J Clin Aesthet Dermatol. 2018;11(9):32–36
by Mara Weinstein Velez, MD; Omer Ibrahim, MD; Kathleen Petrell, BS; and Jeffrey S. Dover, MD, FRCPC
Dr. Weinstein Velez, Dr. Ibrahim, Ms. Petrell, and Dr. Dover are with SkinCare Physicians in Chestnut Hill, Massachusetts.
Funding: Funding provided by Syneron Medical.
Disclosures: The authors have no conflicts of interest relevant to the content of this article.
Abstract: Objective.Noninvasive fat reduction has become increasingly popular. This study evaluated the outcomes of multiple treatments with a nonthermal focused ultrasound device for the noninvasive removal of excess abdominal fat.
Design. Participants underwent a total of three pulsed, focused ultrasound treatments spaced two weeks apart.
Setting. This study took place in an outpatient dermatology office in a suburb of a major city.
Participants. Ten healthy female subjects between 18 and 60 years of age with an abdominal thickness of at least 0.6cm and body mass index between 22 and 30kg/m2 were included.
Measurements.Fat layer thickness was measured by ultrasound imaging and skin caliper and was compared with baseline at the four-, eight-, and 12-week follow-up visits after the final treatment session.
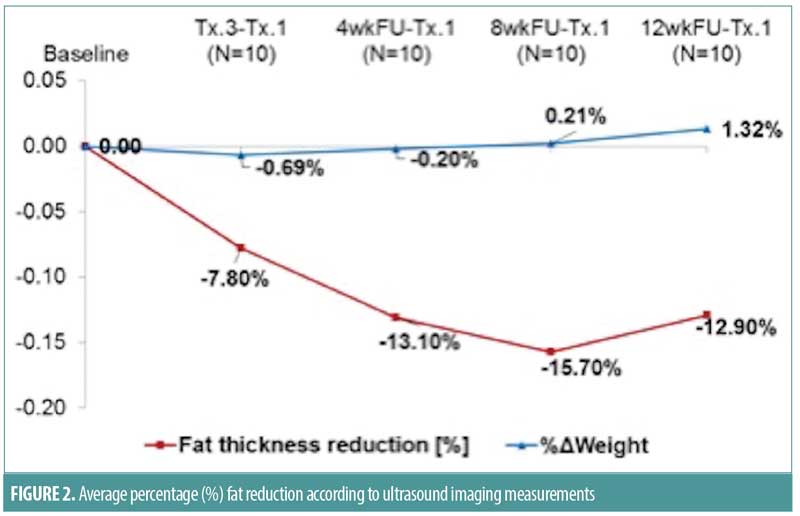
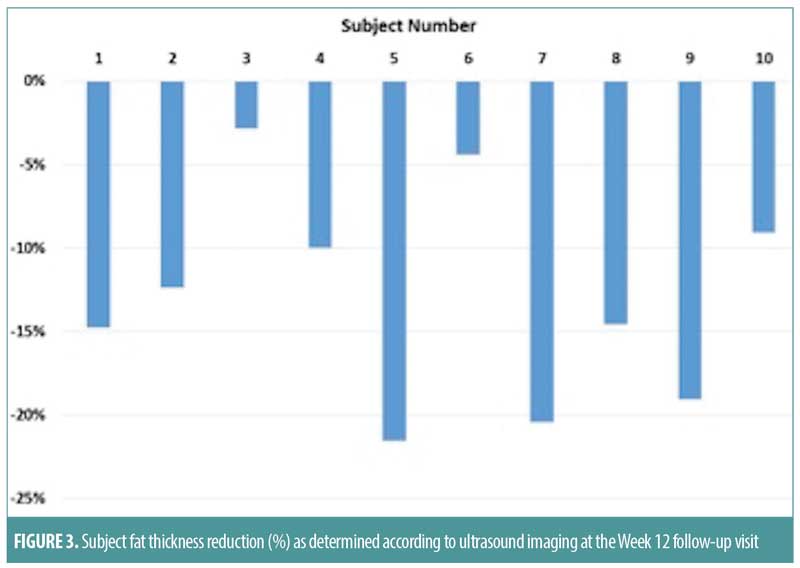
Results.The study subjects underwent a total of 30 treatment sessions. Ultrasound imaging of the targeted fat layer decreased significantly by 13, 16, and 13 percent at the four-, eight-, and 12-week follow-up time points, respectively, while measurements of the fat layer as performed by skin caliper decreased by 12, 10, and 13 percent, respectively. All subjects noted improvement, while investigators noted significant improvement and expressed high satisfaction from the ultrasound treatment outcomes at the final visit. Treatments were well tolerated and no adverse events were recorded during the study period.
Conclusion. Nonthermal pulsed focused ultrasound appears to be a safe and effective treatment option for the noninvasive removal of unwanted abdominal fat deposits.
ClinicalTrials.gov: NCT02700152
Keywords: Nonthermal pulsed ultrasound fat reduction, noninvasive fat loss, noninvasive fat treatment
Introduction
Fat reduction and body contouring procedures have become popular commodities in aesthetic surgery today. Several different treatment modalities are currently being used to safely reduce the volume of subcutaneous fat deposits and help patients achieve a more desirable body shape and contour.1 Although more invasive surgical procedures such as liposuction and abdominoplasty are still considered the gold standard treatment approaches for fat reduction and improving body silhouette, they are also associated with the inherent risks of surgery, unsightly scar tissue, postoperative pain and discomfort, and prolonged recovery times.2–5 The limitations of these cosmetic surgical procedures for aesthetic fat reduction in part have helped to popularize more noninvasive techniques and treatment approaches among potential cosmetic patients.
Ongoing research has led to the development of numerous energy-based technologies, such as cryolipolysis,7 laser and light therapy,8 and radiofrequency and ultrasound,9–25 that have been successfully used for the noninvasive reduction of unwanted fat deposits. These modalities for fat reduction and improvement in body contouring represent a potential treatment alternative for patients in whom surgical procedures are contraindicated or in those who desire minimal downtime.
Numerous clinical trials have demonstrated the positive clinical outcomes achieved with a nonthermal pulsed focused ultrasound system (UltraShape; Syneron Medical Ltd., Yokneam, Israel) used for the noninvasive treatment of excess and unwanted subcutaneous fat deposits.17,22–25 The goal of the present prospective pilot study was to evaluate the safety, efficacy, and tolerability of a pulsed focused ultrasound device for the noninvasive removal of unwanted excess abdominal fat deposits and the improvement of body image.
Materials and Methods
Device specifics. The focused ultrasound system used in this study was cleared by the United States Food and Drug Administration (FDA) for the noninvasive reduction of abdominal circumference and fat reduction in the flanks and thighs. Focused pulsed ultrasound technology reduces fat via mechanical disruption, destruction, and natural sequestration of the targeted adipocytes. The system emits acoustic sound waves of ultrasonic energy (200KHz±30KHz frequency) that converge into a confined focal volume at a depth of 1.5cm below the skin’s surface, targeting the subcutaneous fat at a controlled depth. Unlike traditional ultrasound technology, the ultrasound technology used in this study transmits bursts of pulsed ultrasonic energy, allowing for precise control over temperature elevation (i.e., less than a 0.5°C increase) and enabling mechanical (nonthermal) fat destruction at a focal point in the subcutaneous fat layer to occur instantly and selectively. The selective destruction of the adipocytes should circumvent any collateral damage and trauma to the surrounding tissue structures, such as blood vessels, connective tissue, lymphatic vessels, muscles, and nerves. During treatment, focused ultrasound is designed to cause rapid changes in pressure and creates bubbles in the interstitial fluid found between the adipocytes in the targeted area. These bubbles subsequently implode from the quick pressure changes, causing rupture of the adipocyte walls and ultimate death of the targeted fat cells. The released triglycerides and cellular debris from the destroyed adipocytes are then processed by the body’s physiological and metabolic pathways and removed from the body.
The focused ultrasound system is equipped with both a large Vertical Dynamic Focus™ (VDF) transducer and a smaller, 12-gram U-Sculpt transducer to target anatomical locations of various dimensions. The therapeutic ultrasonic transducer delivers the focused ultrasound energy beam, while real-time optical and acoustic feedback during treatment is provided via the tracking and guidance system, ensuring that the treatment is performed only within the designated area in a homogenous and controlled manner. The focused ultrasound system has two treatment modes available: the single-focus deep mode and the super mode. The procedure does not require the patient to be anesthetized, lasts approximately 45 to 60 minutes, and can be performed in an office setting.
Study design. This was a prospective, single-arm, baseline-controlled pilot study for the evaluation of the focused ultrasound treatment for noninvasive abdominal fat reduction. Ten healthy subjects between the ages of 18 and 60 years were recruited. The abdominal thickness, measured by a calibrated caliper, was required to be at least 0.6cm in the treated area, and body mass index (BMI) of the participants needed to be between 22 and 30kg/m2. Exclusion criteria included previous body contouring procedures in the treatment area of the abdomen within 12 months of the study; abdominal wall diastasis or hernia at the time of physical exam; or current pregnancy or childbirth in the prior 12 months. All subjects met the inclusion/exclusion criteria and signed an informed consent prior to the initiation of the clinical study. This study was approved by the Massachusetts Institutional Review Board, and was conducted in compliance with the Declaration of Helsinki.
Using the U-Sculpt/VDF transducer in single-pass mode, study participants with appreciable localized subcutaneous fat in the abdominal region underwent three treatments with the pulsed focused ultrasound system spaced by two-week intervals and were followed up at four, eight, and 12 weeks after the final treatment session. At each treatment visit and every posttreatment follow-up session, abdominal thickness was measured by pink caliper and ultrasound imaging measurements were taken at four locations above and below the abdominal midline (umbilicus); these were then averaged to provide a value (in millimeters) for the fat layer thickness from the dermis to the bottom of the subcutaneous fat layer.
At each treatment visit, study subjects rated treatment discomfort using a numerical scale response scale ranging from 0 to 10, where 0=no pain and 10=worst possible pain. At the 12-week follow-up visit, the investigator also completed a questionnaire, rating satisfaction with treatment outcomes using a five-point scale ranging from -2 to 2, where -2=very dissatisfied and 2=very satisfied. Clinical photographs were taken and subject circumferences were measured at baseline and at each follow-up visit. All clinical photographs were taken with a digital camera system on a tripod. The same photographer was used for consistency. Treatment safety was assessed by the frequency, severity, and type of adverse events that occurred.
Results
Ten female subjects completed the study. Baseline characteristics included a mean age of 52 years (range: 39–60 years), Fitzpatrick skin types ranged from I to IV and participants had a mean weight of 66kg (range: 55–75kg), a mean BMI of 24 (range: 22–29kg/m2), and a mean abdominal thickness of 1.90cm (range: 1.50–3.50cm) as measured by caliper. All 10 subjects underwent a total of three treatments with the focused ultrasound system performed every two weeks on the targeted abdominal region. Ultrasound imaging demonstrated that the thickness of the fat layer decreased by 2.6mm (13.1%), 3.2mm (15.7%), and 2.8mm (12.9%) at the four-, eight-, and 12-week follow-up visits, respectively (Figures 1–4). Additionally, the midline abdominal circumference measurements decreased by 4.1mm, 7.2mm, and 5.6mm at the four-, eight-, and 12-week follow-up visits, respectively. The fat layer thickness according to skin caliper measurements also decreased at the same follow-up time points by 12.4, 9.7, and 12.8 percent, respectively. Of note, subjects maintained stable weights throughout the entire follow-up period.

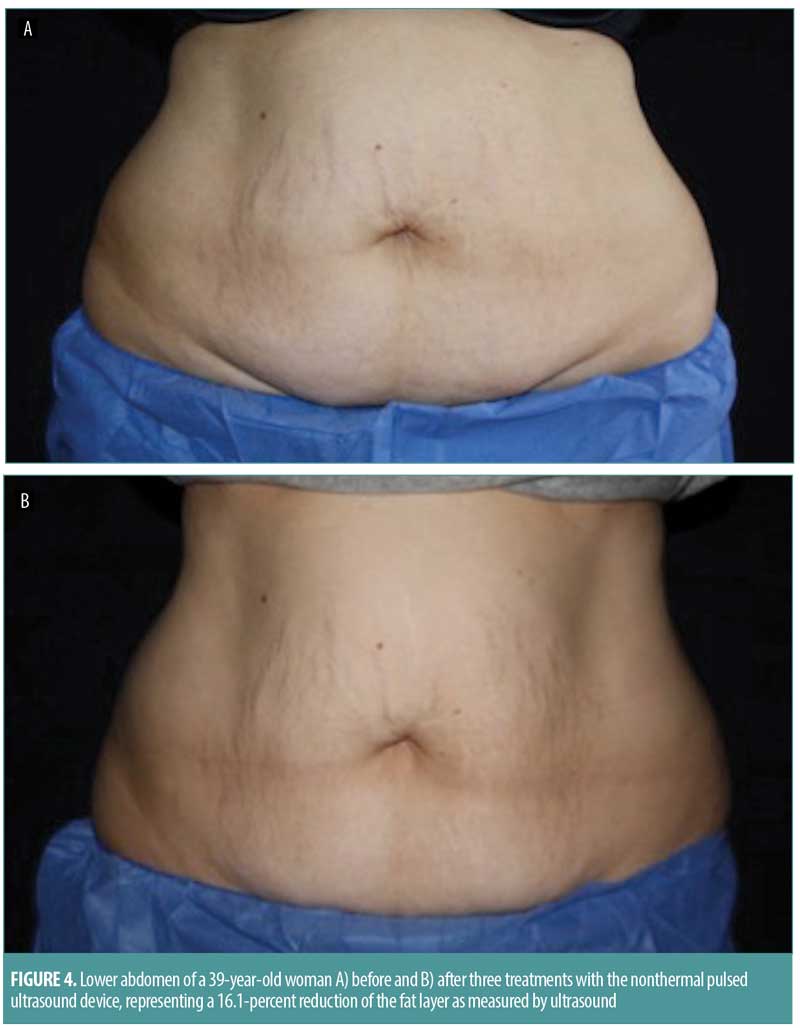
The investigator satisfaction questionnaire demonstrated an average score of 1.8 at the 12-week follow-up visit. Patients were satisfied with their treatments, reporting good tolerability with ratings of “none to minimal” discomfort during the first two treatments (average NSR scores of 0.3 and 0.4, respectively), and “no pain” (100% of subjects) during the third treatment. There were no immediate skin reactions following treatments, and none of the subjects reported adverse events throughout the duration of the study.
Discussion
Noninvasive fat reduction procedures have become popular in aesthetic medicine as they offer patients the chance for significant reductions in targeted fat deposits while circumventing the risks and side effects of invasive surgical procedures. The pulsed focused ultrasound system is an innovative technology that delivers bursts of pulsed focused ultrasound to nonthermally, immediately, and selectively destroy targeted subcutaneous fat cells without surgery, discomfort, or downtime. The outcomes of the present clinical pilot study suggest that treatment with the pulsed focused ultrasound system is safe, efficacious, and tolerable for aesthetic fat reduction in the abdominal region.
Previous clinical studies have demonstrated similar efficacy and safety of the pulsed focused ultrasound system in different anatomic locations, including the abdomen, thigh, and flank regions.17,19–20,22–25 One multicenter clinical study showed that a single treatment performed on the abdomen, thighs, and flanks led to an average reduction of approximately 2cm in the treatment area circumference at two weeks after the treatment session, with the results maintained at the 12-week follow-up visit.23 Study subjects reported very high satisfaction and tolerability following treatment. In another multicenter clinical study, 150 healthy male and female subjects presenting with excess subcutaneous fat deposits in the abdominal region were randomly assigned to Group 1, where they underwent a four-week control phase before undergoing three abdominal fat reduction treatments with the device at two-week intervals, or to Group 2 for immediate treatment.24 The study design included the collection of weight, abdominal circumference, treatment tolerability, and satisfaction levels of the participants, as well as data on any adverse events that occurred during the study period. Results showed that the average reduction in the midline circumference was 2.5cm±2.1cm in Group 1 and 3.5cm±2.7cm in Group 2 at the final follow-up visit at Week 22. In addition, the effect of multiple treatments was found to be cumulative, as a trend for a steady decrease in abdominal circumference throughout the study was observed. The authors suggested that successive focused ultrasound treatments can significantly reduce treatment area circumference while allowing for patients to circumvent invasive techniques and their associated disadvantages.
Comparable technologies for localized fat destruction with minimal downtime include lasers, high-intensity focused ultrasound, radiofrequency devices, and selective cryolipolysis. Each of these treatment modalities varies in terms of their individual mechanism, efficacy, and safety profile. Research by Decorato et al26 demonstrated that a single treatment with an 1,060-nm diode laser on the flanks resulted in an average fat reduction of 13 percent at the six-week follow-up, which was maintained at 12 weeks. Bass and Doherty27 found a 16-percent reduction in fat thickness of the abdomen at 12 weeks posttreatment. Side effects of the diode laser include discomfort during treatment, burns, temporary nodules, and prolonged tenderness.27 In a separate pilot study comparing hyperthermic laser lipolysis to cryolipolysis, there was no statistically significant difference in outcome when measuring fat reduction of the flanks (24%-reduction versus 22%-reduction, respectively).28 Monopolar and multipolar radiofrequency devices have demonstrated similar reductions in localized subcutaneous fat; however, these modalities also exhibit risks of erythema, tenderness, nodules, and variability in results due to operator dependence.29,30 High-intensity focused ultrasound treatment can significantly reduce fat, but these treatments can be notably uncomfortable to subjects and lead to side effects such as erythema, edema, induration, and, in rare cases, fibrosis.31,32
The lack of adverse effects noted in our study compared with other nonsurgical modalities is due in large part to the mechanism of action of the pulsed focus ultrasound system. Depending on the acoustic parameters used, ultrasound energy can induce a wide range of biological effects that can be intelligently crafted to cause positive outcomes in the targeted tissues. While low levels of ultrasound can produce beneficial but reversible cellular effects, higher levels of ultrasound energy (such as high-intensity focused ultrasound) can quickly raise the temperature of the targeted tissues, causing instantaneous coagulative cell necrosis. Using heat to achieve a desired tissue effect is the foundation of many surgical tools, including aesthetic ultrasound-based devices employed in fat reduction procedures. In stark contrast to other noninvasive technologies, however, the pulsed focus ultrasound system achieves fat cell reduction in a nonthermal fashion. Pulsed focused ultrasound energy is delivered in bursts to the targeted area, resulting in a nonthermal cavitation effect that only targets the adipose tissue in the subcutaneous fat layer while controlling the temperature elevation (i.e., less than 0.5°C increase) in the targeted tissues. The selective destruction of the adipocytes leaves the surrounding collateral tissues in the treatment area unharmed. This approach is likely in part responsible for the favorable safety profile associated with this nonthermal pulsed ultrasound system and the lack of typical adverse events associated with thermal-based treatment modalities (e.g., pain, dysesthesia, bruising, and swelling). While the results of this prospective trial demonstrate efficacy and safety of this treatment in the reduction of abdominal fat, our smaller number of subjects and absence of a control arm pose limitations to the generalizability of our findings. However, the results of this study do echo the conclusions of prior reported investigations.
Conclusion
Although smaller, single-armed, and uncontrolled, our study suggests that three nonthermal, pulsed ultrasound treatments can safely and significantly reduce abdominal fat, as measured by objective ultrasound imaging analysis. This modality might provide an attractive treatment alternative for individuals who desire nonsurgical and mostly painless abdominal fat reduction with minimal downtime and risks. Larger, controlled trials with longer follow-up periods are needed to elucidate the long-term effects of this technology.
References
- Kennedy J, Verne S, Griffith R, et al. Non-invasive subcutaneous fat reduction: a review. J Eur Acad Dermatol Venereol. 2015;29(9):1679–1688.
- Wollina U, Goldman A, Berger U, Abdel-Naser MB. Esthetic and cosmetic dermatology. Dermatol Ther. 2008;21(2):118–130.
- Commons GW, Halperin B, Chang CC. Large volume liposuction: a review of 631 cases over 12 years. Plast Reconstr Surg. 2001;108(6):1753–1763.
- Matarasso A, Swift RW, Rankin M. Abdominoplasty and abdominal contour surgery: a national plastic surgery survey. Plast Recontr Surg. 2006;117(6):1797–1808.
- Iverson RE, Lynch DJ; American Society of Plastic Surgeons Committee on Patient Safety. Practice advisory on liposuction. Plast Reconstr Surg. 2004;113(5):1478–1490.
- Dierickx CC, Mazer JM, Sand M, et al. Safety, tolerance, and patient satisfaction with noninvasive cryolipolysis. Dermatol Surg. 2013;39(8):1209–1216.
- Lee SJ, Jang HW, Kim H, et al. Non-invasive cryolipolysis to reduce subcutaneous fat in the arms. J Cosmet Laser Ther. 2016;18(3):126–129.
- Katz B, Doherty S. Safety and efficacy of a noninvasive 1,060-nm diode laser for fat reduction of the flanks. Dermatol Surg. 2018;44(3):388–339.
- Weiss RA. Noninvasive radiofrequency for skin tightening and body contouring. Semin Cutan Med Surg. 2013;32(1):9–17.
- Adatto MA, Adatto-Neilson RM, Morren G. Reduction in adipose tissue volume using a new high-power radiofrequency technology combined with infrared light and mechanical manipulation for body contouring. Lasers Med Sci. 2014;29(5):1627–1631.
- Brightman L, Weiss E, Chapas AM, et al. Improvement in arm and post-partum abdominal and flank subcutaneous fat deposits and skin laxity using a bipolar radiofrequency, infrared, vacuum and mechanical massage device. Lasers Surg Med. 2009;41(10):791–798.
- Winter ML. Post-pregnancy body contouring using a combined radiofrequency, infrared light and tissue manipulation device. J Cosmet Laser Ther. 2009;11(4):229–235.
- Boisnic S, Divaris M, Nelson AA, et al. A clinical and biological evaluation of a novel, noninvasive radiofrequency device for the long-term reduction of adipose tissue. Lasers Surg Med. 2014;46(2): 94–103.
- Fritz K, Salavastru C. Long-term follow-up on patients treated for abdominal fat using a selective contactless radiofrequency device. J Cosmet Dermatol. 2017;16(4):471–475.
- Fajkošová K, Machovcová A, Onder M, Fritz K. Selective radiofrequency therapy as a non-invasive approach for contactless body contouring and circumferential reduction. J Drugs Dermatol. 2014;13(3):291–296.
- Chang SL, Huang YL, Lee MC, et al. Combination therapy of focused ultrasound and radio-frequency for noninvasive body contouring in Asians with MRI photographic documentation. Lasers Med Sci. 2014;29(1):165–172.
- Moreno-Moraga J, Valero-Altés T, Riquelme AM, et al. Body contouring by noninvasive transdermal focused ultrasound. Lasers Surg Med. 2007;39(4):315–323.
- Brown SA, Greenbaum L, Shtukmaster S, et al. Characterization of nonthermal focused ultrasound for noninvasive selective fat cell disruption (lysis): technical and preclinical assessment. Plast Reconstr Surg. 2009;124(1): 92–101.
- Robinson DM, Kaminer MS, Baumann L, et al. High-intensity focused ultrasound for the reduction of subcutaneous adipose tissue using multiple treatment techniques. Dermatol Surg. 2014;40(6):641–651.
- Jewell ML, Baxter RA, Cox SE, et al. Randomized sham-controlled trial to evaluate the safety and effectiveness of a high-intensity focused ultrasound device for noninvasive body sculpting. Plast Reconstr Surg. 2011;128(1):253–262.
- Shek SY, Yeung CK, Chan JC, Chan HH. Efficacy of high-intensity focused ultrasonography for noninvasive body sculpting in Chinese patients. Lasers Surg Med. 2014;46(4):263–269.
- Ascher B. Safety and efficacy of UltraShape Contour I treatments to improve the appearance of body contours: multiple treatments in shorter intervals. Aesthet Surg J. 2010;30(2):217–224.
- Teitelbaum SA, Burns JL, Kubota J, et al. Noninvasive body contouring by focused ultrasound: safety and efficacy of the Contour I device in a multicenter, controlled, clinical study. Plast Reconstr Surg. 2007;120(3):779–789; discussion 790.
- Coleman WP, Coleman W, Weiss RA, et al. A multicenter controlled study to evaluate multiple treatments with nonthermal focused ultrasound for noninvasive fat reduction. Dermatol Surg. 2017;43(1):50–57.
- Coleman KM, Coleman WP, Benchetrit A. Non-invasive, external ultrasonic lipolysis. Semin Cutan Med Surg. 2009;28(4):263–267.
- Decorato JW, Chen B, Sierra R. Subcutaneous adipose tissue response to a non-invasive hyperthermic treatment using a 1,060?nm laser. Lasers Surg Med. 2017;49(5):480–489.
- Bass LS, Doherty ST. Safety and efficacy of a non-invasive 1060 nm diode laser for fat reduction of the abdomen. J Drugs Dermatol. 2018 Jan 1;17(1):106–112.
- Decorato JW, Chen B, Sierra R. Subcutaneous adipose tissue response to a non-invasive hyperthermic treatment using a 1,060 nm laser. Lasers Surg Med. 2017 Jul;49(5):480–489.
- Bhatia A. Subcutaneous adipocyte reduction using a non-invasive monopolar radiofrequency device. Paper presented at 2016 Annual Conference of the American Society for Laser Medicine and Surgery Meeting; March 30–April 3, 2016; Boston, Massachusetts.
- Weiss R, Weiss M, Beasley K, et al. Operator independent focused high frequency ISM band for fat reduction: porcine model. Lasers Surg Med. 2013;45:235–239.
- Jewell MI, Baxter RA, Cox SE, et al. Randomized sham-controlled trial to evaluate the safety and effectiveness of a high-intensity focused ultrasound device for noninvasive body sculpting. Plast Reconstr Surg. 2011;128(1):253–262.
- Greenshaw BN and Cook J. Painful subcutaneous fibrosis: a complication after high-intensity focused ultrasound for lipolysis. Dermatol Surg. 2015;41(6):744–759.

