 by Michael Mickel md; Rainer Kunstfeld mD; and Richard Crevenna, MD
by Michael Mickel md; Rainer Kunstfeld mD; and Richard Crevenna, MD
Drs. Mickel and Crevenna are with the Department of Physical Medicine, Rehabilitation, and Occupational Medicine at the Medical University of Vienna in Austria. Dr. Kunstfeld is with the Department of Dermatology at the Medical University of Vienna.
Funding: No funding was provided for this study.
Disclosures: The authors have no conflicts of interest relevant to the content of this article.
Abstract: In this case report, the authors describe a first-time trial of a variation of extracorporeal shockwave therapy in a patient with disseminated granuloma annulare. Radial pulse therapy was administered in an outpatient clinic of a university hospital to a 72-year-old woman with a 14-year history of disseminated granuloma annulare. The authors describe changes in clinical appearance and results of histological evaluation, reporting observable positive changes in all four treated plaques. The authors conclude that radial pulse therapy was well-tolerated and seemed to influence the course of disseminated granuloma annulare plaques positively.
Keywords: Disseminated granuloma annulare, extracorporeal shockwave therapy, radial pulse therapy
J Clin Aesthet Dermatol. 2018;11(1):32–34
Introduction
Extracorporeal shockwave therapy (ESWT), first used to break up kidney stones,1 has found widespread use in orthopedics and traumatology. ESWT is being used in clinical trials more often for a growing variety of skin conditions.2–5
Extracorporeal shockwaves (ESW) are defined as a sequence of sonic pulses characterized by a high peak pressure, fast pressure rise, and short life cycle. The physical forces of applied ESW lead to increased local tissue perfusion, elevated nitric oxide, and angiogenesis. ESW influences anti-inflammatory mechanisms and collagen synthesis.6,7 A variation of ESWT—termed radial pulse therapy (RPT)—is generated by a ballistic source. It is not characterized by high peak pressure but rather by pressure waves. These waves are not focused and they do not have a penetrating effect; instead, they demonstrate a superficial effect.8
ESWs in soft-tissue indications are a form of mechanotherapy. There is no direct mechanical effect, but an indirect effect does occur via the pathways of biological reactions.9 These biological reactions are an area of increasing interest in scientific research.
The basic findings of histological analyses related to the mechanism of ESWT7 and the histopathology of granuloma annulare (GA)10 led us to attempt a first-time trial of RPT in a patient suffering from GA. To our knowledge, there is no evidence in medical literature on ESWT/RPT for the treatment of GA.
Case Report
We performed RPT on a 72-year-old female patient who had been suffering from disseminated GA (GAD) for 14 years. This patient was unresponsive to multiple therapeutic regimens. Systemic (e.g., dimethyl fumarate, chloroquinphosphat, dapsone, infliximab, rifampicin, ofloxacin, minocycline, acitretin, corticosteroids, and methotrexate) and topical therapies (e.g., tacrolimus, corticosteroids) as well as photo-chemotherapy showed either no effect or only a fractional effect or were not tolerated by the patient.
RPT was applied to a total of four plaques (Plaques A, B, C, and D) located on both dorsal forearms. In each session, 500 shots were delivered to each plaque with a pressure of 2.5 bars and a frequency of four pulses per second. All RPT sessions were conducted by one operator using a Swiss DolorClast® CLASSIC device (EMS Electro Medical Systems SA, Nyon, Switzerland). Ultrasound gel was applied to improve conduction. The pressure waves deployed were not at an energy density that caused pain, so no analgetic pre-medication was necessary. RPT was well-tolerated, and the patient finished therapy with no adverse events. Photographs of treated areas were taken at each therapy session.
All treated plaques showed observable changes (Table 1). Plaque A showed the most distinct improvement (Figure 1). Skin biopsy specimens from Plaque A demonstrated histological changes after RPT (Figure 2).

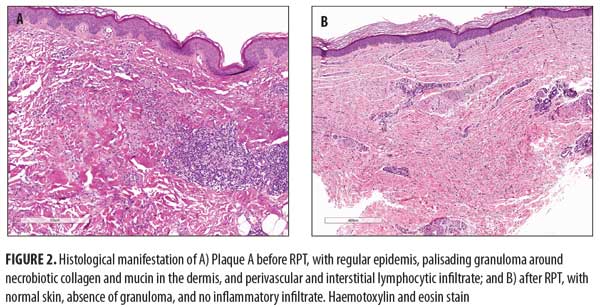
Follow-up six weeks later showed that Plaque A (demonstrating the longest duration of treatment) was still stable. Plaque B disappeared after RPT. Plaques C and D showed a regrowth of the ridges and increased redness.
Discussion
RPT/ESWT is used in skin regeneration efforts such as scar treatment and wound healing.4,5 Based on this and our own positive experiences using RPT/ESWT for the treatment of soft tissue conditions, (e.g., chronic soft tissue wounds, skin fibrosis associated with systemic sclerosis, scleredema) we attempted RPT for the treatment of GAD and our patient. We observed positive effects in all treated GA plaques. The remission of one small plaque led to the assumption that RPT might bring incipient GA plaques to a complete remission if treatment is started at an early stage of the disease. Treatment is only feasible in patients with no disseminated course of GA. It is evident that RPT in GAD is limited by the impracticality of treating a large number of plaques in the same patient. In these patients, only cosmetically defacing plaques on the limbs or trunk should be chosen. Nevertheless, treating GAD with RPT provided us the opportunity to treat and observe GA plaques in different stages of disease progression simultaneously.
RPT/ESWT appears to play a role in the recruitment of regenerative mesenchymal stem cells.7 In our patient, no additional plaques occurred distally on either elbow during treatment, which suggest that RPT/ESWT might have a positive effect beyond treatment area.
Additional questions regarding technical implementations remain, such as the number of necessary RPT sessions and the most effective energy flux density. In the meantime, the appropriate technical setting of RPT should be determined according to ESWT/RPT trials for other cutaneous indications. No negative or adverse events occurred in our patient. Only short-term localized reddening of the skin as a sign of hyperemia was observed. In the medical literature, there are reports of temporary pain and small hematomas, depending on the energy level of RPT/ESWT used. If contraindications and risk factors are considered (e.g., malignant tumor in the treatment area, fetus in the treatment area), RPT seems to be a safe method free of severe side effects.
Conclusion
RPT is a feasible, cost-effective, well-tolerated treatment and seems to influence the course of GAD plaques positively. Further randomized and controlled clinical studies should performed to confirm these preliminary results.
References
- Chaussy C, Brendel W, Schmiedt E. Extracoporeally induced destruction of kidney stones by shock waves. 1980;2(8207):1265–1268.
- Stieger M, Schmid JP, Yawalkar N, Hunziker T. Extracorporeal shock wave therapy for injection site panniculitis in multiple sclerosis patients. 2015;230(1):82–86.
- Tinazzi E, Amelio E, Marangoni E, et al. Effects of shock wave therapy in the skin of patients with progressive systemic sclerosis: a pilot study. Rheumatol Int. 2011;31(5):651–656.
- Fioramonti P, Cigna E, Onesti MG, et al. Extracorporeal shock wave therapy for the management of burn scars. Dermatol Surg. 2012;38(5):778–782.
- Mittermayr R, Antonic V, Hartinger J, et al. Extracorporeal shock wave therapy (ESWT) for wound healing: technology, mechanisms, and clinical efficacy. Wound Repair Regen. 2012;20(4):456–465.
- Vetrano M, d’Alessandro F, Torrisi MR, et al. Extracorporeal shock wave therapy promotes cell proliferation and collagen synthesis of primary cultured human tenocytes. Knee Surg Sports Traumatol Arthrosc. 2011;19(12):2159–2168.
- Frairia R, Berta L. Biological effects of extracoporeal shock waves on fibroblasts. a review. Muscles Ligaments Tendons J. 2011;1(4):138–147.
- Cleveland RO, Chitnis PV, McClure SR. Acoustic field of ballistic shock wave therapy device. Ultrasound Med Biol. 2007;33(8):1327–1335.
- d’Agostino MC, Craig K, Tibalt E, Respizzi S. Shock wave as biological therapeutic tool: from mechanical stimulation to recovery and healing, through mechanotransduction. Int J Surg. 2015;24(Pt B):147–153.
- Smith MD, Downie JB, DiCostanzo D. Granuloma annulare. Int J Dermatol. 1997;36(5):326–333.

