 J Clin Aesthet Dermatol. 2020;13(10):42–44
J Clin Aesthet Dermatol. 2020;13(10):42–44
by Ritu Swali, MD; Allison Limmer, BS, BA; and Stephen K. Tyring, MD, PhD, MBA
Dr. Swali is a Resident Physician, PGY-2, with the Department of Dermatology at the University of Nebraska Medical Center in Omaha, Nebraska. Dr. Limmer is a Resident Physician, PGY-1,with the Department of Medicine at Memorial Sloan Kettering Cancer Center in New York, New York. Dr. Tyring is with the Department of Dermatology at the University of Texas-Houston Health Science Center, Center for Clinical Studies, and Houston Skin Associates in Houston, Texas.
FUNDING: No funding was provided for this study.
DISCLOSURES: The authors have no conflicts of interest relevant to the content of this article.
ABSTRACT: Kaposi sarcoma (KS) is a low-grade vascular neoplasm with four well-documented clinical types: classic, African (endemic), acquired immunodeficiency syndrome (AIDS)-associated (epidemic), and iatrogenic, as well as a fifth recently described variant, men having sex with men (MSM) without human immunodeficiency virus (HIV) infection. Often distinguishable on clinical exam, KS lesions are typically found on the skin and mucosa of immunocompromised individuals, though numerous published reports have demonstrated the ability of KS to present in immunocompetent individuals. Here, we present the case of a 66-year-old, HIV-negative MSM with violaceous, non-blanching macules and patches of the medial foot referred to dermatology by his primary care physician. Histopathologic analysis revealed Kaposi sarcoma. Although this patient engaged in same-sex sexual behaviors, his HIV-negative status and otherwise lack of immunocompromise would deter many clinicians from suspecting a diagnosis of KS. Despite therapy, disease prognosis is often dependent upon stage at diagnosis. Therefore, it is important that every clinician understand the cutaneous findings associated with KS and be aware of the higher rates of KS even in HIV-seronegative MSM to facilitate prompt diagnosis and immediate treatment of this high-risk population.
Keywords: Kaposi sarcoma, human immunodeficiency virus, HIV, acquired immunodeficiency syndrome, AIDS
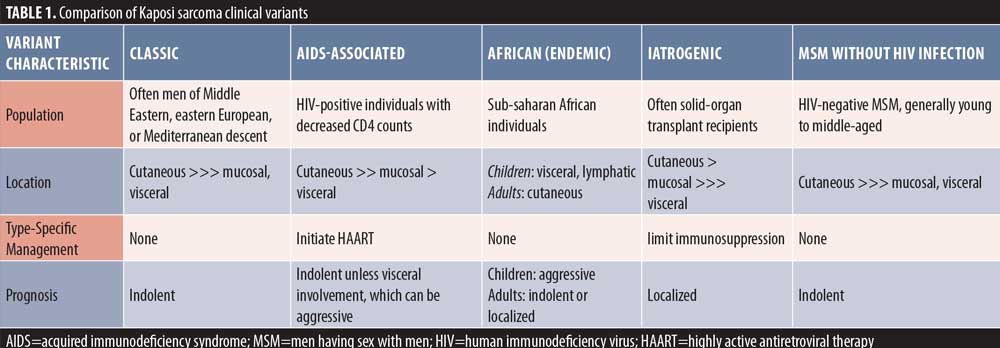
Kaposi sarcoma (KS) is a low-grade vascular neoplasm traditionally categorized into four clinical types: classic, African (endemic), acquired immunodeficiency syndrome (AIDS)-associated (epidemic), and iatrogenic, with a fifth variant, human immunodeficiency virus (HIV)-negative men having sex with men (MSM), being more recently described (Table 1).1–3 Distinguished by their violaceous hue, KS lesions are typically found on the skin, lips, and mucosa of affected individuals.1,2 KS was found in one in three HIV-positive men having sex with men, regardless of age or race, before the highly active antiretroviral therapy (HAART)-era limited the immunosuppresive effects of HIV, whereas a rate of one in 100,000 was seen in the population at large.4 Its reputation in the HIV-positive community has deterred clinicians from suspecting KS in immunocompetent individuals, though numerous published reports have demonstrated the viability of such a diagnosis.3,5–8 Here, we present the case of an HIV-negative MSM with concerning purpuric patches that reinforces the importance of biopsying suspicious, non-healing lesions and recognizing the propensity for KS to present in MSM regardless of HIV serostatus.
Case Report
A 66-year-old Hispanic man with a past medical history of gastroesophageal reflux disease and obstructive sleep apnea presented to the dermatology clinic upon referral from his primary care physician for evaluation of persistent red-purple lesions on the right foot. The patient stated the bruise-like spots had been present for three months and denied associated symptoms, including pruritus, bleeding, and pain. He had not attempted treatment but did note an increase in physical activity that seemed to precipitate lesion appearance. Upon further discussion, it was revealed that the patient was previously exposed to hepatitis (unknown type) and engaged in sexual activity with male partners. The patient reported bi-annual HIV testing, which had repeatedly been negative.

On clinical examination, multiple violaceous, non-blanching macules and patches were noted on the right medial foot (Figure 1). The lesions were not tender to palpation. A shave biopsy was performed. Histopathologic analysis revealed numerous extravasated erythrocytes dispersed among fascicles of spindled cells. Immunostaining for HHV-8 returned positive while MART-1 was negative, consistent with a diagnosis of Kaposi sarcoma. Repeat HIV testing confirmed the patient’s HIV-negative status. The patient was prescribed imiquimod 5% and tretinoin 0.05% cream to be applied twice daily to the affected areas.
Discussion
The patient described here is a member of a high-risk population (MSM), and though his HIV-negative status and otherwise lack of immunocompromise would discourage many clinicians from considering KS, his biopsy is consistent with the clinical diagnosis of KS in MSM without HIV infection, an underrecognized KS variant.3,5–8 Often readily distinguishable on physical exam, biopsy is the diagnostic gold standard for KS, and screening, other than regular oral exams, is not recommended.2 However, the clinical findings in this and many other cases can be subtle, resembling bacillary angiomatosis, spindle cell neoplasms, minor trauma, or other vascular tumors.1,2 In this way, histopathologic analysis and immunostaining in combination with a thorough history and physical exam can be especially helpful in arriving at the diagnosis of KS.
Regardless of clinical type, KS pathology classically demonstrates vascular and spindle cell proliferation in the dermis, inflammatory cells, hyaline globules formed by extravasated red blood cells, and hemosiderin deposition.1,2 Lesional cells also stain positive for human herpesvirus-8 (HHV-8). Transmitted by sexual contact and blood, this virus’s modes of transmission directly reflect the disease’s prevalence.9 Consistent with the observed propensity for KS to present in MSM, HHV-8 has long been detected in prostate tissue and semen.10 Interestingly, recent studies of endemic KS suggest that HHV-8 may also be transmitted via secretions such as saliva and breast milk.9
The majority of the available treatment and prognostic data are from the AIDS-associated KS population, with few studies specifically examining treatment efficacy in the other KS variants. As KS in MSM without HIV infection both appears and behaves as if it were classic KS, it has been suggested that this fifth clinical variant be treated similarly to the classic form.5 Observation is considered appropriate for uncomplicated KS cases, as both treated and untreated KS often follows an indolent course, with signs of progression including edema and visceral sequelae.11 Thus, treatment is often aimed at symptom relief and cosmetic concerns.1 Surgery and radiation are viable options, especially for localized disease. Systemic therapies with varied efficacy include pegylated liposomal doxorubicin, vinca-alkaloids, etoposide, taxanes, gemcitabine, vinblastine with bleomycin, interferon alfa-2, thalidomide, and indinavir. Intralesional vincristine and interferon alfa-2 as well as topical imiquimod and nicotine patches are also frequently employed for cutaneous KS lesions.11
Despite therapy, prognosis often correlates to stage at diagnosis: the higher the stage, the worse the prognosis.2 Thus, it is important that clinicians refer patients with suspicious lesions to a dermatologist urgently to facilitate prompt diagnosis and immediate treatment. Such lesions may be non-healing, non-blanching, red-to-purple flat or raised spots, often resembling bruises or cutaneous vasculitides. Therefore, we suggest that recognizing the cutaneous findings associated with KS and understanding its predilection for the MSM community regardless of HIV infection is valuable for all clinicians.
References
- Radu O, Pantanowitz L. Kaposi sarcoma. Arch Pathol Lab Med. 2013;137(2):289–94.
- Cesarman E, Damania B, Krown SE, et al. Kaposi sarcoma. Nat Rev Dis Primers. 2019;5(1):9.
- Lanternier F, Lebbé C, Schartz N, et al. Kaposi’s sarcoma in HIV-negative men having sex with men. AIDS. 2008;22(10):1163–1168.
- La Ferla L, Pinzone MR, Nunnari G, et al. Kaposi’s sarcoma in HIV-positive patients: the state of art in the HAART-era. Eur Rev Med Pharmacol Sci. 2013;17(17):2354–2365.
- Hinojosa T, Lewis DJ, Liu M, et al. Nonepidemic Kaposi sarcoma: a recently proposed category. JAAD Case Rep. 2017;3(5):441–443.
- Denis D, Seta V, Regnier-Rosencher E, et al. A fifth subtype of Kaposi’s sarcoma, classic Kaposi’s sarcoma in men who have sex with men: a cohort study in Paris. J Eur Acad Dermatol Venereol. 2018;32(8):1377–1384.
- Vangipuram R, Tyring SK. Epidemiology of Kaposi sarcoma: review and description of the nonepidemic variant. Int J Dermatol. 2019;58(5):538–542.
- Wang J, Reid H, Klimas N, et al. An unusual series of patients with Kaposi sarcoma. JAAD Case Rep. 2019;5(8):646–649.
- Li S, Bai L, Dong J, et al K. Kaposi’s sarcoma-associated herpesvirus: epidemiology and molecular biology. Adv Exp Med Biol. 2017;1018:91–127.
- Monini P, de Lellis L, Fabris M, et al. Kaposi’s sarcoma-associated herpesvirus DNA sequences in prostate tissue and human semen. N Engl J Med. 1996;334(18):1168–1172.
- Régnier-Rosencher E, Guillot B, Dupin N. Treatments for classic Kaposi sarcoma: a systematic review of the literature. J Am Acad Dermatol. 2013;68(2):313–331.

