 J Clin Aesthet Dermatol. 2020;13(6):xx–xx
J Clin Aesthet Dermatol. 2020;13(6):xx–xx
by Sandrine Sebban, MD
Dr. Sebban is in private practice in Paris, France.
FUNDING: No funding was provided for this study.
DISCLOSURES: The author owns shares in Soft Medical Aesthetics.
ABSTRACT: Background. There is currently no standardized and reproducible injection technique to address facial aging at all anatomical levels.
Objective. The Sebban Technique One-point (STOP) Facial Aging Method™ for hyaluronic acid (HA) fillers aims to provide predictive results using a single point of entry.
Methods. STOP combines two complementary techniques: Deep One-point (DOP) and Superficial One-point (SOP). DOP targets the deep plane to restructure the facial architecture, while SOP targets the superficial and deeper hypodermic planes to add volume and provide optimal tissue hydration. The injection procedure involves one DOP phase and two SOP phases using an HA filler appropriate for the treatment indication and injection depth. STOP has been investigated in a retrospective, open-label observational case series.
Results. Data from 10 women, aged 41 to 59 years, with varying stages of facial aging were retrospectively examined. Eight had received DOP with bolus injections of a cohesive HA filler and nine had received SOP using an HA filler with good elasticity to target the deep or superficial hypodermis. The mean total volume of HA filler injected (all HA fillers combined) was 5.46mL (range: 4.0–7.0mL) for the whole face. Physician and patient satisfaction with the treatment was high and all subjects stated that they would recommend the treatment to their friends. The STOP protocol was well-tolerated and no complications were observed during the DOP or SOP phases.
Conclusions. STOP is a reproducible and safe technique for global facial rejuvenation with a single cannular point of entry.
Keywords: Hyaluronic acid, global face approach, one-point technique, deep and superficial volume loss
It is only relatively recently, after decades of research, that we have a better understanding of the anatomical changes that occur in the facial skeleton and overlying soft tissues over time.1–4 Facial aging involves interactions between bone, muscle, fat, and skin that result in changes in quality, shape, and contour.5 At the deepest level, resorption of the craniofacial skeleton alters the support base for the overlying tissues and correlates with outward soft tissue changes associated with aging.6 The deep and superficial fat layers exist as well-delineated, separate compartments.1 With age, the redistribution and loss of fat in these compartments, assisted by changes in muscle tone and activity, can significantly alter face shape.7,8 At the uppermost level, changes in skin tone and elasticity also contribute to an aged appearance.1,9 These facial changes do not occur simultaneously and different facial compartments age at different levels so that obvious transition zones become apparent in the form of deep folds or sunken hollows.
With our increased understanding of facial anatomy and how it is influenced by aging, aesthetic indications have been developed to address all anatomical layers and restore the overall three-dimensional appearance of the face while maintaining natural facial contours.9 This increased knowledge of facial anatomy has also improved safety and allowed practitioners to avoid vascular complications. For individuals not wanting to undergo surgery, dermal fillers offer an alternative solution. The hyaluronic acid (HA) fillers, in particular, are available with a wide range of properties, with differences in manufacturing processes altering their degree of cross-linking density, particle size, and HA concentration and, therefore, their suitability for individual indications.10,11
The aim of the current study was to present a new injection protocol for HA fillers, the Sebban Technique One-point (STOP) Facial Aging Method™. This technique uses a single cannula point of entry to address facial aging at all anatomical levels with reduced pain and trauma and with a low risk of vascular complications, while allowing the physician to be artistic with the treatment. Retrospective results from a small case series of patients at varying stages of facial aging are presented to illustrate the benefits of this technique.
Methods
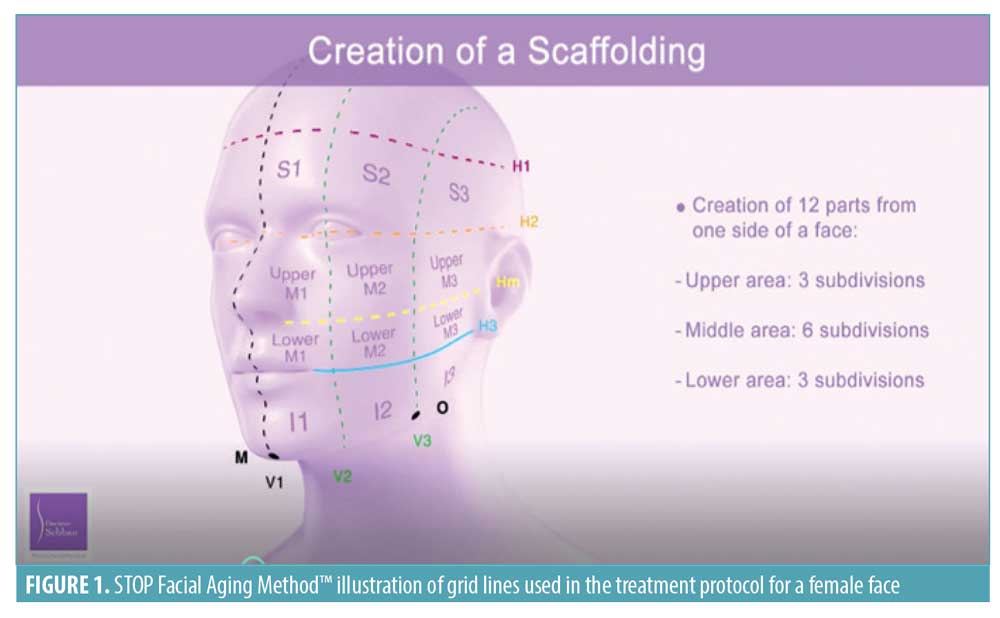
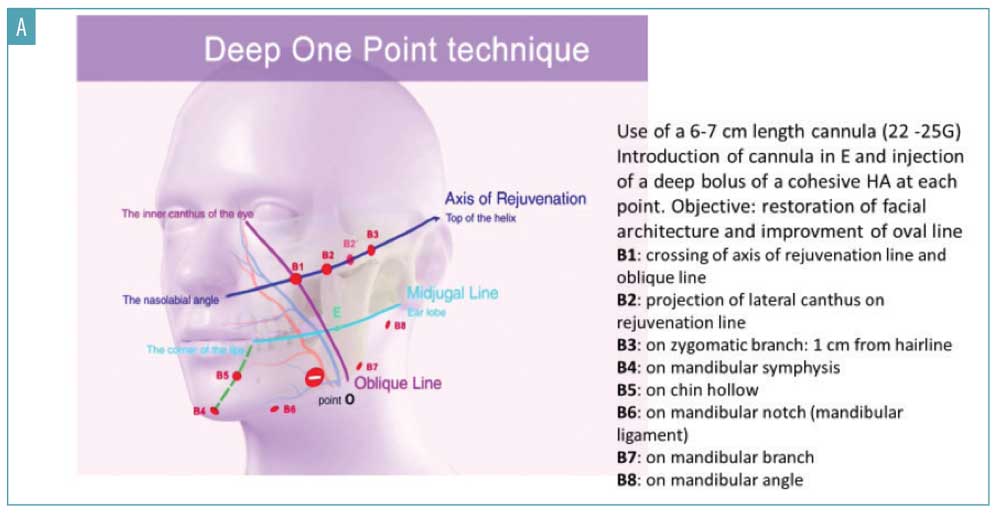
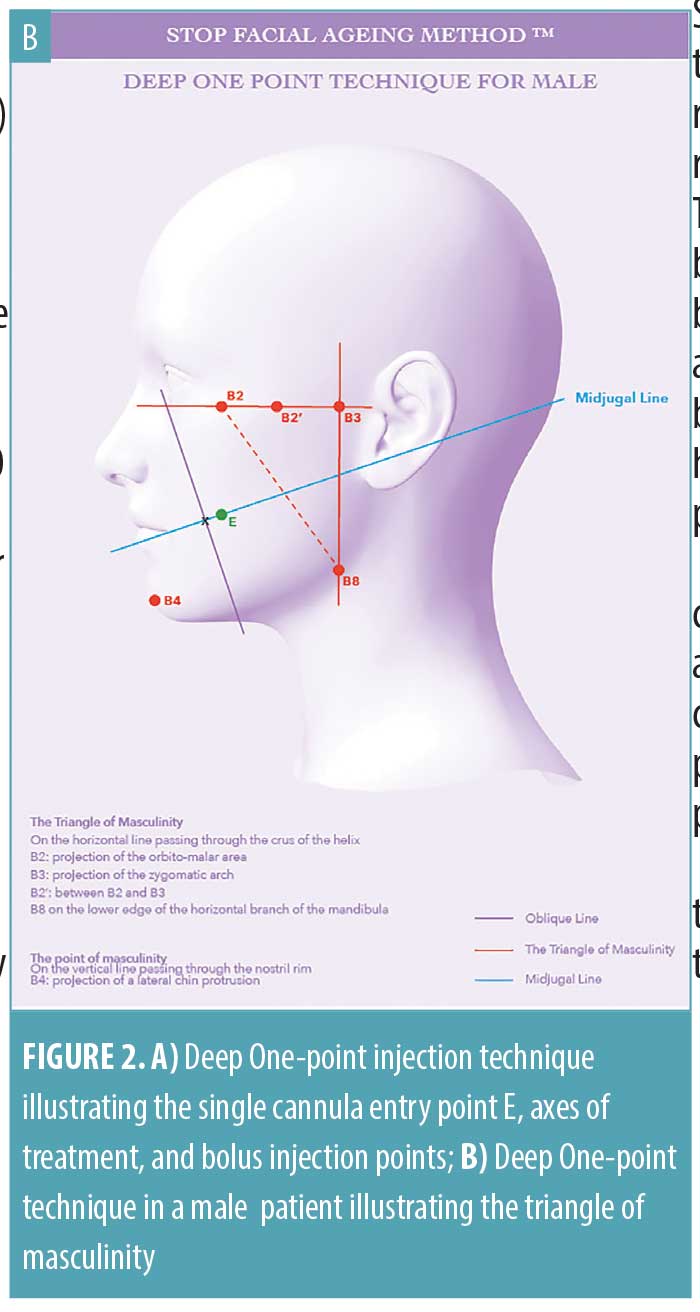
Developing the framework. The first stage in the STOP protocol is to establish a framework for the facial volume restoration. This scaffolding is required to restore a more youthful facial anatomy at both deep and superficial tissue depths and is achieved by dividing each side of the face into a grid of 12 squares, which correspond to the superficial fat compartments. As illustrated in Figure 1, each side of the face comprises three squares in the top half, six squares in the middle, and three squares in the bottom half. The grid also enables the STOP single-injection entry point to be determined. This is achieved by marking the intersection of the oblique line—which passes through the inner canthus of the eye and Point O (positioned two-thirds of the way along the oval line in grid V3)—and the midjugal line (Figure 2A). The single cannula insertion point (E, entry point) is located 5mm behind this mark on the midjugal line (Figure 2A). Point O represents the anterior border of the masseter and is an important landmark for the facial artery location, which crosses the horizontal branch of the mandible just anterior to the masseter muscle at the antegonial notch.
STOP combines two complementary techniques: Deep One-point (DOP) and Superficial One-point (SOP). The DOP technique targets the deep plane to restructure the facial architecture by restoring volume and treating ptosis. This can be adapted for the male face by focusing on areas of masculine bone architecture, such as the jawline and chin. The SOP technique targets both the superficial and deeper hypodermic planes to add volume and provide optimal tissue hydration.
The injection procedure is conducted in the physician’s office and consists of three successive steps corresponding to the three treatment phases: one DOP phase and two SOP phases.
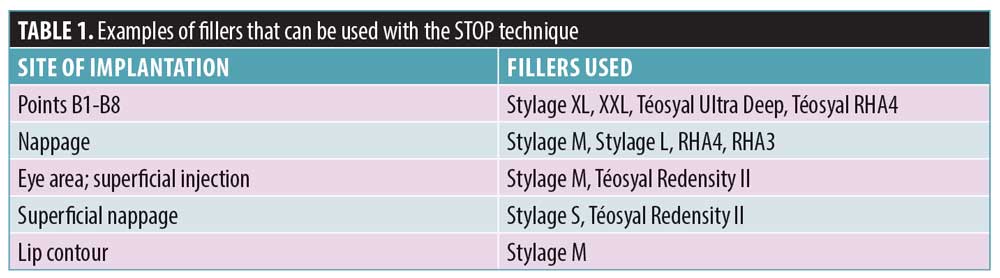
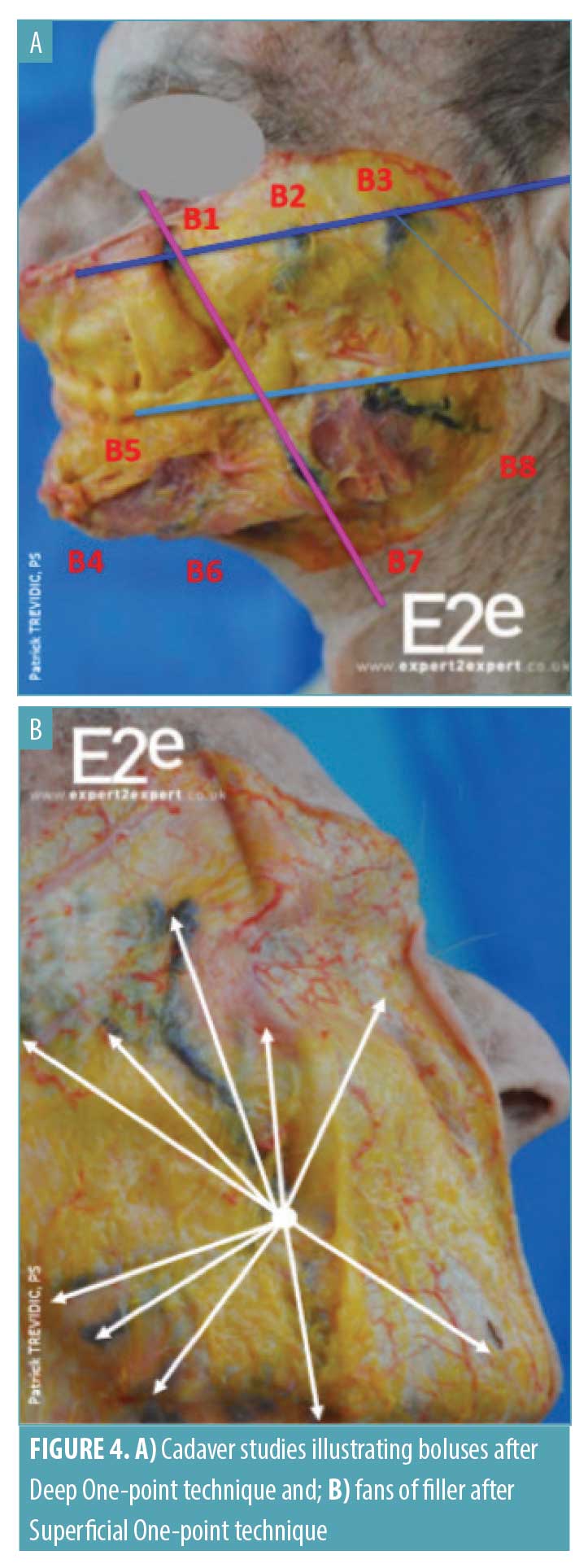
DOP technique. This technique targets the middle and deep planes of the face to re-establish a firm support for overlying tissues. A cannula is selected that is not too flexible (6–7cm in length, 22–25-gauge) and inserted into a deep plane with the bevel pointing downwards. Boluses of a cohesive HA filler, which boasts a good balance of rigidity and flexibility (Table 1), are then injected at specfic points along the axes of treatment (Figure 2A). Boluses are placed in the deep plane at the supraperiostal level. The location of the boluses will depend upon the indications being treated. For example, in the upper third of the face, boluses are placed along the axis of rejuvenation at points B1 to B3 (Figure 2A). If the subject requires treatment of dark circles under their eyes, four micro-boluses are injected in the suborbital region (MB1–MB4) using an HA filler adapted for this area (Table 1 and Figure 2A). In the lower third of the face, the boluses are injected mainly along the mandibular branch (B4–B8) (Figure 2A). Importantly, all boluses are injected from the same point of entry E.
In the male face, the DOP technique focuses on the “triangle of masculinity,” adding relief to the bone architecture of the jaw with the projection of the mandibular angle and the orbitomalar and zygomatic zones (Figure 2B). The DOP technique can also be used by the injector to accentuate the width or the length of the chin.
SOP technique. This technique targets either the deep or superficial hypodermis to restore fat volume loss, smooth superficial rhytides, and hydrate the skin. For the deep injections, a Softfil® EasyGuide 25-gauge (50 or 60mm) cannula (Soft Medical Aesthetics, Paris, France) is introduced into the deep hypodermis via the same cannula entry point (E) as before. Using a fanning technique, an HA filler with good elasticity is placed in the middle and lower thirds of the face, avoiding the suborbital region and the jowl area (Figure 3). The SOP technique can also be used to restore volume to the lips and treat the perioral region.
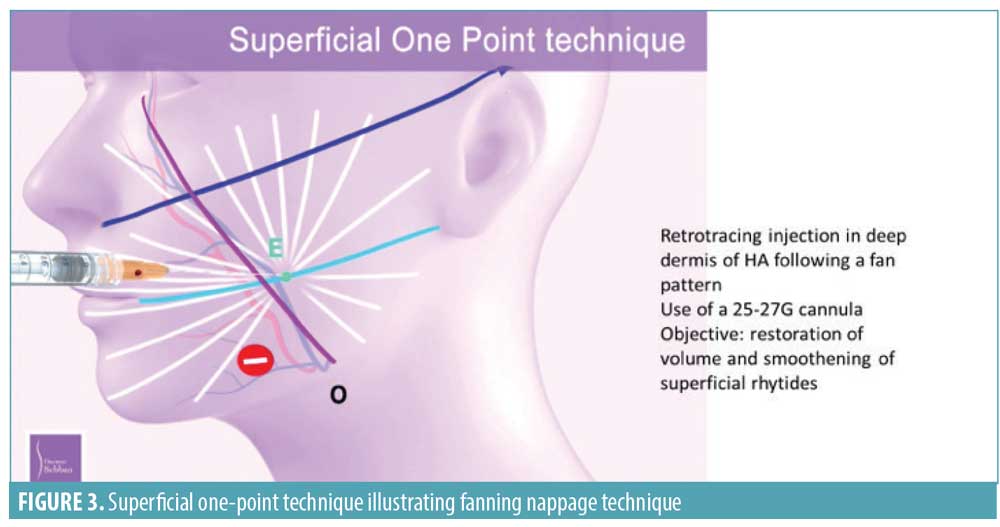
The superficial hypodermis injections are performed with a Softfil® EasyGuide 27-gauge (40mm) cannula using the same fanning technique, but this time in a more superficial plane with an HA filler with little or no crosslinking.
Treatment plan. The STOP method can be used in people of all ages, beginning at the first signs of aging. In individuals younger than 40 years old displaying minimal signs of aging, the SOP technique alone might be sufficient with a total HA filler volume of 2 to 4mL. Among those 40 to 50 years of age seeking facial rejuvenation, both the DOP and SOP techniques are recommended, as they work in harmony to restore facial architecture, add volume, and smooth lines and wrinkles. A total HA filler volume of 4 to 6mL is generally required for these patients. After 50 years of age, annual follow-up visits should be planned with the SOP technique performed annually and combined with the DOP technique every two years. In these individuals, a total HA filler volume of 6 to 8mL might be required.
Localization of HA filler following injection. HA filler placement after injection using the STOP protocol has been evaluated in both cadaver and magnetic resonance imaging (MRI) studies. For the cadaver studies, a cohesive HA filler colored with methylene blue dye was injected using the STOP protocol and the cadaver was subsequently dissected to observe filler deposition in the different facial planes. When injected using the DOP technique, boluses of filler were clearly visible at the periosteal level (Figure 4). Likewise, when injected using the SOP technique, fan lines were visible in the superficial hypodermis (Figure 4).
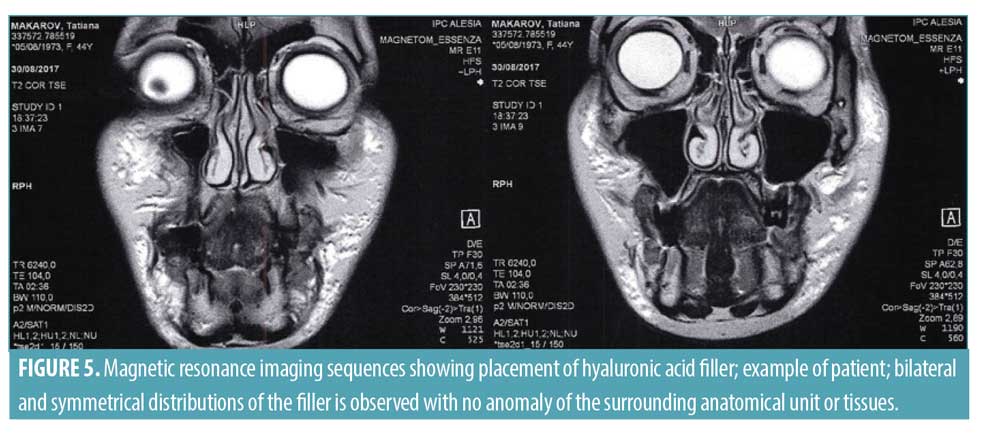
In four subjects, filler placement was also visualized at six months by MRI investigation (Siemens Magnetom Essenza 16, Centre d’Imagerie Parisien, Dr R. Souillard-Scemama). MRI T2 axial and coronal sequences taken three weeks after HA filler was injected using the STOP protocol confirmed bilateral and symmetrical distribution of filler in the face in the expected areas (Figure 5). MRI has previously demonstrated efficacy for the identification of facial fillers and associated complications.12 The MRI images showed no evidence of any adverse effects of HA filler injected using the STOP technique.
Retrospective, open-label observational case series. Individuals aged 30 to 60 years presenting to a private aesthetic surgery practice for a facial rejuvenation procedure were accepted for the STOP technique if they had no medical history that would contraindicate injection with a facial filler, including no history of permanent fillers. Patients received full information about the treatment, technique of administration, outcomes, pre- and post-procedure care, side effects, potential complications, and any other additional information required to achieve optimum results. The study complied with all ethical requirements including those outlined in the Declaration of Helsinki and Good Clinical Practice guidelines. All participants were required to show willingness and an ability to return for a follow-up visit and to provide signed, informed consent for the procedure and subsequent use of their photographs for scientific purposes.
All treated patients made two visits to the practice: a treatment visit and a follow-up visit scheduled for 30 to 60 days later. At the first visit, subjects underwent a careful facial examination to determine the extent of treatment required. Those with evidence of changes to the facial skeleton underwent both DOP and SOP, while those whose aging-related facial changes were confined to the soft tissue underwent SOP alone. The subject’s face was then divided into the grid pattern illustrated in Figure 1 and the point of entry and axes of treatment weres marked. Prior to the procedure, anesthetic in the form of xylocaine was injected at the cannula insertion Point E. With the subject in a supine position, an HA filler appropriate for the treatment indication and injection depth was injected according to the previously described STOP protocol. No massage is required after treatment, but patients are advised to avoid activities that cause the face to heat, such as sports, for one week and spa treatments, such as saunas or hammams, for two weeks. Photographs were obtained at baseline and at the follow-up visit using standardized positioning and lighting.
At the follow-up visit, the treating physician evaluated each individual’s before and after photos and assessed the degree of improvement using a five-category Global Aesthetic Improvement Scale (GAIS) as either much improved, improved, no change, worse, or much worse.
Participants also received a satisfaction questionnaire, which they were asked to complete several months after the STOP procedure had been performed. As part of the questionnaire, subjects were required to rate their satisfaction with the aesthetic results and quality of their skin using a five-point scale, where 1=worse and 5=very much improved. They were then asked whether they agreed or disagreed with the following statements: “I feel more attractive,” “I feel better,” “I have more confidence in my appearance,” and “I benefit from the treatment in my professional life.” The final part of the questionnaire asked whether participants would repeat the treatment or recommend it to a friend. Adverse events were documented.
Results
Retrospective data of patients treated with the STOP protocol were available for 10 women ranging in age from 41 to 59 years old and with a mean age of 48.6 years. All subjects attended both visits. Eight women underwent the DOP procedure with bolus injections with a cohesive HA filler at bolus points B1 to B8. The mean total volume injected (both sides of the face) was 3.15mL (range: 1.7–4.0mL). Two women received DOP jawline treatment (injection at bolus points B6–B8) with a total mean volume of 1.5mL (range: 1.0–2.0mL). Three women were injected in the periocular area with microbolus injections in the deep plane (bolus points MB1–MB4) with a mean volume of 0.83mL (0.5–1.0mL). Nine women underwent the SOP procedure using an HA filler with good elasticity to target the deep or superficial hypodermis with a nappage of fanning injections. The mean total volume for this procedure was 2.24mL (1.6–4.0mL). The lips were treated in one subject with 1mL.
The mean total volume of HA filler injected (all HA fillers combined) was 5.46mL (range: 4.0–7.0mL) for the whole face. For individuals aged 40 to 50 years, the mean volume was 5.12mL and, for those aged 50 to 60 years, it was 5.8mL. Figure 6 shows images of subjects before and after treatment with the STOP protocol from three different age categories: 30 to 40, 40 to 50, and 50 to 60 years old.

The mean time between treatment and physician GAIS rating was 38 days, but one rating was performed on the day of injection. Physician scores of subject appearance according to GAIS were rated as “much improved” in 70 percent of subjects and “very much improved” in 30 percent of subjects.
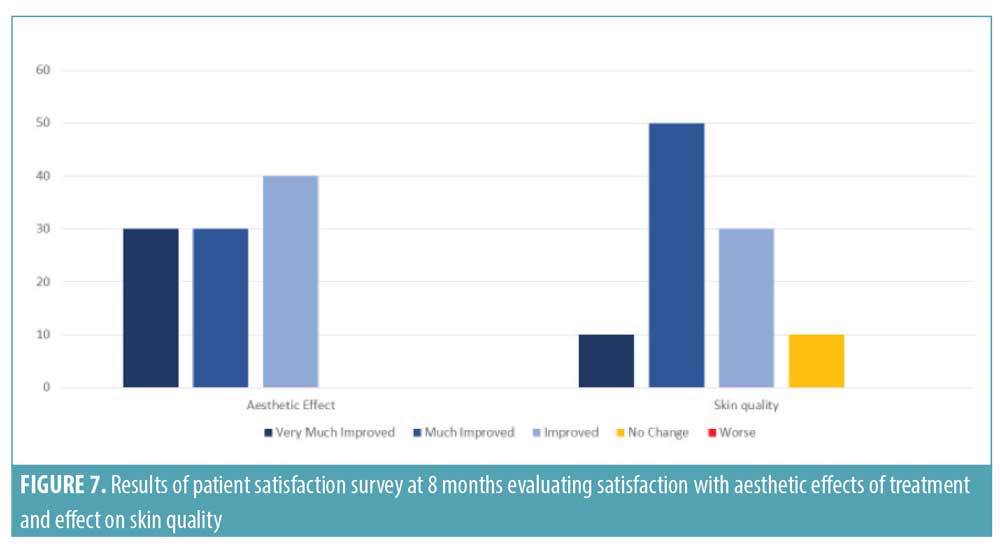
The satisfaction questionnaire was completed, on average, eight months after the treatment had been performed. Satisfaction remained high at eight months after treatment, with all women reporting the aesthetic results remained improved to very much improved and 90 percent of women reporting improved skin quality (Figure 7). All subjects agreed that the treatment made them feel more attractive or more comfortable with their body, feel better in general, and gave them more confidence with their appearance. In addition, 90 percent felt that it helped them in their professional life. Eight women confirmed that they would repeat the STOP treatment protocol. One woman stated she would not repeat the treatment but, nevertheless, felt that it had brought “freshness to her face and had a small lifting effect.” One woman was not sure if she would repeat the treatment but commented that the “treatment was effective, not noticed by family [or] acquaintances, and gave a glow to her face.” All subjects stated that they would recommend the treatment to their friends.
Treatment with the STOP protocol was well-tolerated and no complications were observed with the DOP and SOP techniques.
Discussion
It is generally agreed that, to create a natural, more youthful appearance in facial aesthetics, volume restoration and contouring using a global facial approach is required.13 This concept has been adopted by many physicians who routinely inject individuals with dermal fillers with varying techniques to replace volume at different anatomical layers. At present, there is no uniform consensus about the techniques used to inject dermal fillers in clinical practice. The aim of STOP was to provide a standardized, reproducible treatment protocol with predictive results. The STOP method differs from other techniques in that it combines injections in different planes with a single point of entry to create a tissue-supporting scaffold. By dividing the face into a framework based on anatomical structures, it ensures that treatment is individualized for each patient. The retrospective survey of patients treated with the STOP protocol demonstrates that the protocol was effective at restoring age-associated facial volume loss across three age generations, resulting in more youthful looking faces with defined contours as well as an improved skin condition.
Facial aging affects all anatomical layers, including the skeleton, which results in a loss of bony support.14 This causes overlying soft-tissue structures to appear sunken and wrinkled. The STOP procedure combines two complementary techniques. The first corrects the loss of bony support with the DOP approach, providing a firm foundation for the overlying superficial musculo-aponeurotic system (SMAS), which lifts and repositions the subcutaneous fat pads. The SOP technique then addresses facial aging in the overlying tissues, restoring volume to the fat pads and the superficial hypodermis to smooth superficial rhytides and hydrate the skin. The process targets three different anatomical layers, smooths the boundaries that aging introduces between the different facial areas, and re-establishes facial contours. The procedure can also be adjusted depending on the degree of age-related changes. For example, younger individuals might only show signs of superficial volume loss and can therefore be treated with SOP alone, whereas, in older individuals, restoration of both the facial architecture and soft tissue volume loss might be necessary. If required, treatment can also be targeted to specific areas of the face, such as the cheeks, jawline, and tear troughs.
The STOP protocol is unique in that injections are performed via a defined, single cannula entry point for each side of the face. This central cheek entry point allows all areas of the face to be accessed and HA filler to be distributed homogeneously. It also reduces the tissue trauma caused by multiple entry points. As part of the protocol, the face is divided into a series of grids based on facial anatomy. This allows dermal filler to be placed in defined locations designed to maximize treatment benefits in a reproducible manner. The correct placement of filler using this technique has been confirmed by both cadaver dissections and MRI imaging. The latter is valuable for imaging facial fillers as it localizes filler at the same time as providing an anatomical reference.15 The current paper does not recommend individual fillers for the STOP protocol, as availability will vary from country to country, but when more than one product is required in the same patient, it is advisable to use products from the same range. It is the role of the physician to select the most appropriate filler for the technique being performed. For example, when performing the DOP technique, it is important that an HA filler with high cohesivity is selected that provides good volume and projection without spreading through the tissues.
After treatment with the STOP protocol, the appearance of all subjects in the case series was rated as “much improved” to “very much improved” by the physician. Due to the subjective nature of cosmetic improvements, outcomes measured from a patient’s point of view are also important in aesthetic medicine.16 A satisfaction questionnaire confirmed that all subjects considered the aesthetic effect to be “improved” to “very much improved” and 90 percent reported improved skin quality at an average of eight months after treatment. Superficial injection of HA fillers has been shown to improve elasticity and skin hydration.17
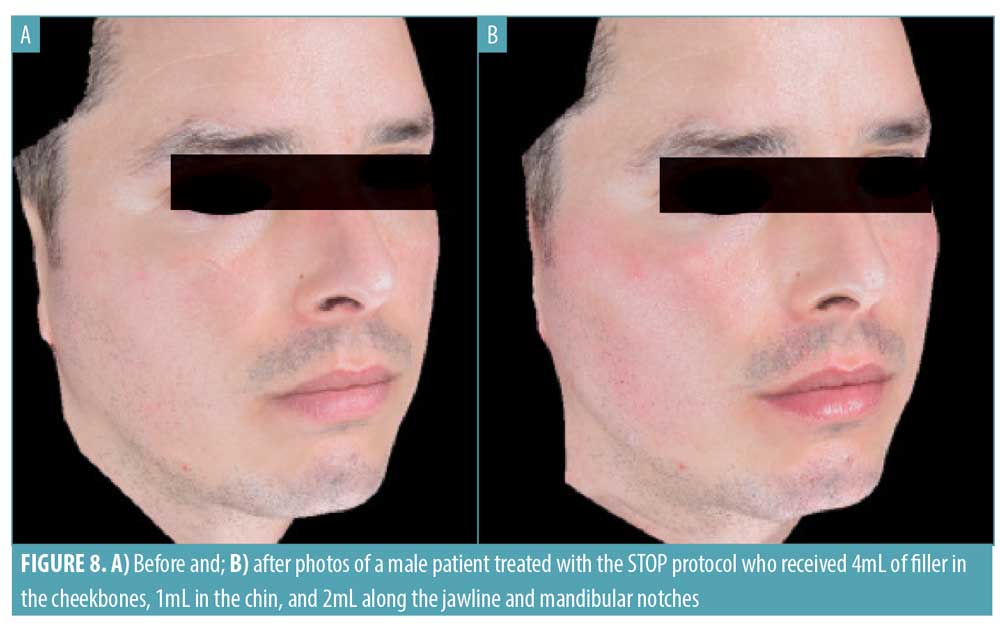
All subjects reported they felt more attractive after the procedure and more confident in their appearance. Eight of 10 reported they would repeat the treatment and all said they would recommend it to friends. Women in this study ranged in age from 41 to 59 years old, supporting that the STOP protocol is of benefit for people of a wide age range at different stages of facial aging; the STOP protocol has also yielded satisfactory results in male patients (Figure 8).
 Aesthetic treatments with HA fillers are not permanent and annual follow-up visits are required to maintain optimal results. A sound understanding of the structural basis on which they are laid is therefore important. By addressing volume loss in both the facial skeleton and soft tissue, physicians will be able to treat both the cause and effect and therefore increase the longevity of treatment results. The reproducibility of the STOP protocol allows this to be achieved. The retrospective nature of this study means that it was open to certain biases. Larger, prospective studies with long-term follow-up are now warranted in subjects of varying ages and different ethnicities to confirm the current findings.
Aesthetic treatments with HA fillers are not permanent and annual follow-up visits are required to maintain optimal results. A sound understanding of the structural basis on which they are laid is therefore important. By addressing volume loss in both the facial skeleton and soft tissue, physicians will be able to treat both the cause and effect and therefore increase the longevity of treatment results. The reproducibility of the STOP protocol allows this to be achieved. The retrospective nature of this study means that it was open to certain biases. Larger, prospective studies with long-term follow-up are now warranted in subjects of varying ages and different ethnicities to confirm the current findings.
Conclusion
The STOP Facial Aging Method™ combines both deep and superficial HA volumizing techniques with a single cannular point of entry. By restoring an individual’s baseline facial anatomy and replacing volume loss in the overlying soft tissues, a global face approach is achieved. The advantages are that a large surface area can be treated with minimal pain and trauma, using an MRI-supported, reproducible methodology, that provides harmonious and natural results.
References
- Rohrich RJ, Pessa JE. The fat compartments of the face: anatomy and clinical implications for cosmetic surgery. Plast Reconstr Surg. 2007;119(7):2219–2227.
- Pessa J. The tear trough and lid/cheek junction: anatomy and implications for surgical correction. Plast Reconst Surg. 2009;123(4):1332–1340.
- Gierloff M, Stöhring C, Buder T, Gassling V, Acil Y, Wiltfang J. Aging changes of the midfacial fat compartments: a computed tomographic study. Plast Reconstr Surg. 2012;129(1):263–273.
- Pessa JE. SMAS fusion zones determine the subfascial and subcutaneous anatomy of the human face: fascial spaces, fat compartments, and models of facial aging. Aesthet Surg J. 2016;36(5):515–526.
- Fitzgerald R, Graivier MH, Kane M, et al. Update on facial aging. Aesthet Surg J. 2010;30 Suppl:11S–24S.
- Shaw RB, Kahn DM. Aging of the midface bony elements: a three-dimensional computed tomographic study. Plast Reconstr Surg. 2007;119(2):675–681.
- Wollina U, Wetzker R, Abdel-Naser MB, Kruglikov IL. Role of adipose tissue in facial aging. Clin Interv Aging. 2017;12:2069–2076.
- Kruglikov IL, Wollina U. Soft tissue fillers as non-specific modulators of adipogenesis: change of the paradigm? Exp Dermatol. 2015;24(12):912–915.
- Coleman SR, Grover R. The anatomy of the aging face: volume loss and changes in 3-dimensional topography. Aesthet Surg J. 2006;26(1S):S4–59.
- Edsman K, Nord LI, Ohrlund K, et al. Gel properties of hyaluronic acid dermal fillers. Dermatol Surg. 2012;38(7 Pt 2):1170–1179.
- Sundaram H, Rohrich RJ, Liew S, et al. Cohesivity of hyaluronic acid fillers: development and clinical implications of a novel assay, pilot validation with a five-point grading scale, and evaluation of six U.S. Food and Drug Administration-approved fillers. Plast Reconstr Surg. 2015;136(4):678–686.
- Tal S, Maresky HS, Bryan T, et al. MRI in detecting facial cosmetic injectable fillers. Head Face Med. 2016;12(1):27.
- Muhn C, Rosen N, Solish N, et al. The evolving role of hyaluronic acid fillers for facial volume restoration and contouring: a Canadian overview. Clin Cosmet Investig Dermatol. 2012;5:147–158.
- Shaw RB, Katzel EB, Koltz PF, et al. Aging of the facial skeleton: aesthetic implications and rejuvenation strategies. Plast Reconstr Surg. 2011;127(1):374–384.
- Mundada P, Kohler R, Boudabbous S, et al. Injectable facial fillers: imaging features, complications, and diagnostic pitfalls at MRI and PET CT. Insights Imaging. 2017;8(6):557–572.
- Sears DE, Chung KC. A guide to interpreting a study of patient-reported outcomes. Plast Reconstr Surg. 2012;129(5):1200–1207.
- Baspeyras M, Rouvrais C, Liégard L, et al. Clinical and biometrological efficacy of a hyaluronic acid-based mesotherapy product: a randomised controlled study. Arch Dermatol Res. 2013;305(8):673–682.
