number of sun protection factor (SPF) is addressed, although this is only one of the many sunscreen recommendations put forth by the American Academy of Dermatology (AAD).15,17 In addition to dermatologists, primary care physicians (PCPs) should counsel and educate patients on sun protection methods, but other preventive health measures, such as smoking cessation and the participation in regular mammographies, are far more often the subject of PCP counseling.15,18
The aim of our study was to determine patient knowledge of the AAD guidelines for proper sunscreen use and to assess patient perception on having received sunscreen counseling by a physician. Previous studies have assessed rates of sunscreen counseling by dermatologists, but studies analyzing patient perception of physician sunscreen counseling are limited. In addition, we sought to define factors that influence patient knowledge about sunscreen use and perception of receiving physician counseling. By identifying gaps in patient knowledge of appropriate sunscreen use, we can improve and target educational efforts to promote the health of patients.
Methods
This was an observational, cross-sectional study using a 12-question, multiple-choice, anonymous survey that was distributed to patients presenting for routine visits at a private dermatology clinic near Detroit, Michigan. The survey was conducted from September 26, 2016 to November 5, 2016. All patients aged 18 years or older were eligible for the study. Patients who were 17 years old or younger, those who had already completed the survey, and those who declined to participate at a previous visit were excluded from the study. Nurses asked patients to complete the survey after being taken to the examination room, but prior to seeing the dermatologist. Participation was voluntary. If it was the patient’s first visit at the clinic, they were categorized as new patients. New patient responses therefore reflected counseling rates by any previous dermatologists the patient might have seen. Patients who had previously been seen by the dermatologist in the clinic were categorized as existing patients, and reported counseling rates were assumed to reflect those of the dermatology group involved in this study. Surveys were collected at the end of the visit by nursing staff. The study was Institutional Review Board review-exempt.
Patient demographics. Patient demographics and clinical characteristics are shown in Table 1. A total of 294 patients completed the survey. The majority of participants were existing patients (83.6%), female (70.4%), and aged 41 years of age or older (83.2%). Patients previously diagnosed with skin cancer made up 24.7 percent of the participants, with BCC being the most prevalent skin cancer diagnosis (73.2%). Almost all patients with skin cancer were older than 40 years of age (97.2%, p<0.0001). The most prevalent skin types in our sample were Fitzpatrick Type II (26.6%), Type III (32.1%), and Type IV (21.8%).
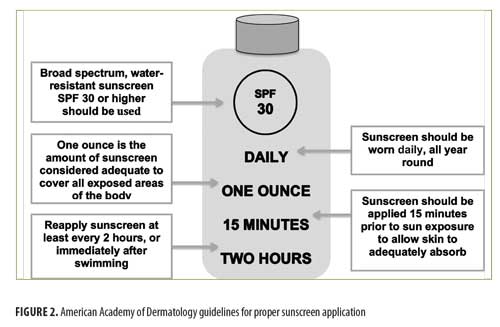
The survey (Figure 1) included questions on the following: new or existing patient, sex, age, Fitzpatrick skin type, knowledge of proper sunscreen use, previous physician counseling, if sunscreen samples would encourage sunscreen use, and previous skin cancer diagnosis. Five questions in the survey assessed patient knowledge of proper sunscreen use, including 1) how often application should occur; 2) how much sunscreen should be applied per application; 3) which level SPF sunscreen should be worn; 4) how long before sun exposure sunscreen should be applied; and 5) how frequently sunscreen should be reapplied. Answers matching the AAD guidelines (Figure 2) for proper sunscreen use were marked correct.17 AAD recommendations relevant to our study include daily, year-round use of sunscreen with a minimum SPF of 30 applied 15 minutes prior to sun exposure and reapplied every two hours with one ounce of sunscreen to adequately cover the entire body.
Statistical analysis. Data were analyzed using frequency distributions and the chi-squared test. All analysis was done using Statistical Package for the Social Sciences version 24.0 (IBM Corp., Armonk, New York); a p value of 0.05 or less was considered statistically significant.
Results
Patient knowledge of AAD guidelines. Patient answers to the five survey questions assessing knowledge of proper sunscreen use are shown in Table 2. More than half (58.5%) of patients correctly identified daily, year-round application of sunscreen as the proper frequency of sunscreen use. The remaining patients were almost evenly divided between daily sunscreen use during the summer months and sunscreen use with the anticipation of prolonged sun exposure (18.7% and 21.1%, respectively). As for level of SPF, more than half (59.9%) of patients correctly identified SPF 30 as the minimum level of UV protection, while SPF 15 was the next most common response (15.9%). For the amount of sunscreen to cover the entire body, less than half of patients correctly selected one ounce (37.7%). Time of sunscreen application prior to sun exposure was most commonly identified as 30 minutes (34.1%). The correct time interval, 15 minutes, was the second most frequent answer (33.4%). A significant portion of patients (24%) responded that sunscreen should be applied at the time of sun exposure rather than before. Forty-eight percent of patients selected two hours as the longest amount of time between sunscreen applications, while three- and four-hour intervals were the next most common responses (18.9% and 14.4%), respectively.
Factors affecting patient response. Clinical and demographic factors affecting patient responses regarding proper sunscreen use are shown in Table 3. Female participants selected daily, year-round sunscreen use more frequently than male participants (71.3% vs. 28.7%, p<0.0001) and were also more likely to select two hours as the proper maximum amount of time between sunscreen reapplication (54.0% versus 35.3%, p=0.004). Patients with Fitzpatrick Skin Types I to III were more likely to select SPF 30 than those with Fitzpatrick Skin Types IV to VI (66.1% vs. 49.5%, p=0.005). For the remaining comparisons, including patients who were new versus existing, aged 40 years and under versus aged 41 years or older, and previously diagnosed with skin cancer versus those without a skin cancer, no significant differences in knowledge were found.
Factors affecting sunscreen counseling by a physician. Patient reporting of sunscreen counseling by a physician is shown in Table 4. Fifty-six percent of respondents had not received counseling by a dermatologist or PCP. The respondents who did receive counseling were most likely to have been counseled by a dermatologist (35.4%), with only 5.2 percent of counseling reportedly performed by a PCP. Existing patients were more likely to have received prior sunscreen counseling (40.7% vs. 8.3%, p<0.0001). No difference in counseling based on sex was found. Patients aged 41 years or older (39.3% vs. 18.4%, p=0.04) reported statistically significant higher rates of counseling. Dermatologists were more likely to counsel patients regarding sunscreen use if the patients had a history of skin cancer (58.3% versus 28%, p<0.0001). About one-third (31.9%) of patients with a previous skin cancer had never been counseled. Fitzpatrick skin type was inversely associated with rates of counseling by a dermatologist, with subjects of fairest skin type (Fitzpatrick Type I) reporting the highest rates of counseling (62.5%) and rates decreasing as Fitzpatrick type increased to V; however, statistical significance could not be assessed because the data did not fit the assumptions of the chi-squared test.
Discussion
This study demonstrates a need for further patient education on proper UVR protection. While just over half of patients could properly identify the recommended frequency of sunscreen use and the minimum recommended SPF for daily sunscreen, less than half of patients knew how often to reapply sunscreen, how long before sun exposure it should be applied, and the proper amount to use to cover the entire body. This study did not collect data on patients who do not see a dermatologist; thus, we are unable to draw conclusions regarding their knowledge of AAD guidelines for appropriate sunscreen use. However, we expect that patients who routinely see a dermatologist will be better informed regarding proper photoprotection than those who do not see a dermatologist. Hence, our results likely reflect better knowledge of photoprotection guidelines among our study subjects than would be seen among the general population. Nonetheless, more than half of the patients evaluated had never received sunscreen counseling by a physician.
The effectiveness of sunscreen use in primary prevention of skin cancer compared with the current cost and morbidity of skin cancer make it imperative for physicians to emphasize sunscreen counseling in the patient education portion of the visit. We found that patients with skin cancer were more likely to report receiving sunscreen counseling, at which point it is too late to obtain the greatest benefits from sunscreen use. Considering that the most damaging sun exposure occurs during childhood and young adulthood, which then predisposes these young individuals to skin cancer later in life, there should be an increased focus on counseling efforts should be directed toward these populations in order to provide the maximum benefits of sunscreen counseling.15,19 In addition to incorporating sun protection counseling into pediatric office visits, parents of children should be counseled on the importance of sun protection for both themselves and their children when presenting for their own routine health care visits. In addition to increasing counseling, educational handouts and samples might prove helpful.
Our patient-reported rates of physician counseling were consistent with previously published ranges (1.6–58%) reported by dermatologists.15,16 However, this counseling was likely incomplete, given that existing patients, patients aged older than 40 years, and those with a history of skin cancer reported higher counseling rates, but were not more knowledgeable than their counterparts on the sunscreen guidelines.
In the survey, patients were not asked what practices they used, but instead what they believed were the recommended practices. Without appropriate knowledge, patients are unable to adhere to best practices. While patients cannot be forced to adopt AAD sunscreen recommendations, physicians must empower them with knowledge.
It is not enough for this patient education effort to end with the individual physician. Insurance companies, government agencies, and the media must also be called upon to share the message of photoprotection. Physician reimbursement modeled after the system used for discussing tobacco use and smoking cessation might be an effective incentive to increase patient counseling. In addition, increasing funds to support patient education and sunscreen availability in public arenas might also be powerful interventions. The media can assist in broadly distributing the message of photoprotection and the harmful effects of tanning. Unlike previously unsuccessful attempts, we need a coordinated effort so that proper sunscreen education for patients is comprehensive, broad-reaching, and sustained.
Limitations. There are limitations to our study. The study design was cross-sectional in nature, which limits the temporal relationships that can be drawn regarding age and skin cancer diagnosis at time of counseling. The data were also collected from two locations of a private practice, which limits the diversity in patient demographics and physician counseling practices among the patients who participated. Participation in the study was voluntary and nurse-initiated, so there might be a bias in our sample based on who was willing to complete the survey. Also, given that the data were collected by questionnaire, there is the possibility of recall bias or differences in ideas of what sunscreen counseling by a physician involves. In addition, skin type and previous skin cancer diagnoses were patient-reported and not confirmed by the dermatologist to assess response accuracy.
Conclusions
A majority of patients in our study had never received counseling on proper sunscreen use. Consistent with this finding, only two of the five correct AAD guidelines (frequency of use and minimum SPF required) received a majority response. Small differences in knowledge were seen based on sex and skin type, but there were no significant differences based on patient status, age, and previous diagnosis of skin cancer. There is still a significant portion of our patient population that is not educated on proper sunscreen use and has never been counseled by a physician on the importance of UVR protection and its multiple benefits. Focusing counseling efforts on younger adults and primary care venues can significantly increase the prevention of skin cancer. Primary prevention of skin cancer and photodamage is available, and in order to obtain its maximum benefit, a comprehensive effort to improve patient education in this regard should not be further delayed.
References
- Jansen R, Wang SQ, Burnette M, et al. Part I. Photoprotection by naturally occurring, physical, and systemic agents. J Am Acad Dermatol. 2013;69(6):853.e1–e12.
- National Toxicology Program. Ultraviolet-radiation-related exposures. National Institutes of Health sitet: http://ntp.niehs.nih.gov/ntp/roc/content/profiles/ultravioletradiationrelatedexposures.pdf. Accessed May 30, 2017.
- Koh HK, Geller AC, Miller DR, et al. Prevention and early detection strategies for melanoma and skin cancer: current status. Arch Dermatol. 1996;132(4):436–442.
- Skin cancer facts & statistics. Skin Cancer Foundation site. http://www.skincancer.org/skin-cancer-information/skin-cancer-facts. Accessed May 30, 2017.
- Coups E, Manne S, Heckman C. Multiple skin cancer risk behaviors in the U.S. population. Am J Prev Med. 2008;34(2):87–93.
- Rogers HW, Weinstock MA, Feldman SR, Coldiron BM. Incidence estimate of nonmelanoma skin cancer (keratinocyte carcinomas) in the US population, 2012. JAMA Dermatol. 2015;151(10):1081–1086.
- Robinson JK. Sun exposure, sun protection, and vitamin D. 2005;294(12):1541–1543.
- Guy GP, Machlin SR, Ekwueme DU, Yabroff KR. Prevalence and costs of skin cancer treatment in the U.S., 2002–2006 and 2007–2011. Am J Prev Med. 2014;104(4):e69–e74.
- Cancer facts and figures 2017. American Cancer Society site. http://www.cancer.org/acs/groups/content/@editorial/documents/document/acspc-048738.pdf. Accessed January 10, 2017.
- Tripp M, Peterson S, Prokhorov A, et al. Correlates of sun protection and sunburn in children of melanoma survivors. Am J Prev Med. 2016;51(3):e77–e85.
- Parkin DM, Mesher D, Sasieni P. Cancers attributable to solar (ultraviolet) radiation exposure in the UK in 2010. Br J Cancer. 2011;105 Suppl 2:S66–S69.
- Francis SO, Mahlberg MJ, Johnson KR, et al. Melanoma chemoprevention. J Am Acad Dermatol. 2006;55(5):849–861.
- Jansen R, Osterwalder U, Wang SQ, et al. Photoprotection: part II. Sunscreen: development, efficacy, and controversies. J Am Acad Dermatol. 2013;69(6):867.e1–e14.
- Buller DB, Cokkinides V, Hall HI, et al. Prevalence of sunburn, sun protection, and indoor tanning behaviors among Americans: review from national surveys and case studies of 3 states. J Am Acad Dermatol. 2011;65(5):S114–S123.
- Akamine KL, Gustafson CJ, Davis SA, et al. Trends in sunscreen recommendation among US physicians. JAMA Dermatol. 2014; 150(1):51–55.
- Winkelmann R, Rigel D. Assessing frequency and quality of US dermatologist sunscreen recommendations to their patients. J Am Acad Dermatol. 2015;72(3):557–558.
- How to apply sunscreen. American Academy of Dermatology site. https://www.aad.org/public/spot-skin-cancer/learn-about-skin-cancer/prevent/how-to-apply-sunscreen. Accessed May 30, 2017.
- DePue JD, Goldstein MG, Redding CA, et al. Cancer prevention in primary care. Prev Med. 2008;46(3):252–259.
- Mitka M. Survey finds physicians rarely advise use of sunscreen to patients, even those most at risk for skin cancer. 2013;310(13):1328.

