 J Clin Aesthet Dermatol. 2021;14(1):24–26.
J Clin Aesthet Dermatol. 2021;14(1):24–26.
by Bruna Souza Felix Bravo, MD; Camila Roos Mariano da Rocha, MD; Leonardo Gonçalves Bravo, MD; Raquel de Melo Carvalho, MD; and Lucia Joffily, MD
Drs. B. S. F. Bravo, Mariano Da Rocha, L. G. Bravo, and De Melo Carvalho are Clínica Bravo in Rio de Janeiro, Brazil. Dr. Joffily is with Universidade Federal do Estado do Rio de Janeiro in Rio de Janeiro, Brazil.
FUNDING: No funding was provided for this article.
DISCLOSURES: The authors report no conflicts of interest relevant to the content of this article.
ABSTRACT: Nonsurgical rhinoplasty is a good treatment choice when surgery is not a viable option. However, serious complications, including blindness or cerebral ischemia, can occur given this area is one of external and internal carotid anastomosis. Here, we describe a case of a patient with a septum ulcer secondary to local ischemia postnasal filling with hyaluronic acid without skin lesion. Due to the rarity of the condition, her diagnosis was made late, but she was treated with hyaluronidase and showed total resolution.
KEYWORDS: Hyaluronidase, fillers, liquid rhinoplasty, septum ulcer
Hyaluronic acid is a widely popular dermal filler as a result of its safety profile. Recently, there has been an increase in the number of facial areas treated with the various types of hyaluronic acid filler. Nonsurgical rhinoplasty using hyaluronic acid filler has demonstrated satisfactory outcomes with little to no down time.2
Filler-augmentation rhinoplasty is a quick, nonsurgical procedure that can produce outcomes comparable to those of open rhinoplasty surgery. However, the increased frequency of vascular complications has emerged as an important issue.3 Moreover, because this is an area of external and internal carotid anastomosis, the complications related to this procedure may be significant and may even cause blindness or cerebral ischemia.4 Other complications, such as skin ischemia, have also been reported.5,6 Medical injectors should strive for early recognition and treatment of complications.
In this paper, we describe a case of a septal ulcer secondary to local ischemia postnasal filling with hyaluronic acid without skin lesions.
Case Report
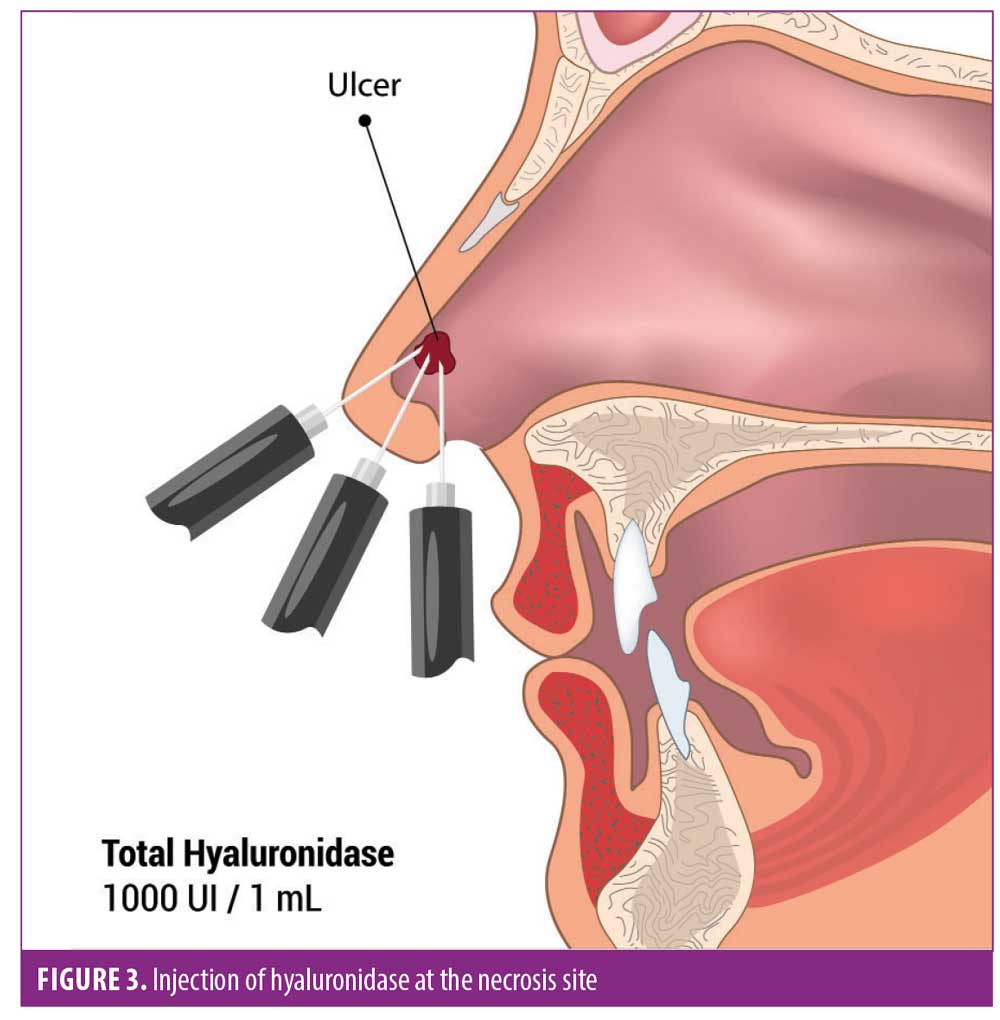
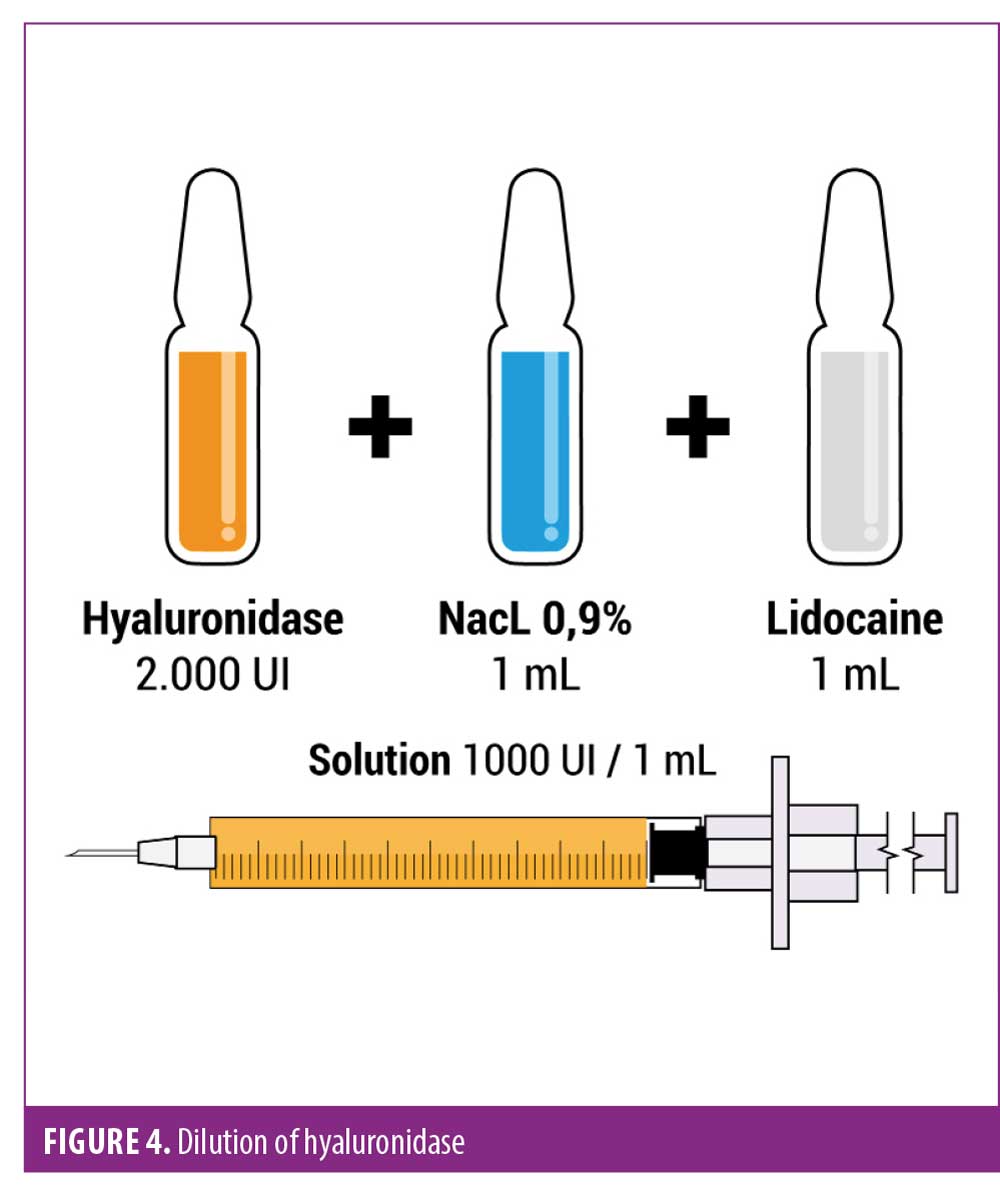
A 29-year-old, healthy female patient underwent nasal filling with hyaluronic acid for aesthetic purposes. She was not able to report the technique or product used. On the same day, after the procedure, she experienced rhinorrhea and mild burning in the nose. Then, one day after, she developed intense pain in the treated area and visited an emergency service, where a computed tomography scan was requested that showed no signs of sinusitis (Figure 1). She had normal blood test results and was medicated with oral prednisolone 40 mg/day for five days. Despite this, she experienced worsening pain, which began to radiate to the upper alveolar ridge and dental arch. She was seen by an otorhinolaryngologist, who diagnosed a septal ulcer through clinical examination and nasal endoscopy (Figure 2). The possibility of an adverse event after the hyaluronic acid injection became an hypothesis, and an evaluation by a dermatologist was requested. The physical examination showed no lesion on the skin, but there was a septal ulcer. With the hypothesis of necrosis by arterial occlusion following injection of hyaluronic acid, hyaluronidase treatment was proposed (2,000 IU dilution to 1mL of 2% lidocaine and 1mL of 0.9% NacL, totaling 1,000 IU/mL) (Figure 3). A total of 1,000 IU was delivered at three points around the ulcer with a 1-mL 30-gauge syringe (Becton, Dickinson and Co., Franklin Lakes, New Jersey) (Figure 4). The patient reported an almost immediate improvement in her pain level and progressive improvement of the lesion over the following days.

Discussion
The tip and the nasal dorsum are the two most common areas of the nose involved in dermal fillers to the nasal area.4 To increase the prominence of the nasal tip, filler is usually applied to the nasal crest, in order to support the area. In dorsum corrections, the filler is applied along the nasal dorsum, correcting asymmetries of the nose.4
Topographically, the nose extends inferiorly from the forehead and can be divided into three sections. The upper third is formed by the nasal bones and the frontal process of the maxilla, the middle third is formed by the lateral processes of the septal cartilage paired, and the lower third is formed by the inferior nasal spine, part of the maxillary bone process, and by the larger wing cartilages that have three components: a medial branch, a middle branch, and a lateral branch. The piriform, interalar ligaments, and elastic fibers connect the cartilages to each other.8
The nose is predominantly supplied by branches of the facial artery. The columella, alae, and vestibule receive branches from the superior labial artery. The remainder of the nose receives its blood supply predominantly from branches of the angular artery as it passes superiorly along the nasofacial sulcus. At the medial canthus, the angular artery anastomoses with the dorsal nasal artery, which is a branch of the ophthalmic artery.9
The most common complication of hyaluronic acid fillers is skin necrosis. Recognition of the onset of ischemia, the most dangerous complication, is critical. Signs of paleness, livedo reticularis, and/or local pain during or immediately after the procedure should be treated immediately with hyaluronidase application.2
In this case, it seems that the patient was treated with an injection in the area of the nasal crest, progressing to show symptoms of local ischemia on the same day and, subsequently, an ulcer in the area of the septum. Based on her clinical presentation, the involved artery was probably the collumelar artery, a branch of the superior labial artery. These cases are usually well managed when diagnosed early. In this case, the injection of hyaluronidase at the site was chosen, with an almost immediate reversal of pain and progressive improvement of the septal lesion experienced by the patient posttreatment. It is very important that injectors be trained in anatomy, indication, injection technique, and possible complications so that a rapid diagnosis and immediate yet safe treatment can be performed.
Conclusion
Hyaluronic acid filler injection in the nasal area is a procedure that should be performed by an experienced physician. Adverse events include tissue necrosis, amaurosis and cerebral ischemia. We report a case of septal ulcer without skin lesion. The patient was not diagnosed by the dermatologist who performed the procedure because she had no skin alterations. This is the first case we have encountered of an ischemic event after a nasal aesthetic injection by needle, injected through the skin, with no skin alteration.
It is important to emphasize that a multidisciplinary approach is extremely relevant for early diagnosis and resolution of this ischemic condition. It is important for the injector to have hyaluronidase at hand and to know how to inject it when necessary to resolve complications.
References
- Augusto GG, Shiro T, Serra GG, et al. Aesthetic comparison of the ideal nasal radix height in a Brazilian population. Braz J Otorhinolaryngol. (Impr). 2011;77(3):334–340. Article in Portuguese.
- Wang LL, Friedman O. Update on injectables in the nose. Curr Opin Otolaryngol Head Neck Surg. 2017;25(4):307–313.
- Jung GS, Chu SG, Lee JW, et al. A safer non-surgical filler augmentation rhinoplasty based on the anatomy of the nose. Aesthetic Plast Surg. 2019;43(2):447–452.
- Bravo BSF, Bravo LG, Mariano Da Rocha C, et al. Evaluation and proportion in nasal filling with hyaluronic acid. J Clin Aesthet Dermatol. 2018;11(4):36–40.
- Bachmann F, Erdmann R, Hartmann V, et al. The spectrum of adverse reactions after treatment with injectable fillers in the glabellar region: results from the Injectable Filler Safety Study. Dermatol Surg. 2009;35 Suppl 2:1629–1634.
- Bravo BSF, Klotz De Almeida Balassiano L, Mariano Da Rocha, et al. Delayed-type necrosis after soft-tissue augmentation with hyaluronic acid. J Clin Aesthet Dermatol. 2015;8(12): 42–47.
- Klotz De Almeida Balassiano L, Bravo BSF. Hyaluronidase: a necessity for any dermatologist applying injectable hyaluronic acid. Surg Cosmet Dermatol. 2014;6(4):33843.
- Neligan PC. Analysis and nasal anatomy. In: Warren R, Neligan P. Plastic Surgery. 3rd ed. Philadelphia, PA: Elsevier; 2012: 373–386.
- Oliphant TJ, Langtry JAA. Nasal anatomy for the dermatological surge-on. Br J Dermatol. 2014;171 Suppl 2:2–6.
- Furtado IR. Nasal morphology—harmony and proportion applied to rhinoplasty. Rev Bras Cir Plást. 2016;31(4):599–608. Article in Portuguese.

