 J Clin Aesthet Dermatol. 2021;14(8):61–65.
J Clin Aesthet Dermatol. 2021;14(8):61–65.
by Khaled Seetan, MD; Mohammad Al-Zubi, MD; and Rami Al-Omari, MD
Dr. Seetan is with the Department of Dermatology, Faculty of Medicine, Yarmouk University in Irbid, Jordan. Dr. Al-Zubi is with the Department of Surgery and Specialized Surgery, Faculty of Medicine, Yarmouk University in Irbid, Jordan. Dr. Al-Omari is with the Department of Ophthalmology, Faculty of Medicine, Yarmouk University in Irbid, Jordan.
FUNDING: No funding was provided for this article.
DISCLOSURES: The authors report no conflicts of interest relevant to the content of this article.
ABSTRACT: Background. Hidradenitis suppurativa (HS) can be a severe condition that impacts patients’ health and quality of life. One aspect that can be impaired is sexual health, with many patients suffering from sexual dysfunction (SD). There are numerous articles describing this association.
Objective. We sought to synthesize and analyze the recent available evidence on HS and SD.
Methods. A systematic review was conducted. Three medical databases were used: Medline, Embase, and Cochrane. All types of epidemiological articles were included, while reviews, guidelines, protocols, conference abstracts, and case report articles were excluded. This review covers the past eight years.
Results. Twelve studies were included for review, with the most common study design being cross-sectional. Most studies involved surveys and questionnaires, with some using control groups to compare results. SD affected roughly half of patients with HS, and was found more frequently in women. Comorbidities included psychological conditions, such as depression and low self-esteem, as well as metabolic and cardiovascular diseases.
Conclusion. HS is significantly associated with sexual health issues, including SD in women and erectile dysfunction in men.
Keywords: Hidradenitis suppurativa, sexual dysfunction, meta-analysis
Hidradenitis suppurativa (HS), also known as acne inversa, is a chronic skin condition that causes persistent boil-like lumps or nodules under the skin, which become inflamed and painful; their rupture results in draining abscesses, which produce extensive scarring of the skin during the healing process.1 These nodules most commonly occur in intertriginous regions, such as the axillary, inguinal, and perianal areas, and can lead to fistula and sinus tract formation in severe cases.2 This condition starts with follicular occlusion of the folliculopilosebaceous units (FPSUs) in areas of the body that also contain a high concentration of apocrine glands, which trap bacteria and result in immune responses (perifollicular lympho-histiocytic inflammation) and follicular rupture; this leads to clinical HS lesions.3
The exact etiology of HS is unknown, although both hormones (as it occurs after puberty) and the immune system are believed to be involved. It is a multifactorial disease, with both genetic and environmental factors playing a key role; recent studies indicate roughly 30 percent of patients have a family history of this condition, suggesting an autosomal dominant inheritance pattern.4,5 The condition’s onset is typically sometime after the age of 11 years, averaging around a person’s early twenties.6 HS has an estimated worldwide prevalence of 1 to 4 percent worldwide, being three times more common in women than men.7 Patients’ disease burden includes extreme pain, work disability, and overall poor quality of life (QoL), resulting in psychological stress, depression, and social stigma.8 One problem linked to HS is sexual dysfunction (SD). Researchers have found a high prevalence of SD in patients with HS, suggesting that sexual impairment is partly due to disease activity, symptoms, and active lesions.9 There has been a deeper exploration of this link in recent years, although there is still a lack of current studies; therefore, the aim of this systematic review and meta-analysis was to compile the available research on HS and SD, determining the prevalence of these comorbidities. In this way, any new findings and studies can be more easily integrated and reviewed.
Methods
Definitions. The Diagnostic and Statistical Manual of Mental Disorders, fifth edition, explains that SD, also known as sexual disorder, is any difficulty experienced by an individual or couple during normal sexual activities, such as desire, preference, physical pleasure, arousal, or orgasm; it is diagnosed when a person feels severe distress or interpersonal strain for at least six months, with a profound impact on perceived quality of sexual life.10
Inclusion and exclusion criteria. Study inclusion criteria included articles written in English and published after 2012 from peer-reviewed journals in three major databases (Medline, Embase, and Cochrane). All types of epidemiological studies regarding SD in patients with HS were included and analyzed; these were clinical trials, case-control studies, as well as cohort and cross-sectional studies. Reviews, guidelines, protocols, case reports, and conference abstracts were excluded.
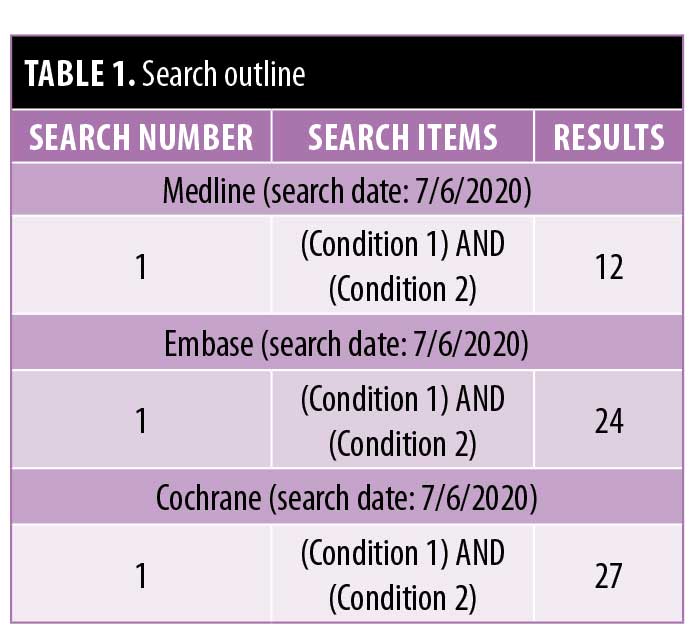
Bibliographic search. A literature search of Medline, Embase, and Cochrane was conducted on July 6, 2020, using the following search string: (“hidradenitis suppurativa” OR “acne inversa”) AND (“sexual” OR “sexual dysfunction”) (Table 1). One researcher independently reviewed the articles to assess relevant studies, reviewing the full texts of all articles meeting the inclusion criteria, including the articles’ bibliographic resources. Relevant articles were then included into our analysis.
Variables. The variables assessed were study design (including sample size) and level of scientific evidence; other variables included tools used to assess SD as well as statistical analysis and results.
Results
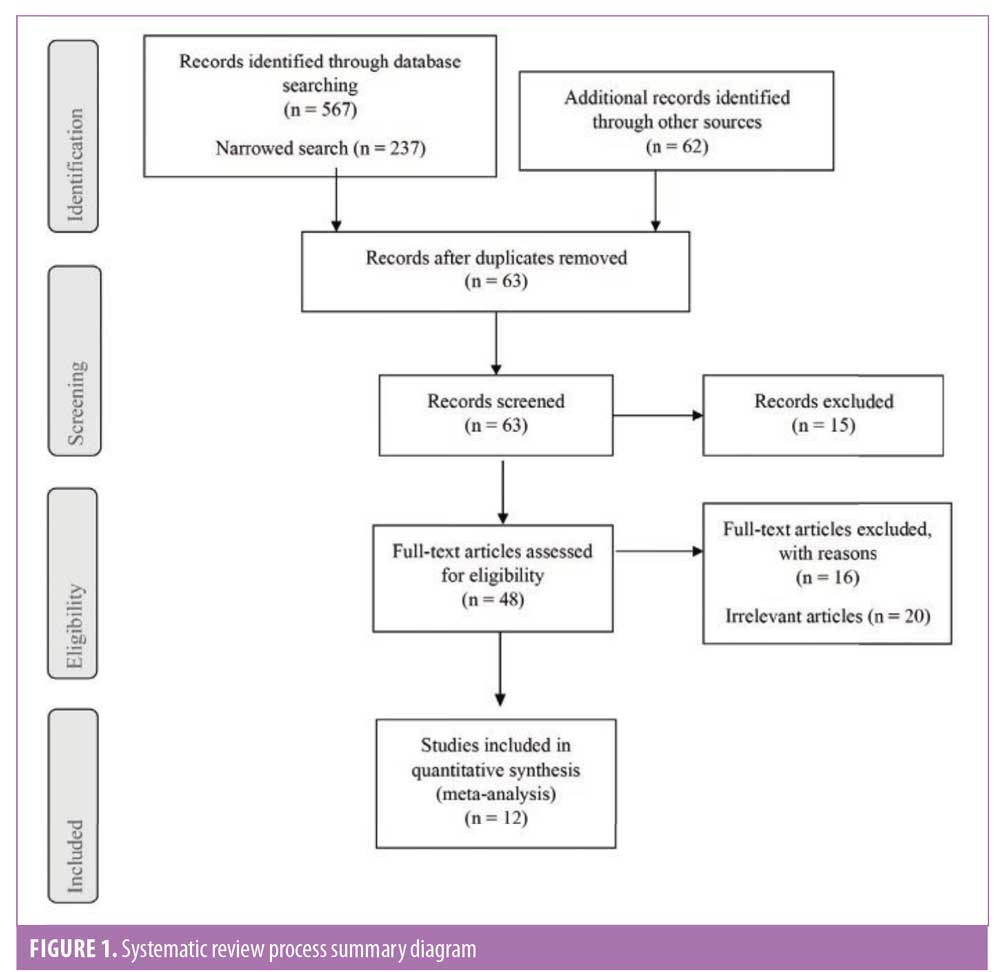
Study design. A total of 567 articles were identified from the electronic database search, with 62 additional records identified through other sources. After eliminating duplicates, reviewing titles and abstracts, and applying inclusion and exclusion criteria, 12 epidemiological studies were considered relevant and included for review (Figure 1 and Table 2). The most frequently used tools for assessing sexual function were the Female Sexual Function Index (FSFI) and its short variant (FSFI-6) and the International Index of Erectile Function (IIEF) and its short variant (IIEF-5), respectively.
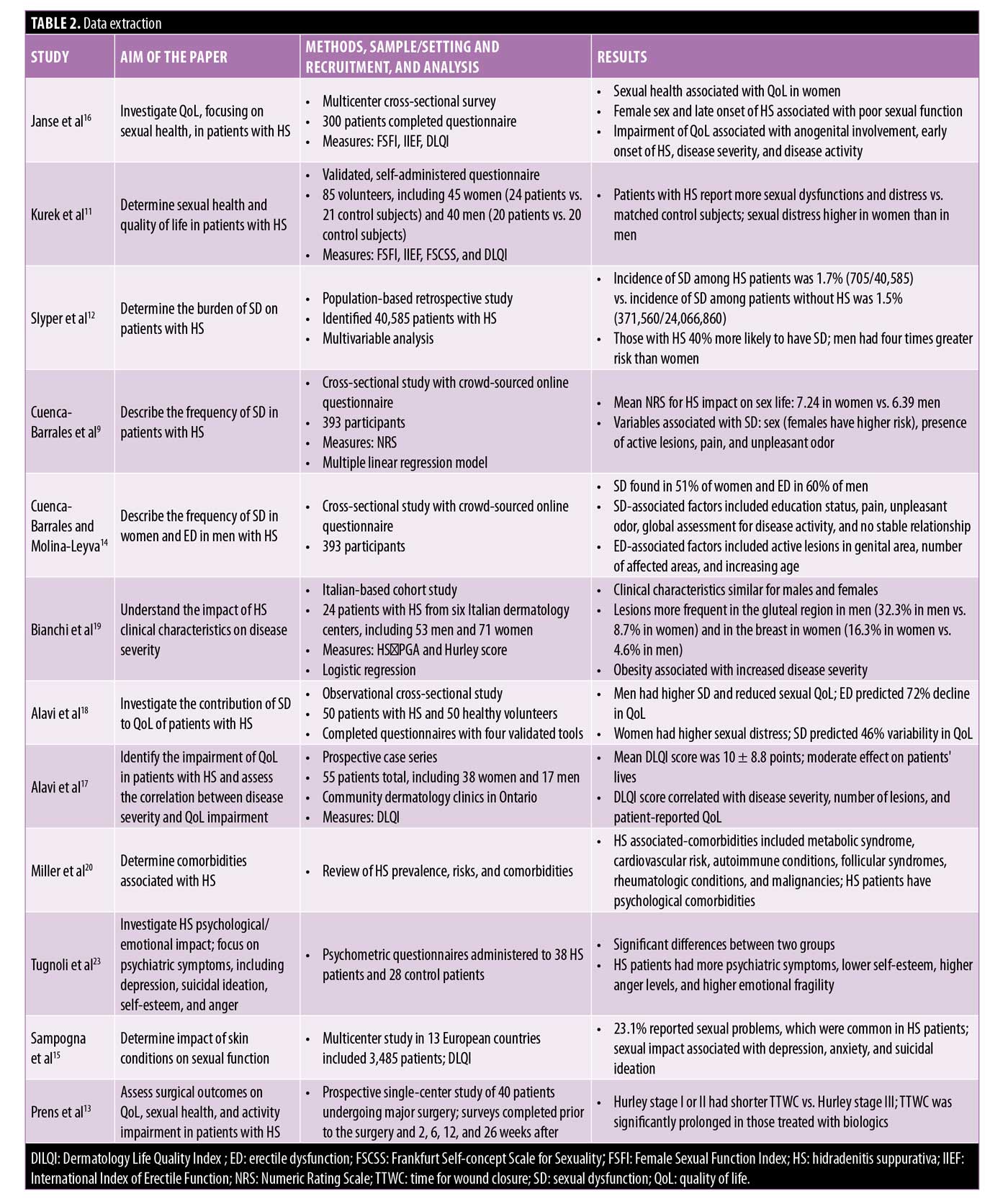
Sexual dysfunction. In a 2012 study by Kurek et al,11 validated, self-administered questionnaires were used to evaluate the sexual health and QoL of 85 voluntary participants with HS, including 45 women (24 patients vs. 21 control subjects) and 40 men (20 patients vs. 20 control subjects).11 The FSFI and IIEF, along with the Frankfurt Self-concept Scale for Sexuality, were applied to assess sexual health; QoL was measured with the Dermatology Life Quality Index (DLQI).11 This was one of the first studies to show that patients with this condition have a greater likelihood of SD and sexual distress compared to matched control subjects; furthermore, sexual distress was higher in women than in men. Slyper et al12 conducted a population-based retrospective study in 2018 to determine the burden of SD in patients with HS. They identified 40,585 patients with HS, with 75.6 percent being women between the ages of 18 and 44 years; the incidence of SD in the HS group was 1.7 percent (705/40,585) compared to 1.5 percent (371,560/24,066,860) in those without HS.12 Multivariable analysis showed that those with HS had roughly a 40-percent increase in the odds of experiencing SD, with men’s chance being nearly four times higher than that of women.12
In a 2019 prospective single-center study, Prens et al13 examined surgical outcomes and their effect on QoL, sexual health, and activity impairment in 40 patients with HS undergoing surgery. Patients had shorter times for wound closure with Hurley Stage I or II compared to Hurley Stage III, with this time significantly prolonged in those treated with biologics.13 However, major surgery did improve the overall work and daily activity impairment, resulting in enhanced QoL, including sexual health, in these patients.13
Sexual distress. In a 2019 cross-sectional study by Cuenca-Barrales et al,9 researchers aimed to describe the frequency of sexual distress in patients with HS, examining any epidemiological and clinical factors that might be associated with this condition. There were 393 participants questioned, with sexual distress evaluated using a Numeric Rating Scale (NRS) for HS impact on sex life; the mean NRS for HS impact on sex life was 7.24 in women and 6.39 in men, which was statistically significant.9 Sex, the presence of active lesions, pain, and unpleasant odor were variables connected with SD, with women showing a greater risk than men.9 However, a crucial protector factor was being in a stable relationship.
These findings were corroborated in a later study by Cuenca-Barrales and Molina-Leyva,14 which aimed to describe the frequency of SD in women and that of erectile dysfunction (ED) in men with HS, examining potential risk factors; these authors found that SD occurred in 51 percent of women and ED in 60 percent of men, respectively.14 Factors associated with SD included education status, pain, odor, global assessment for disease activity, and lack of a stable relationship, while those correlated with ED were active lesions in the genital area, number of affected areas, and increasing age.14
Sexuality. In the 2017 study by Sampogna et al,15 information on the sexual impact of several skin conditions, including HS, was collected in 13 European countries. There were 3,485 patients surveyed, of which 23.1 percent reported sexual problems; these issues were extremely common in patients with HS. Sexual impact was also strongly associated with depression, anxiety, and suicidal ideation.15 Therefore, nearly one-quarter of patients with this condition admitted to experiencing sexual issues, which are linked with psychological comorbidities.
QoL. The multicenter cross-sectional survey study by Janse et al16 examined QoL, focusing on sexual health, in patients with HS; 300 patients completed the questionnaire, with FSFI, IIEF, and DLQI used as measures to determine sexual health and dysfunction as well as QoL. These authors found that sexual health was only associated with QoL in women, with female sex and late onset of HS linked with poor sexual function; among those who had reduced QoL, greater disease severity and activity were noted.16 Elsewhere, Alavi et al17 used a prospective case series in 2015 to identify the impairment of QoL in patients with HS, evaluating the correlation between disease severity and QoL impairment; they found that disease severity and the number of lesions each participant had related to their self-reported QoL score.17
Another observational cross-sectional study on QoL by Alavi et al18 was conducted a few years later to investigate the contribution of SD to QoL in patients with HS, exploring the extent to which sexual health predicts their QoL. Questionnaires using four validated tools were used to collect the responses of 50 patients with HS and 50 healthy volunteers. They found that, relative to the control group, men experienced greater SD and reduced sexual QoL, with ED predicting a 72-percent decline in QoL; women reported higher levels of sexual distress, with SD predicting a 46-percent variability in QoL score.18 This indicates that sexual functioning disruptions significantly contribute to reduced QoL in patients with HS.
Comorbidities. In an Italian-based cohort study by Bianchi et al,19 the aim was to understand the impact of clinical characteristics of HS on disease severity; 124 patients (53 men and 71 women) with HS from six Italian dermatology centers participated, with disease severity assessed using the Hidradenitis Suppurativa Physician’s Global Assessment score and Hurley score.19 These researchers found that clinical characteristics and disease severity were similar between men and women, with lesions in men more frequently found in the gluteal region, while women had more around the breasts.19 In the 2016 study by Miller et al,20 HS was found to be associated with metabolic syndrome and greater cardiovascular risk.This was corroborated by other studies, which found that both metabolic and cardiovascular conditions were the most common comorbidities reported in these patients.21,22
There are also psychological comorbidities associated with HS. In a 2019 study by Tugnoli et al,23 the psychological and emotional impacts of HS were investigated, emphasizing psychiatric symptoms, such as depression, anger, self-esteem, and suicidal ideation.There were 38 HS patients who answered questionnaires regarding disease severity and associated conditions, with results compared to those of 28 control group patients; ultimately, the researchers found significant differences between these two groups, with HS patients displaying more psychiatric symptoms, including higher levels of anger, lower self-esteem, and greater emotional fragility.23 This association between HS and psychological comorbidities is well established, with other research showing that more than half of patients experience a large effect on QoL as measured by the DLQI.24
Tzellos and Zouboulis25 corroborated these findings in 2020, showing that HS had a huge emotional impact on patients, particularly promoting isolation due to fear of stigmatization. Body image dissatisfaction resulted in feelings of shame, embarrassment, and anxiety; this subsequently caused a lack of self-confidence, depression, and social isolation.25 Much of the shame and irritability stem from scarring and unpleasant odors that are a part of this condition, making suffers hesitant to engage in social functions, impacting their sexual health and function. Skin inflammation, physical appearance, reduced sexual desire (in both patients and their partners), and fear of passing this condition on to children were reported as reasons for SD and comorbidities related to sexual health.25
Discussion
HS is a severe dermatological condition with an unknown etiology, although hormonal and immunological causes are commonly accepted. There are both genetic and environmental factors that affect which patients are more likely to suffer from this condition, with an estimated 30-percent of patients having a family history. HS’s worldwide prevalence is between 1 and 4 percent and it is three times more likely in women than men, with the average age of onset around the early twenties. The burden of disease includes work disability, severe pain, and poor QoL; these elements typically result in psychological comorbidities, including depression, anxiety, and social stigma. A significant condition associated with HS is SD, with a high prevalence of sexual-related issues noted among these patients.
As this systematic review and meta-analysis show, HS has a substantial connection with SD and sexual distress in patients, with women more commonly experiencing SD, while men suffer from ED. These sexual impairment conditions are present in roughly half of patients with HS, which is a higher prevalence than that in the general population. In fact, those with HS have almost a 40-percent increased likelihood of suffering SD. Some reasons for this might be the presence of active lesions, extreme pain, and unpleasant odor, which can result in patients being hesitant to engage in sexual relationships; however, being in a stable relationship was shown to be a critical protector factor for women.
Sexual function’s impact on HS patients can be seen in their reduced QoL, with many displaying psychological comorbidities, including feelings of shame, anxiety, and embarrassment, resulting in a significant lack of self-confidence, social isolation, and even depression. However, there are other comorbidities related to this condition. The most common reported include both metabolic and cardiovascular comorbidities, such as increased risk for both metabolic syndromes and cardiovascular risk. These can also substantially impact sexual health, resulting in SD as well. There is still more research that must be performed, including further clinical trials and cohort studies; ample scientific evidence is required, so researchers can better understand the underlying risk factors and associated comorbidities with HS, including the impact on QoL.
References
- U.S. National Library of Medicine. Hidradenitis suppurativa.. Available at: https://ghr.nlm.nih.gov/condition/hidradenitis-suppurativa
- Vinkel C, Thomsen SF. Hidradenitis suppurativa: causes, features, and current treatments. J Clin Aesthet Dermatol. 2018;11(10):17–23.
- Napolitano M, Megna M, Timoshchuk EA, et al. Hidradenitis suppurativa: from pathogenesis to diagnosis and treatment. Clin Cosmet Investig Dermatol. 2017;10:105–115.
- Von der Werth JM, Williams HC, Raeburn JA. The clinical genetics of hidradenitis suppurativa revisited. Br J Dermatol. 2000;142(5):947–953.
- Al-Ali FM, Ratnamala U, Mehta TY, et al. Hidradenitis suppurativa (or Acne inversa) with autosomal dominant inheritance is not linked to chromosome 1p21.1-1q25.3 region. Exp Dermatol. 2010;19(9):851–853.
- Collier F, Smith RC, Morton CA. Diagnosis and management of hidradenitis suppurativa. Br Med J. 2013;346(7905):29–32.
- Revuz JE, Canoui-Poitrine F, Wolkenstein P, et al. Prevalence and factors associated with hidradenitis suppurativa: results from two case–control studies. J Am Acad Dermatol. 2008;59(4):596–601.
- Dufour DN, Emtestam L, Jemec GB. Hidradenitis suppurativa: a common and burdensome, yet under-recognised, inflammatory skin disease. Postgrad Med J. 2014;90(1062):216–220.
- Cuenca-Barrales C, Ruiz-Villaverde R, Molina-Leyva A. Sexual distress in patients with hidradenitis suppurativa: a cross-sectional study. J Clin Med. 2019;8(4):532.
- American Psychiatric Association. Sexual dysfunctions. In: Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association Publishing; 2013.
- Kurek A, Peters EM, Chanwangpong A, et al. Profound disturbances of sexual health in patients with acne inversa. J Am Acad Dermatol. 2012:67(3):422–428.
- Slyper M, Strunk A, Garg A. Incidence of sexual dysfunction among patients with hidradenitis suppurativa: a population-based retrospective analysis. Brit J Dermatol. 2018;179(2):502–503.
- Prens LM, Huizinga J, Janse IC, Horváth B. Surgical outcomes and the impact of major surgery on quality of life, activity impairment and sexual health in hidradenitis suppurativa patients: a prospective single centre study. J Eur Acad Dermatol Venereol. 2019;33(10):1941–1946.
- Cuenca-Barrales C, Molina-Leyva A. Risk factors of sexual dysfunction in patients with hidradenitis suppurativa: a cross-sectional study. Dermatol. 2020;236(1):1–9.
- Sampogna F, Abeni D, Gieler U, et al. Impairment of sexual life in 3,485 dermatological outpatients from a multicentre study in 13 European countries. Acta Derma Venereol. 2017;97(4):478–482.
- Janse IC, Deckers IE, van der Maten AD, et al. Sexual health and quality of life are impaired in hidradenitis suppurativa: a multicentre cross-sectional study. Brit J Dermatol. 2017;176(4):1042–1047.
- Alavi A, Anooshirvani N, Kim WB, et al. Quality-of-life impairment in patients with hidradenitis suppurativa: a Canadian study. Am J Clin Dermatol. 2015;16(1):61–65.
- Alavi A, Farzanfar D, Rogalska T, et al. Quality of life and sexual health in patients with hidradenitis suppurativa. Int J Women’s Dermatol. 2018;4(2):74–79.
- Bianchi L, Caposiena RD, Ganzetti G, et al. Sex-related differences of clinical features in hidradenitis suppurativa: analysis of an Italian-based cohort. Clin Exp Dermatol. 2019;44(5):e177–e180.
- Miller IM, McAndrew RJ, Hamzavi I. Prevalence, risk factors, and comorbidities of hidradenitis suppurativa. Dermatol Clin. 2016;34(1):7–16.
- Cartron A, Driscoll MS. Comorbidities of hidradenitis suppurativa: a review of the literature. Int J Women’s Dermatol. 2019;5(5):330–334.
- Dessinioti C, Katsambas A, Antoniou C. Hidradenitis suppurrativa (acne inversa) as a systemic disease. Clin Dermatol. 2014;32(3):397–408.
- Tugnoli S, Agnoli C, Silvestri A, et al. Anger, emotional fragility, self-esteem, and psychiatric comorbidity in patients with hidradenitis suppurative/acne inversa. J Clin Psychol Med Settings . 2020;27(3):527–540.
- Von der Werth JM, Jemec GB. Morbidity in patients with hidradenitis suppurativa. Brit J Dermatol. 2001;144(4):809–813.
- Tzellos T, Zouboulis CC. Review of comorbidities of hidradenitis suppurativa: Implications for daily clinical practice. Dermatol Therapy. 2020;10(1):63–71.

