 J Clin Aesthet Dermatol. 2020;13(4 Suppl):S26-S29
J Clin Aesthet Dermatol. 2020;13(4 Suppl):S26-S29
by Joe Monroe, MPAS, PA
Mr. Monroe is a Fellow of the American Academy of Physician Assistants; is Founder, Past President, and Current Fellow of the Society of Dermatology Physician Assistants; and practices general and surgical dermatology in Tulsa, Oklahoma.
FUNDING: No funding was provided for the preparation of this article.
DISCLOSURES: The author has no conflicts of interest relevant to the content of this article.
ABSTRACT: At the beginning of the 21st century, the prevalence of Cimex species (bedbugs) infestation in human dwellings rose exponentially, particularly in the United States. Although there is no evidence that bedbugs transmit diseases to their hosts, they are difficult to eradicate, making them a source of psychological and physical distress and a socioeconomic burden to society. Here, the author describes the case of an eight-year-old boy who presented with widespread, multiple, itchy, red papules surrounded by round patches of erythematous, edematous skin, and was eventually diagnosed with cimicosis (bedbug infestation). Other family members living with the boy showed no clinical signs of bedbug infestation, and the bites on the boy were not in the typical three-row linear configuration associated with bedbug bites—which made this case compelling. Clinical diagnostic characteristics, symptom management, and suggestions on infestation eradication are provided. Biological and epidemiological characteristics of bedbug infestation are also described. Currently, evidence of simple, safe, and effective means of bedbug eradication is lacking.
KEYWORDS: Bedbug, Cimex species, Cimex lectularius, Cimex hemipterus, pediatric
A bedbug is a wingless, bloodsucking, hemipterous bug of the Cimex (C.) species (C. lectularius, C. hemipterus) known to infest human housing, especially beds, and feed on human blood.1 Bedbug infestation was relatively uncommon in the United States (US) until the early 21st century, when bedbug infestation exponentially increased.2 The increased prevalence of bedbug infestation in the US is thought to be linked to the high number of Americans (up to 40%) currently living in multifamily dwellings.2,3 A combination of insecticide resistance among bedbugs and increased international travel by Americans is also thought to contribute to the increased prevalence.2,4 Currently, evidence of simple, safe, and effective means of bedbug eradication is lacking.
In this report, the author presents an atypical case of cimicosis (bedbug infestation) in an eight-year-old boy. Clinical diagnostic characteristics, symptom management, and suggestions on cimicosis eradication are provided. Biological and epidemiological characteristics of cimicosis are also described.
Case Report
An eight- year-old boy presented to an outpatient dermatology clinic for evaluation of widespread, multiple, itchy, red papules that were surrounded by round patches of erythematous, edematous skin. The boy had experienced several such episodes since moving into a new apartment with his family six months prior to presentation. No other family members showed similar cutaneous symptoms.
The child was otherwise healthy, though he appeared somewhat atopic, suffering from seasonal allergies, exertional asthma, and occasional flares of eczema—similar symptoms of which were experienced by several other family members. The patient and his family members denied symptoms of joint pain, fever, or malaise.
The family had suspected that bedbugs were responsible for the boy’s itchy rash, but because they were not able to confirm the presence of the organisms in their home and none of the other family members exhibited similar cutaneous symptoms, the explanation was discarded. Nonetheless, when the family went on a vacation, they used an over-the-counter (OTC) pest fumigator in an effort to eliminate any potential bedbugs; however, the boy’s cutaneous manifestations resumed upon his return home. The boy’s pediatrician prescribed a topical steroid cream (triamcinolone 0.1%) to help with the itching.
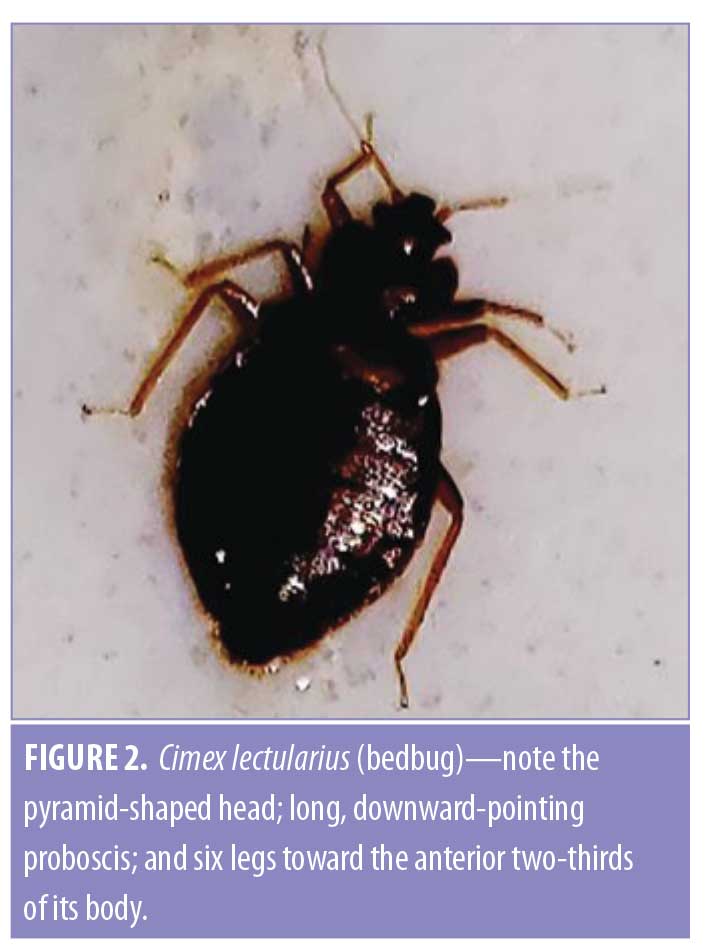
The boy was seen in the dermatology clinic on several occasions. Each time, similar red bumps were observed (Figure 1), varying in number from 3 to 8 discrete lesions, each of which comprised a central tiny blister or scab surrounded by an erythematous, edematous circle and ranged in size from 1cm to 3.5cm; the lesions appeared in a single, transverse, linear configuration just above the patient’s waistline. There was not tenderness on palpation, and nodes were not palpable in the groin or axillary areas.

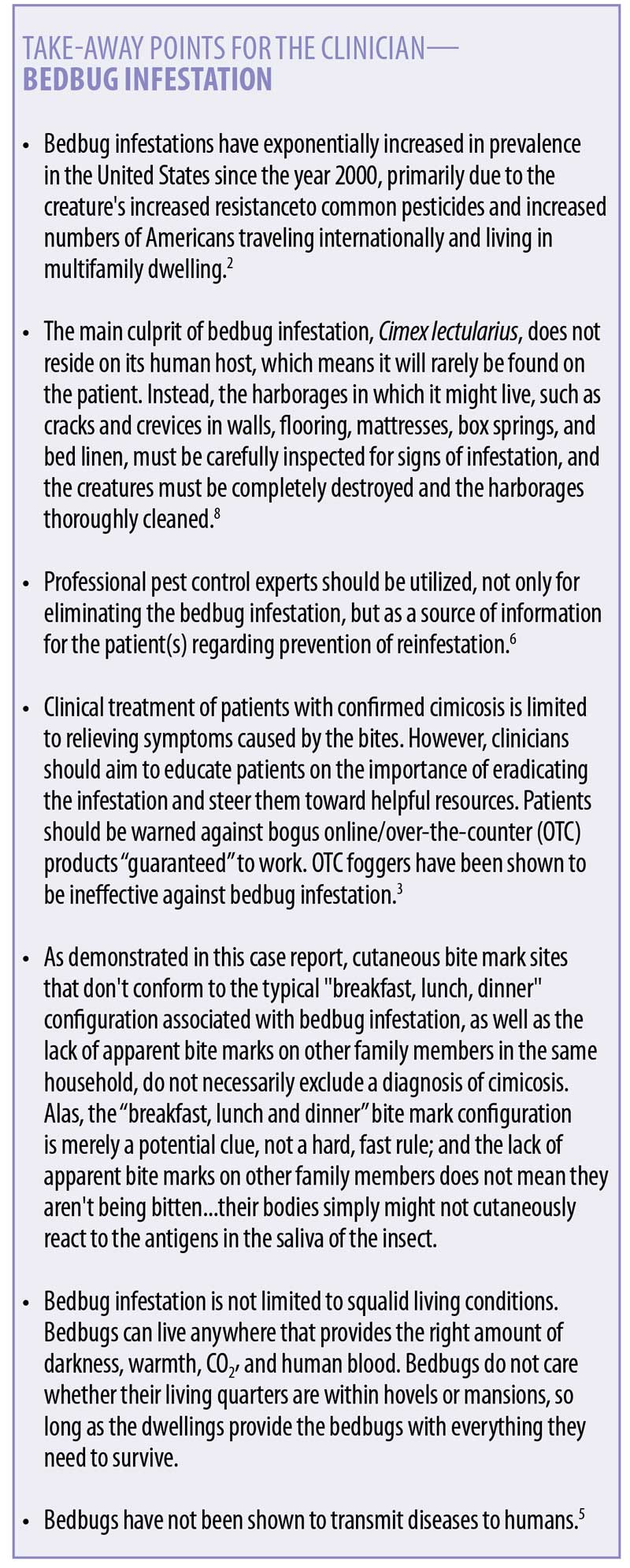
On the final visit, the family brought in one of several “bugs” they had found between the boy’s mattress and box spring. They were not able to find similar bugs in any other bedroom. Examination of the organism showed it to be a 5mm-long, brown, thin, oval, roach-like insect. It was still quite alive and able to crawl rapidly when provoked. Under 10-power microscopic examination, a pyramid-shaped head and long, downward-pointing proboscis could be seen, along with six legs located on the anterior two-thirds of the creature (Figure 2).5
Clinically, based on the appearance of the skin lesions, their manner of configuration (linear), and their associated symptomatology, along with the confirmed identification of a bedbug extracted from the boy’s bedding, a confident diagnosis of cimicosis (bedbug infestation) was made. A biopsy was felt to be unnecessary, though had a biopsy been performed, histological findings of the arthropod bites would have included scattered eosinophils in interstitial locations, especially in the deep dermis.6 Biopsy of a bedbug bite site may show spongiosis, acanthosis, and mild parakeratosis, though it should be noted that these findings are consistent with arthropod bites of all types.6
The list of differential diagnoses for this type of clinical picture is lengthy and may include scabies (caused by parasitic mites [e.g., Sarcoptes scabiei], mosquito bites, and eczema, among many others. Typically, if a confirmed sighting of the bedbugs and/or bedbug droppings (with typical musty odor and pinpoint orange staining of bedding) are not made in the presence of cutaneous manifestations, other diagnoses should most likely be explored; however, if suspicions of cimicosis are strong, a qualified pest control agent can confirm the presence of the infestation in the patient’s dwelling.7–9
C. lectularius can be extremely difficult to eliminate. In this particular case, the family of the boy resided in a multifamily structure that they reported was not well-cared for by the landlords; additionally, many of the people living in the building were truckers, whose frequent traveling would have provided ample opportunity for the organism to continually be brought back into the house from other infested places.7–9
In the boy’s case, we were able to provide an accurate diagnosis, offer itch relief with use of a topical steroid cream, and encourage the family to pursue pest control intervention through the landlord. With the exception of itch control, there are no other clinical treatment approaches for cimicosis. We did not feel a follow-up visit was necessary in the boy’s case, though, in some cases in which a language barrier is present, a return visit with an interpreter can be extremely helpful in educating the patient on managing the infestation.
BedBug Biology
Also called chinches, redcoats, or mahogany flats, bedbugs known to commonly affect humans are from the Cimex family (Cimicidae), with C. lectularius (in temperate regions) and C. hemipterus (in tropical and sub-tropical regions) predominating. Other species of these obligate bloodsuckers occasionally wander onto humans but are far more common on creatures such as bats.8
The adult C. lectularius is typically flat, unless it has just fed, and closely resembles a tiny cockroach. The female creature’s abdomen is rounded on the tip, while the male’s is pointed.5 Their appearance changes drastically after ingesting blood, which increases their length 30 to 50 percent, increases their weight 150 to 200 percent, and turns their body color from dark brown to a reddish orange. Their excreta present as tiny brown particles and by pinpoints of dark orange staining on the bed, clothes, and bed linens (which often have a residual musty odor).5
Bedbugs do not reside on their human hosts—they dwell in cracks and crevices close to where humans live, such as in bedding, flooring cracks, behind wallpaper, on headboards, and between the mattress and box springs. Feeding only at night, bedbugs are sensitive to light and seldom dwell more than eight feet away from their victim’s bed.5,8
Bedbug bites are not usually immediately noticeable, but antigens in the creature’s saliva can lead to an itchy, swollen papule on the host, which often vesiculates and is frequently surrounded by a ring of erythema and edema. Severity of cutaneous reaction is, in large part, a reflection of how atopic the host is; a similarly observed reaction can be seen with bites from mosquitoes, ticks, and chiggers.7,9–11
A linear configuration of bedbug bites is considered diagnostic, and these configurations are commonly seen in rows of threes (so-called “breakfast, lunch, and dinner”).12 However, some researchers believe the concept of the three linear bite rows representing three separate mealtimes is a myth because multiple bites that are randomly distributed are at least as common and can be easily explained by any number of factors, such as multiple bedbugs biting the host simultaneously or bites that fail to tap into blood vessels.13
The adult female bedbug mates and lays her eggs in the creature’s harborage (never on the host’s body), where the eggs hatch within 10 days, producing nymphs that immediately begin to feed. Starting early in their life cycle, bedbugs can feed once a week. As they develop into adulthood, they might feed more often, even daily. Adult bedbugs, however, can survive for weeks to months between feedings, if necessary. Actual feeding takes only 5 to 6 minutes.5,8
The complete life cycle of a bedbug is 6 to 12 months. Bedbugs at every stage of life are attracted to warmth, darkness, and CO2.Fortunately, bedbugs do not appear to carry or transmit any contagious diseases,14 but their presence might generate psychological distress, in addition to pruritus.
Cimicosis Treatment
Treating the environment. Since bedbugs cannot live or multiply on their human hosts, the emphasis on “treatment” of bedbugs should be aimed at the environmental harborages where the bugs reside, mate, and multiply. This might seem obvious, but this must be made clear to the patient/patient’s family, who might believe otherwise. Patients should be encouraged to find and eliminate the bedbugs in their hiding places. Steam treatment and vacuuming the areas where the organisms are found are reasonable pest control options. But with persistent cases, consulting a qualified professional pest control expert is suggested. Pest control companies are probably the best sources of information on how to most effectively manage bedbug infestations, but local health departments are also helpful, and there are multiple resources available online.3,5,15–17
It should also be stressed to patients that having an infestation of bedbugs is not a reflection of their socioeconomic status or hygiene. A popular bedbug myth is that bedbugs are only found in squalid living conditions. The truth is bedbugs do not care how far up or down the socioeconomic ladder a dwelling is as long as it provides the darkness, warmth, CO2, and blood they need for survival. In fact, bedbugs have been found in the best hotels and finest homes.3,13
Patients should also be informed that while it is not uncommon for one person in an infested bed to have bite marks while his or her bedmate appears bite free, it is highly probable that both bedmates are being bitten—one person might react enough to the bedbug’s saliva to produce the visible, itchy lesions, whereas in the other person, the bite does not cause a symptomatic reaction at all. Atopic patients, especially those previously bitten, tend to react more vigorously to any insect bite.10,11
Treating the clinical symptoms. Contrary to patient expectation, the clinical treatment of bedbugs is primarily confined to controlling the symptoms created by the bites and educating the patients on how to eradicate the organisms from their dwelling. For treating the symptoms of bedbug bites, topical steroids (e.g., a Class III topical steroid cream) and antihistamines (e.g., hydroxyzine orally at bedtime) can reduce the itching, potentially buying the patient a good night’s sleep. In especially severe cases, systemic glucocorticoids can be used short term to good effect, though this is seldom necessary. The dosage of prednisone ranges from 5 to 60mg per day for a week, depending on the patient’s size, age, and symptom severity. Prednisone should be taken with food to avoid acid reflux and should be avoided by patients with diabetes (since it increases blood sugar levels) and by patients with hypertension, chronic heart disease, current infections, or dementia—all of which can be worsened by systemic steroids.18 These contraindications should be thoroughly discussed with the patient and family before treatment is instituted.
Conclusion
In summary, medical providers can be helpful in confirming a diagnosis of cimicosis, alleviating some of the clinical discomfort associated with the bites, and providing education on available measures aimed at eradicating the infestation. Consultation with professional pest control experts should be recommended to the patient to assist in fully eradicating an infestation; these experts are great resources in general for patients with questions or concerns regarding bedbug infestations.
Unfortunately, evidence for the existence of simple, safe, and effective eradication methods of bedbug infestation is lacking. OTC fumigators, for example, have been found to be ineffective against bedbug infestation.3,4 On a national level, the United States Environmental Protection Agency (EPA) and the Centers for Disease Control and Prevention (CDC) have been working on the bedbug epidemic, producing criteria for infestation confirmation and best practices for eradication, which has been officially termed IPM (Integrated Pest Management), for various state and local government entities.17 In addition, the EPA formed a group (Federal Bedbug Work Group), which produced a document in February 2015 called the “Collaborative Strategy on Bedbugs,” which calls for further research on safer, more effective pesticides and urges the utilization of qualified pest control experts in the eradication and prevention of infestations by the pests. This type of information can be especially helpful in cases of multifamily dwelling infestations (e.g., apartment buildings, hotels, and other similar housing).3,5,8,9,15–17
References
- Meriam-Webster Dictionary site. Bedbug. https://www.merriam-webster.com/dictionary/bedbug. Accessed 5 Jun 2020.
- United States Centers for Disease Control and Prevention. Bedbugs. https://www.cdc.gov/parasites/bedbugs/. Accessed 5 Jun 2020.
- Taisey, AA, Neltner, T. What’s working for bedbug control in multifamily housing: reconciling best practices with research, and the realities of implementation. National Center for Healthy Housing, 2010. https://nchh.org/resource-library/report_what’s-working-for-bed-bug-control-in-multifamily-housing.pdf. Accessed 5 Jun 2020.
- Jones S, Bryant J. Ineffectiveness of OTC foggers against the bedbug. J Econ Entomol. 2012; 105(3):957–963.
- University of Minnesota Extension site. Bedbugs. https://extension.umn.edu/biting-insects-and-insect-relatives/bed-bugs. Accessed 12 Jun 2020.
- Perkins, I, Gardner, J, et al. Histology of arthropod bites. Reviewed 13 DEC 2019. Pathology Outlines site. https://www.pathologyoutlines.com/topic/skinnontumorarthropod.html. Accessed 5 June 2020.
- Goddard, J, Deshazo, R. Bedbugs (C. lectularius) and clinical consequences of their bites. JAMA. 2009; 301(13):1358-1366.
- Koehler RM, Pereira MP, Lehnert P, Hertz J. Florida insect management guide for bedbugs. Publication #ENY-227. Original publication date April 1993. Revised November 2008, July 2011, and October 2013. Reviewed January 2017. Gainsville, FL: University of Florida IFAS Extension. https://edis.ifas.ufl.edu/ig083. Accessed 5 June 2020.
- Doggett, S, Dwyer, D, et al. Bedbugs: clinical relevance and control options. Clin Microbiol Rev. 2012;25(1):164–192.
- Goddard J. [Bedbug supplement] How bedbug bite reactions differ. 30 Dec 2014. PCT Magazine site. https://www.pctonline.com/article/pct1214-bed-bugs-bite-allergic-reactions/. Accessed 11 Jun 2020.
- Hossler EW. Arthropod bite reaction (bug bite, insect bite, insect sting). 2017. Dermatology Advisor site. https://www.dermatologyadvisor.com/home/decision-support-in-medicine/dermatology/arthropod-bite-reaction-bug-bite-insect-bite-insect-sting/. Accessed 11 Jun 2020.
- Fitzpatrick JE, High WA, Kyle WL (eds). Blisters and vesicles. In: Urgent Care Dermatology: Symptom-Based Diagnosis. New York, NY: Elsevier Inc.;2018: 163–204
- Utah Department of Health Bureau of Epidemiology site. Common myths about bedbugs. Updated 28 May 2020. https://health.utah.gov/epi/diseases/bedbugs/myths. Accessed 21 Mar 2020.
- Lai O, Ho D, Glick S, Jagdeo J. Bed bugs and possible transmission of human pathogens: a systematic review. Arch Dermatol Res. 2016;308(8):531?538.
- Adrian B, Dooley O, Huang C, Levkowitz M. Tackling bed bugs: a starter guide for local government. June 2015. Revised May 2016. Evans School of Public Policy and Governance, University of Washington. http://npic.orst.edu/pest/bedbug/tacklingbbstarterguide.pdf. Accessed 11 Jun 2020.
- Cornell University College of Agriculture and Life Sciences site. New York State Integrated Pest Management. Bedbugs resources. https://nysipm.cornell.edu/whats-bugging-you/bed-bugs/. Accessed 12 Jun 2020
- United States Environmental Protection Agency site. Integrated pest management: controlling bedbugs using IPM. .https://www.epa.gov/bedbugs/controlling-bed-bugs-using-integrated-pest-management-ipm. Accessed 12 Jun 2020.
- Poetker DM, Reh DD. A comprehensive review of adverse effects of systemic corticosteroids. Otolaryngol Clin North Am.2010 Aug;43(4):753–756.

