 J Clin Aesthet Dermatol. 2020;13(10):45–48
J Clin Aesthet Dermatol. 2020;13(10):45–48
by James Q. Del Rosso, DO, FAAD, FAOCD
Dr. Del Rosso is Research Director at JDR Dermatology Research in Las Vegas, Nevada, is with Thomas Dermatology in Las Vegas, Nevada, and is an adjunct clinical professor of dermatology at Touro University Nevada in Henderson, Nevada.
FUNDING: No funding was provided for this publication.
DISCLOSURES: Related to this subject area, Dr. Del Rosso is a consultant, speaker, and researcher for Almirall, Mayne Pharma, and Bausch Health (Ortho Dermatology).
ABSTRACT:
Oral tetracyclines are commonly prescribed in dermatology, especially for acne. The most commonly used oral agents for acne treatment over the past several years are doxycycline and minocycline based on their overall efficacy and safety. Available for over five decades as immediate-release formulations, both of these agents exhibit broad-spectrum antibiotic activity and are primarily FDA-approved for treatment of a variety of cutaneous infections. In 2018, oral sarecycline was FDA-approved for the treatment of acne, which is the only disease state for which it was evaluated based on a narrower antibiotic spectrum of activity. This article reviews the overall antibiotic properties of commonly used oral tetracyclines with a focus on explaining the narrow spectrum of activity exhibited by sarecycline. Specifically, sarecycline has high activity against Cutibacterium acnes, the organism correlated with acne pathogenesis, as well as Staphylococci and Streptococci, with a low potential for emergence of resistant mutant bacteria based on in-vitro testing. The narrow-spectrum antibiotic designation of sarecycline relates to its negligible or low activity against many gram-negative and anaerobic bacteria. This article serves to review available data to date to assist clinicians in determining potential clinical relevance related to oral antibiotic use for acne.
Keywords: Sarecycline, narrow-spectrum antibiotic, broad-spectrum antibiotic, antibiotic resistance, microbiome
Tetracyclines (TCNs) are a class of compounds used for the treatment of a vast array of infectious and non-infectious dermatologic disorders, due to their antimicrobial activity (especially antibiotic activity), anti-inflammatory properties, or both.1–4 For the purposes of this discussion, TCNs refers specifically to four individual compounds that are administered almost exclusively as oral agents: tetracycline (TCN), doxycycline, minocycline, and sarecycline. TCN became available in the United States (US) as an oral formulation in the early 1950s, doxycycline in 1967, minocycline in 1971, and sarecycline in 2018.5 Over the past two decades, doxycycline and minocycline have progressively become the most commonly prescribed TCNs in dermatology, especially for acne and rosacea, due to greater lipophilicity, pharmacokinetic profiles, and antibiotic resistance patterns, especially for Cutibacterium acnes (formerly Propionibacterium acnes); they are also used for outpatient treatment of cutaneous methicillin-resistant Staphylococcus aureus (MRSA) infections.2,5
The broad versatility of TCNs for treatment of many skin disorders, including a wide variety of bacterial/microbial infections, has led to concerns related to increased emergence of antibiotic resistance. The concerns relate not only to C. acnes resistance, but also to the unwanted collateral antibiotic exposure of other commensal and known potential pathogenic bacteria present throughout the body, such as within skin, oral/nasopharyngeal region, genitorurinary (GU) tract, and gastrointestinal (GI) tract.6–8 Unfortunately, although not intentional, the antibiotic exposure of these other “bystander” bacteria selects for resistant strains that may be relevant to emergence of infection in the patient or in others through communicable passage of bacteria among individuals over time.
This manuscript reviews information on TCNs, with emphasis on antibiotic activity. There is focus on sarecycline, which has been categorized as a narrow-spectrum tetracycline compound, with discussion of the data supporting this concept. Although more data are needed, the reader is encouraged to consider whether they feel the information available to date is clinically relevant and how it may influence acne management.
Commonly Used Broad-Spectrum Tetracyclines: Doxycycline and Minocycline
Immediate-release formulations. Immediate-release oral formulations of doxycycline and minocycline, including those that are enterically-coated to reduce GI side effects associated with doxycycline, are primarily approved for the treatment of a variety of infections, although their most common use in dermatology is for acne and rosacea.1,2,55,9–11 Such formulations of doxycycline and minocycline, according to their United States (US) Food and Drug Administration (FDA) approved package inserts, are for treatment or prevention of infections that are proven or strongly suspected to be caused by a broad spectrum of susceptible gram-positive and gram-negative bacteria; their approved indications also includes adjunctive therapy for severe acne, which was grand-parented approval that was not based on formal new drug application (NDA) submission with large-scale pivotal clinical trials to the FDA.9–11 The available clinical studies in the literature and widespread real world experience in acne supported oral use of doxycycline and minocycline, with most patients observing clinical improvement and with a typical reduction of >50 percent inflammatory lesions after three months of use.9 A systematic review of clinical trials from 1962 through 2006 investigating oral TCNs for inflammatory acne stated that evidence was insufficient to support greater efficacy of one tetracycline agent as compared to another, no definitive dose-response correlations could be determined, and no changes in efficacy were observed over the prolonged time period that was evaluated.12
Other specialized formulations. It is important to recognize that an extended-release oral formulation of minocycline, dosed based on patient weight, is FDA-approved for acne since 2006 based on formal NDA submission to the FDA with the necessary supportive preclinical and clinical studies. The only approved indication for this extended-release formulation is for treatment of inflammatory lesions of moderate-to-severe non-nodular acne in patients 12 years of age and older.13 A biphasic release oral formulation of minocycline, available since 2019, is also FDA-approved only for the treatment of inflammatory lesions of non-nodular moderate to severe acne in patients 12 years of age and older, and not for cutaneous infections.14 Additionally, a sub-antibiotic dose of a modified-release doxycycline capsule (40mg once daily) is formally FDA-approved since 2006 based on NDA submission for the treatment of inflammatory (papulopustular) lesions of rosacea in adults, and is not FDA-approved for cutaneous infections, and is not FDA-approved for acne.15 Sub-antibiotic dosing of doxycycline may also be achieved with oral use of 20mg immediate-release tablets twice daily. However, data that suggest possible efficacy of sub-antibiotic dosing of doxycycline for acne are limited, this approach is not FDA-approved for acne therapy, and the 20mg twice daily approach is not FDA-approved for any dermatologic indication.16,17
Doxycycline and approved treatment for infections. With the exception of sub-antibiotic dosing described above, doxycycline is FDA-approved for antibiotic/antimicrobial treatment of specific infections caused by susceptible organisms, sometimes based on the organ system affected, and caused by a broad spectrum of both gram-positive and gram-negative pathogens, including from several families of bacteria.1,9,10 Sensitivity of individual organisms may vary, suggesting that the pathogen be identified and susceptibility tested if clinically possible. The types of approved infections include respiratory infections, genitourinary infections, ophthalmologic infections (i.e. trachoma), Rickettsial infections, several sexually transmitted diseases, malaria prophylaxis, and as an alternative for treatment of certain infections when penicillin is contraindicated.10 The FDA-approved package insert for immediate-release oral doxycycline formulations includes a long list of organisms that may be susceptible and amenable to treatment with doxycycline, including many aerobic and anaerobic bacteria.10
Minocycline and approved treatment for infections. With the exception of extended-release and biphasic release oral minocycline formulations, minocycline, like doxycycline, is also FDA approved as an antibiotic/antimicrobial agent for a broad spectrum of infections caused by several gram-positive or gram-negative pathogens.1,9,11 Similar to immediate-release doxycycline, the FDA-approved package insert for immediate-release oral minocycline includes a thorough list of aerobic and anaerobic bacterial organisms that may be susceptible and amenable to treatment with minocycline, with some differences in organisms listed and the types of treatable infections.11 The types of approved infections for minocycline include skin and soft tissue infections, respiratory infections, genitourinary infections, Rickettsial infections, several sexually transmitted diseases, treatment of asymptomatic nasopharyngeal carriers of Neisseria meningitidis, and as an alternative for selected infections when penicillin is contraindicated.11
Differences that address treatment selection with doxycycline or minocycline in the clinical setting for cutaneous infections, and also related to potential adverse events (AEs) have been reviewed in the literature.18,19
New Horizon of Narrow Spectrum Tetracyclines: Sarecycline
Sarecycline is an oral aminomethylcycline compound in the tetracycline family that entered the US marketplace in 2018 with FDA approval for the treatment of inflammatory lesions of non-nodular moderate to severe acne vulgaris (AV) in patients nine years of age and older.20 Unlike immediate-release doxycycline and minocycline, sarecycline was not evaluated for and is not FDA approved for the treatment of cutaneous infections. Nevertheless, the microbiologic profile of sarecycline has been studied, leading to the designation of this agent as a narrow spectrum tetracycline. This narrow spectrum designation is based on sarecycline exhibiting a diminished diversity of antibiotic activity, especially against gram-negative bacterial organisms, with a more targeted antibiotic profile, including high activity against C. acnes.21-23 Modifications of the basic tetracycline chemical moiety at the C7 and C9 positions were incorporated in the structural development of sarecycline to overcome bacterial resistance mechanisms including ribosomal protection and efflux pumps.22,24 The modes of action of TCNs are reviewed in more detail elsewhere, including both antibiotic mechanisms, biologic/anti-inflammatory properties, and bacterial resistance pathways.1–4,9,22,25,26
The FDA approval of sarecycline for inflammatory acne treatment in patients nine years of age and older demonstrated efficacy, along with a highly favorable safety profile that included evaluation of over 2000 acne patients treated in randomized, controlled trials (RCTs).23,25,27 Although primary evaluations of efficacy were based on responses in facial acne, data were also collected in truncal acne based on global assessments.26,26 Most of the AEs noted with a numerically greater incidence with sarecycline versus placebo in the two pivotal Phase III trials, such as nausea, abdominal pain/discomfort, dizziness, sunburn, and vulvovaginal candidiasis/mycotic infection occurred in less than 1.5 percent of subjects on sarecycline; vomiting was reported in 2.1 percent of sarecycline subjects and in 1.4 percent of placebo recipients.27 The low incidence of vulvovaginal candidiasis/mycotic infections reported among female subjects actively treated with sarecycline supports a minimal risk for vaginal dysbiosis.
The available data on oral sarecycline use for treatment of acne in RCTs supports both efficacy and favorable safety, including a very low incidence of AEs that are of special interest related to oral tetracyclines (i.e. GI effects, vaginal mycotic infections, photosensitivity). Ultimately, the discussion of what can define sarecycline as a narrow spectrum tetracycline is based on its microbiologic profile.
Sarecycline microbiologic profile. The potential clinical relevance of narrow spectrum antibiotic activity with sarecycline is based on the belief that this will reduce the emergence of antibiotic-resistant strains among organisms that are placed under selection pressure when exposed to sarecycline.22,23,26–29 Concern regarding the overall increase in bacterial resistance related to antibiotic therapy for acne, including alteration of the GI tract microbiome, has been discussed in the literature.7,8,18,21,22,29 It is recognized that antibiotic therapy is part of the armamentarium used to treat acne. However, it is important that efforts be made to reduce the emergence of resistant bacterial organisms.2,5,7–9,30
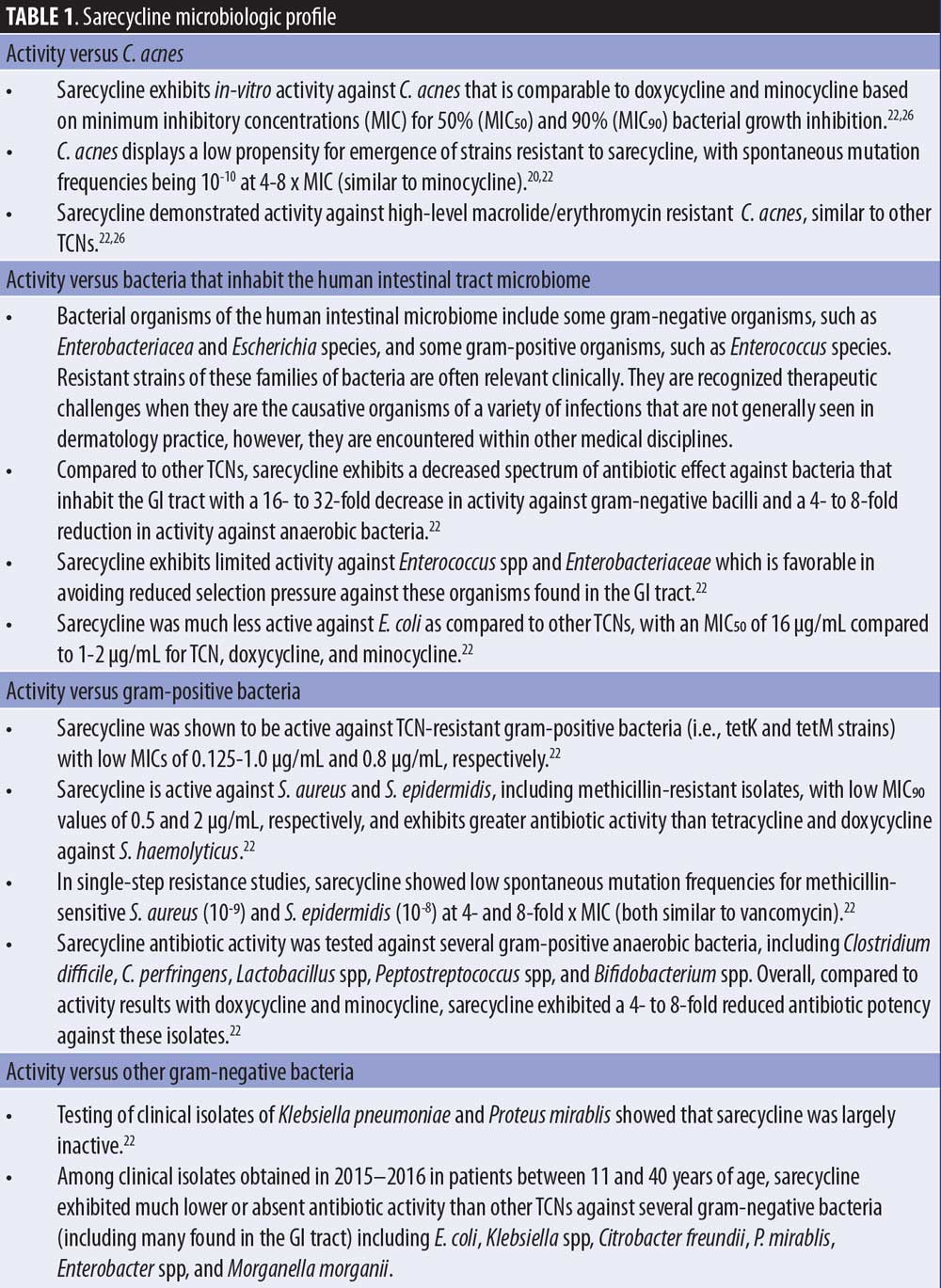
Sarecycline was developed specifically for treatment of acne due to high activity against C. acnes and lesser activity against many other bacteria as compared to other TCNs, especially doxycycline and minocycline.21,22,26 Table 1 summarizes data defining the microbiologic profile of sarecycline using a variety of standardized methods to assess antibiotic activity, which are reviewed in greater detail elsewhere.22
Can We Make Sense of This Data?
Tetracyclines have been used for antibiotic therapy in many areas of medicine due to the wide range of organisms they have been shown to treat effectively, many included in their FDA-approved indications.1,10,11 In dermatology, TCNs are frequently prescribed, mostly for inflammatory skin disorders, such as acne and rosacea, but also for cutaneous infections.2,5,9 Both doxycycline and minocycline are commonly used to treat acne, primarily due to their anti-inflammatory properties and antibiotic activity against C. acnes.1-5,9 The emergence of antibiotic resistance as a unwanted sequelae related to the prescribing of TCNs in doses that induce bacterial selection pressure continues to be an important clinical concern.2,6–9,29,30 Until the development of sarecycline, the frequently used TCNs in dermatology exhibit broad spectrum microbiologic profiles. The information reviewed here discusses the narrow antibiotic spectrum of sarecycline, supported primarily by decreased antibiotic activity against many gram-negative bacteria and also several gram-positive anaerobic organisms.22 Sarecycline was specifically developed for and formally studied for treatment of acne, receiving FDA approval for the treatment of inflammatory lesions of non-nodular moderate to severe acne vulgaris (AV) in patients nine years of age and older.20
While maintaining high antibiotic activity against C. acnes with a low propensity for emergence of resistant C. acnes isolates, the decreased antibiotic effect against many other bacteria, especially gram-negative organisms, is likely to correlate with decreased bacterial selection pressure, especially important within the GI tract microbiome. Does narrowing the antibiotic spectrum among TCNs used in dermatology have clinical relevance? In answering this question, it is difficult to definitively quantify the overall clinical magnitude based on data available to date, but it is certainly relevant to consider, especially from both clinical and ecologic perspectives, as antibiotic resistance continues to be a major concern globally.
References
- Snodgrass A, Motaparthi K. Systemic antibacterial agents. In: Wolverton SE, Wu J, Eds. Comprehensive Dermatologic Drug Therapy. Fourth Edition, Elsevier, Philadelphia, USA, 2021:82–89.
- Leyden JJ, Del Rosso JQ, Webster GF. Clinical considerations in the treatment of acne vulgaris and other inflammatory skin disorders: a status report. Dermatol Clin. 2009;27:1–15.
- Webster G, Del Rosso JQ. Anti-inflammatory activity of tetracyclines. Dermatol Clin. 2007; 25:133–135.
- Sapadin AN, Fleischmajer R. Tetracyclines: nonantibiotic properties and their clinical implications. J Am Acad Dermatol. 2006;54:258–265.
- Del Rosso JQ, Kim G. Optimizing use of oral antibiotics in acne vulgaris. Dermatol Clin. 2009;27:33–42.
- Levy RM, Huang EY, Roling D, et al. Effect of antibiotics on oropharyngeal flora in patients with acne. Arch Dermatol. 2003;139:467–471.
- Del Rosso JQ, Leyden JJ. Status report on antibiotic resistance: implications for the dermatologist. Dermatol Clin. 2007;25:127–132.
- Del Rosso JQ, Webster GF, Rosen T, et al. Status report from the Scientific Panel on Antibiotic Use in Dermatology of the American Acne and Rosacea Society: part 1: antibiotic prescribing patterns, sources of antibiotic exposure, antibiotic consumption and emergence of antibiotic resistance, impact of alterations in antibiotic prescribing, and clinical sequelae of antibiotic use. J Clin Aesthet Dermatol. 2016;9(4):18–24.
- Kim S, Michaels BD, Kim GK, et al. Systemic antibacterial agents. In: Wolverton SE, Ed. Comprehensive Dermatologic Drug Therapy. Third Edition, Elsevier-Saunders, Philadelphia, USA, 2013:77–87
- Doryx (doxycycline hyclate) tablets delayed release, Mayne Pharma Inc, Greenville, North Carolina, 2020.
- Minocycline hydrochloride capsules USP prescribing information, Teva Canada Limited, Toronto, Ontario, Canada, 2019.
- Simonart T, Dramaix M, De Maertelaer V. Efficacy of tetracyclines in the treatment of acne vulgaris: a review. Br J Dermatol. 2008;158(2):208–216.
- Solodyn (minocycline HCl) extended release tablets, Valeant Pharmaceuticals North America LLC, Bridgewater, New Jersey, 2017.
- Minolira (minocycline hydrochloride) extended release tablets, EPI Health LLC, Charleston, South Carolina, 2018.
- Oracea (doxycycline USP) capsules 40 mg prescribing information, Galderma Laboratories, Fort Worth, Texas, 2014.
- Skidmore R, Kovach R, Walker C, et al. Effects of subantimicrobial-dose doxycycline in the treatment of moderate acne. Arch Dermatol. 2003;139(4):459–464.
- Perret LJ, Tait CP. Non-antibiotic properties of tetracyclines and their clinical application in dermatology. Austral J Dermatol. 2014;55: 111–118.
- Cunha BA, Baron J, Cunha CB. Similarities and differences between doxycycline and minocycline: clinical and antimicrobial stewardship considerations. Eur J Clin Microbiol Infect Dis. 2018;37:15–20.
- Smith K, Leyden JJ. Safety of doxycycline and minocycline: a systematic review. Clin Therapeutics. 2005;27(9):1329–1342.
- Seysara (sarecycline) tablets prescribing information, Almirall LLC, Exton, Pennsylvania, 2019.
- Moore AY, Elizze, Charles M, et al. Sarecycline: a narrow spectrum tetracycline for the treatment of moderate-to-severe acne vulgaris. Future Microbiol. 2019;14(14):1235–1242.
- Zhanel G, Critchley I, Lin LY, et al. Microbiological pro?le of sarecycline, a novel targeted spectrum tetracycline for the treatment of acne vulgaris. Antimicrob Agents Chemother. 2019;63(1): e01297–18.
- Leyden JJ, Sniukiene V, Berk D, et al. Efficacy and safety of sarecycline, a novel, once-daily, narrow spectrum antibiotic for treatment of moderate to severe facial acne vulgaris: results of a phase 2, dose-ranging study. J Drugs Dermatol. 2018;17(3):333–338.
- Batool Z, Lomakin IB, Polikanov Y, Bunick CG. 576 Crystal structure of sarecycline bound to the 70S bacterial ribosome reveals structural differences from other tetracyclines at atomic resolution. J Investig Dermatol. 2020;140(7):S79.
- Chopra I, Roberts M. Tetracycline antibiotics: mode of action, applications, molecular biology, and epidemiology of bacterial resistance. Microbiol Molec Biol Rev. 2001;65(2):232–260.
- Haidari W, Raquel Bruinsma R, Cardenas-de la Garza JA, et al. Sarecycline review. Ann Pharmacother. 2020;54(2):164–170.
- Moore A, Green LJ, Bruce S, et al. Once-daily sarecycline 1.5 mg/kg/day is effective for moderate to severe acne vulgaris: results from two identically designed, phase 3, randomized, double-blind, clinical trials. J Drugs Dermatol. 2018;17(9): 987–996.
- Pariser DM, Green LJ, Lain EL, et al. Safety and tolerability of sarecycline for the treatment of acne vulgaris: results from a Phase III, multicenter, open label study and a phase I phototoxicity study. J Clin Aesthet Dermatol. 2019;12(11):E53–E62.
- Zimmermann P, Curtis N. The effect of antibiotics on the composition of the intestinal microbiota: a systematic review. J Infection. 2019;79:471–489.
- Zaenglein AL, Pathy AL, Schlosser BJ, et al. Guidelines of care for management of acne vulgaris. J Am Acad Dermatol. 2016;74:945–973.

