 J Clin Aesthet Dermatol. 2021;14(5):50–55.
J Clin Aesthet Dermatol. 2021;14(5):50–55.
by Jana Pravangsuk, MD; Montree Udompataikul, MD; Nutjira Cheyasak, MD; and Nanticha Kamanamool, MD, PhD
Drs. Pravangsuk and Udompataikul are with the Skin Center, Srinakharinwirot University in Bangkok, Thailand. Dr. Cheyasak is with Panyanunthaphikkhu Chonprathan Medical Center, Srinakharinwirot University in Nonthaburi, Thailand. Dr. Kamanamool is with the Department of Preventive and Social Medicine, Srinakharinwirot University in Bangkok, Thailand.
FUNDING: No funding was provided for this article.
DISCLOSURES: The authors report no conflicts of interest relevant to the content of this article.
ABSTRACT: Background: Acne scarring is a concerning consequence of acne with a prevalence of 11 to 14 percent after acne resolution. Needle subcision is usually used by clinicians to treat acne scars due to its safety and simplicity. Recently, normal saline injection with a pneumatic injector has shown compatible outcomes in treating acne scars.
Objective: This study compared the effectiveness of acne scar treatment with a pneumatic injector and that of hypodermic needle subcision.
Methods: Twenty patients with moderate to severe atrophic acne scars were voluntarily enrolled. All consecutive patients were randomly selected and treated with normal saline injection by using a pneumatic injector on one side of the face during three sessions, separated by a four-week interval. The other side of the face was treated with needle subcision at the end of the first week of the protocol. Subjective assessments were performed by self-evaluation and two blinded dermatologists. For objective assessment, the depth and volume of acne scars were estimated by an ultraviolet A light video camera and Vernier calipers at baseline and four, eight, and 12 weeks. Pain score and adverse reactions were also noted at each visit.
Results: Eighteen patients with Fitzpatrick Skin Type III or IV completed the study. Differences in the resolution in diameter and the volume of boxcar and rolling acne scars over 12 weeks of follow-up between the pneumatic injection and needle subcision groups were statistically significantly improved relative to at baseline; however, there was no statistically significant difference in the efficacy between the two modalities. Satisfaction with each modality was not statistically different. No serious adverse effects occurred. Minor reactions such as minor hematoma and subcutaneous emphysema resolved within two weeks.
Conclusions: The efficacy of normal saline injection with a pneumatic injector is not statistically different from that of needle subcision in treating boxcar and rolling acne scars; however, less side effects were recorded. Given this advantage, the use of pneumatic injectors should be considered for treating acne scars.
Keywords: Acne scar, atrophic acne scar, subcision, pneumatic injection, jet injection
Acne scarring is considered a worrisome issue for acne patients.1 There are three types of acne scars: icepick, boxcar, and rolling. With advanced innovation, therapeutic modalities include chemical peeling, microdermabrasion, laser abrasion, radiofrequency abrasion, skin augmentation, punch technique, and needling; however, none has demonstrated a significantly greater benefit so as to be considered the gold standard. Thus, the severity and type of scar, the patient’s skin type, and financial aspects should be taken into account when choosing the treatment modality.1–4
Pneumatic injection, or jet injection, was first introduced in 1866 by Dr. Jean Sales-Girons;5–7 with this technique, a pneumatic jet stream of compressed gases is used to penetrate the skin and deliver drugs or fluids into the dermal or subdermal layer. This microtrauma also stimulates fibroblasts to produce collagen and elastin. Unlike needle incision, pneumatic needle-free injection can reach deeper into the subdermal layer to promote complete scar resolution with less skin injury.
In this study, we aimed to compare the effectiveness of normal saline injection with a pneumatic injector to that of needle subcision in the context of atrophic acne scar treatment.
Methods
Patient characteristics. This study was conducted involving adult patients aged 18 to 40 years with moderate to severe atrophic acne scars on both cheeks, which were graded according to their level of severity using Goodman’s qualitative grading system, and with Fitzpatrick Skin Type III or IV at the dermatology center of Srinakharinwirot University in Bangkok, Thailand from May 2018 to August 2018. This prospective, assessor-blinded, randomized controlled trial was conducted with consent approval in accordance with the code of ethics of the World Medical Association (Declaration of Helsinki) and was approved by the university ethics committee.
Each patient’s face was divided into two areas to be treated with one therapeutic protocol on each side (i.e., normal saline injection with a pneumatic injector and needle subcision, respectively). The decision of treatment side was determined by computerized block randomization.
Treatment procedure. The treatment area was cleaned with a mild cleanser and treated with local anesthetic cream containing 2.5% lidocaine and 2.5% prilocaine cream for 45 minutes. Then, patients’ faces were cleaned with alcohol solution. All patients underwent normal saline injection with a pneumatic injector (Innojector™; AmorePacific, Seoul, South Korea) on one side of the face for three sessions at four-week intervals. This device injected normal saline into the skin at a speed of 180 m/s. During the first and second treatment sessions, the shot pressure power was set at level 2, shooting 150uL of liquid into boxcar and rolling acne scars. During the third session, the pressure power was set at level 3, shooting 100uL into the scars. Meanwhile, the other side was treated with needling at the end of the first week of the study protocol period. We thrust a Nokor needle no. 18 (Becton, Dickinson and Company, Franklin Lakes, New Jersey) into the edges of each scar in forward and backward directions. After completing each treatment session, patients were treated with a topical antibiotic (Foban® fucidic acid ointment; Medsafe, Wellington, New Zealand) and all wounds were closed with sterile strips.
Subjective evaluation of treatment outcome. Serial high-resolution photography (Fuji X-A2; Fujifilm, Tokyo, Japan) was obtained at baseline and four, eight, and 12 weeks of follow-up. Two independent, treatment-blinded dermatologists assessed images from each follow-up visit for overall improvement from baseline in percentages. Average improvement results were then arranged using a quartile grading scale. Pain associated with treatment was assessed immediately after the first session of both treatments and was rated on a 10-point scale (0=no pain at all; 10=the most severe pain). The overall satisfaction with scar resolution was determined at each follow-up visit and graded using five categories: very dissatisfied, not very satisfied, slightly satisfied, satisfied, and very satisfied. At each visit, we also recorded any adverse events, such as infection, hyperpigmentation, and scarring.
Objective evaluation of treatment outcome. Three boxcar and rolling scars on each cheek were chosen for evaluation at the beginning of the study protocol period; these scars were marked and mapped with a translucent sheet to ensure consistency of their locations. The volume of these acne scars was measured using an ultraviolet A light video camera (Visioscan® VC 98; Courage-Khazaka, Köln, Germany) with analysis software (Surface Evaluation of the Living Skin; Courage-Khazaka). The diameters of these three scars were measured by using Vernier calipers. Each scar was measured three times per site to discern the mean volume value and diameter at each visit at Weeks 4, 8 and 12. Changes with the two treatments were contrasted with baseline observations.
Statistical analysis. Linear mixed model analysis was used to compare the average mean volume and diameter values of acne scars at Weeks 4, 8, and 12 with the baseline data. The paired Student’s t-test was used to compare average pain level and patient satisfaction and duration with the overall improvement after treatment. The chi-squared test was used to compare the percentage of side effects from treatment. Statistical analysis was conducted using the Statistical Package for the Social Sciences (SPSS) version 19 for Windows (IBM Corporation, Armonk, New York) and STATA version 13 for Windows (StataCorp LLC, College Station, Texas).
Results
Among a total number of 20 patients included, 18 (90%) were able to complete all treatment sessions. Two subjects were withdrawn from the study due to being lost to follow-up. Among the 18 participants who completed the study, nine (50%) were men and nine (50%) were women, with an average age of 26 years (range: 20–32 years). The average scar age was seven years (range: 2–15 years) and half of the study participants had never undergone acne scar treatment before. The average volumes of boxcar and rolling scars measured by Visioscan® VC 98 were 49.15 and 49.99mm3, respectively, while the mean diameters of boxcar and rolling scars as measured using Vernier calipers were 1.86 and 4.25mm (Table 1). The volume and diameter values of boxcar and rolling scars in both groups were similar.
Following the subjective evaluation performed at four weeks after treatment, the two blinded dermatologists reported that most patients in both groups (55.56%) showed 25- to 50-percent resolution in acne scars in both treatments. Regarding patients’ satisfaction at four weeks after treatment, most were very satisfied following normal saline injection with a pneumatic injector (66.67%) and needle subcision (72.22%), with no statistically significant difference (p=0.542).
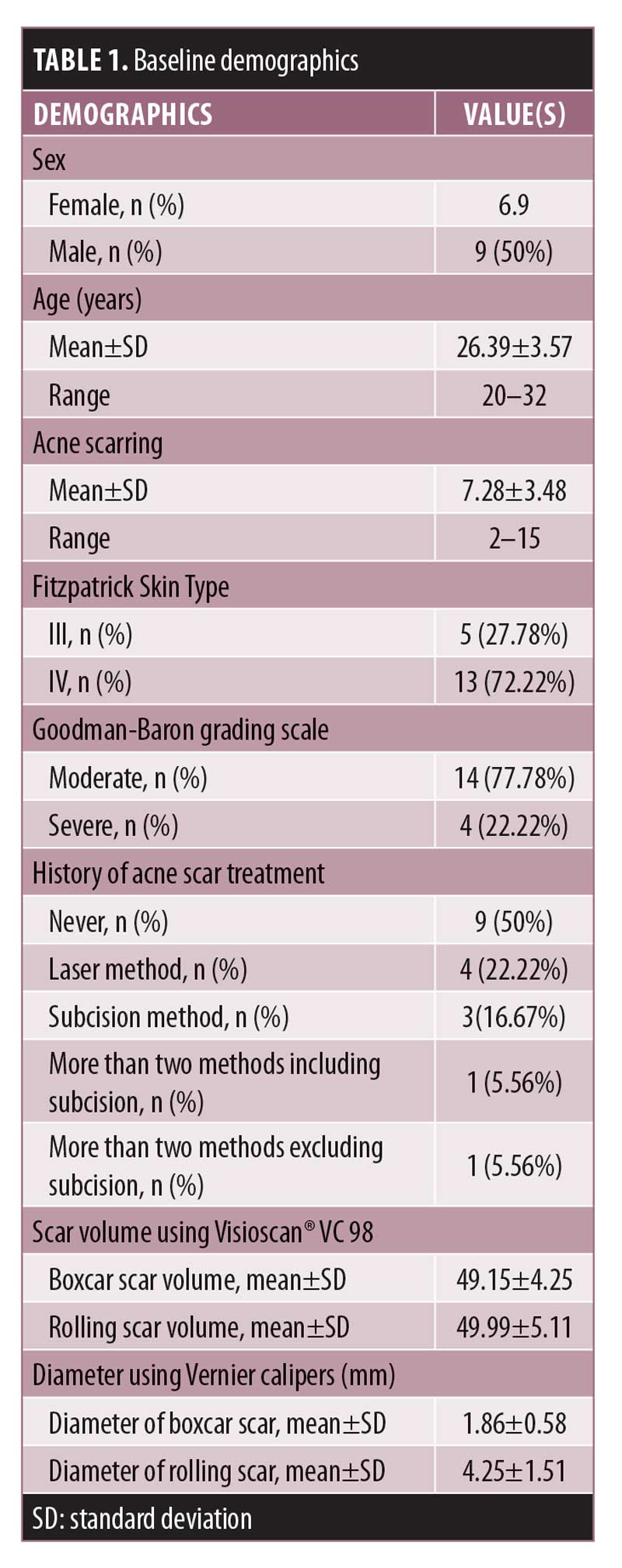
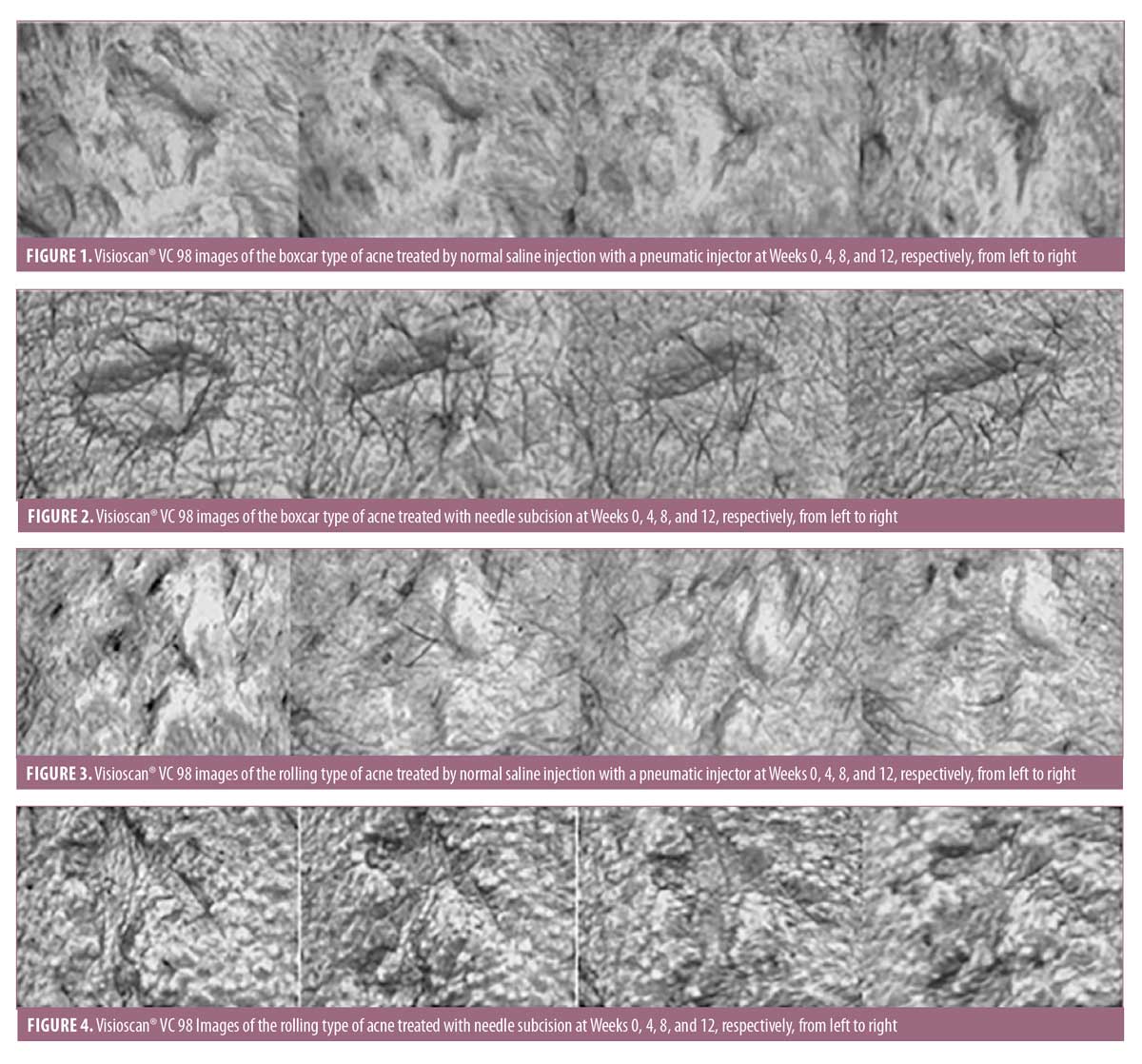
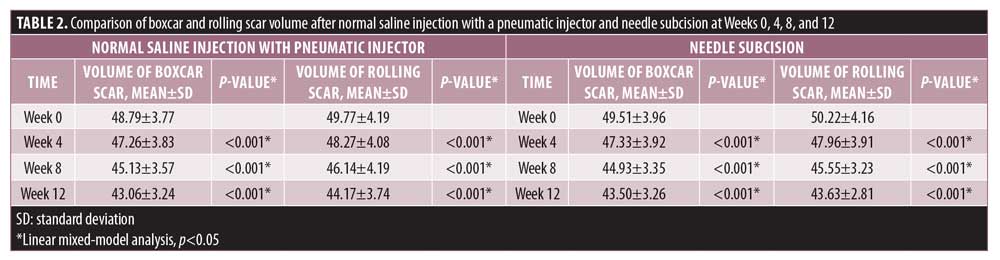
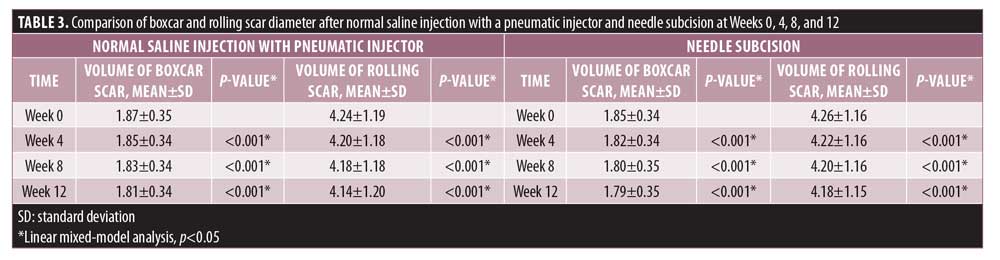
An objective evaluation using the Visioscan® VC 98 system revealed a statistically significant improvement in boxcar scar volume at four, eight, and 12 weeks of treatment in both sites that underwent normal saline injection with a pneumatic injector (p<0.001) and those that received subcision treatment (p<0.001) relative to baseline as shown in Table 2. The results of boxcar scar volume resolution following pneumatic injection treatment were similar to those in the needle subcision group (p=0.339), with example images after treatment presented in Figures 1 and 2. In patients with rolling scars, significant resolution in volume occurred at four, eight, and 12 weeks of treatment in both groups treated with pneumatic injection (p<0.001) and subcision treatment (p<0.001), respectively, as compared with at baseline as shown in Table 2. However, there was no significant difference between these two treatment protocols (p=0.360) as can be seen in images taken after treatment presented in Figures 3 and 4. Similarly, significant resolution of boxcar scar diameter as measured by Vernier calipers at four, eight, and 12 weeks of treatment with both modalities occurred as shown in Table 3 (p<0.001 both); in particular, there were similar resolutions in boxcar scar diameter when comparing the normal saline injection with a pneumatic injector group with the needle subcision group (p=0.497). The diameter of rolling scars improved following both treatments relative to at baseline as shown in Table 3 (p<0.001 both) and there was no difference between pneumatic injector and subcision treatment (p=0.815).
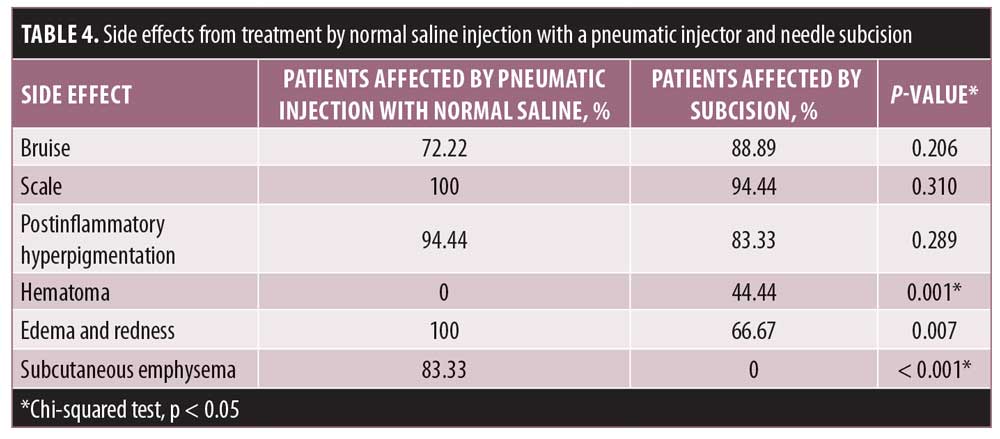
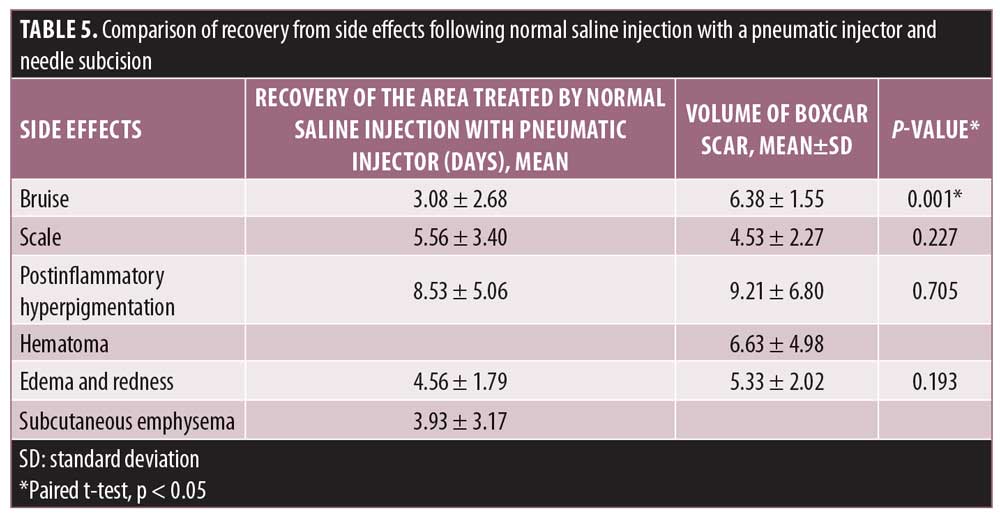
Adverse reactions. The average pain level of participants on the side treated by normal saline injection with a pneumatic injector was scored as 3.61 out of 10, while that for the subcision side was scored as 6.56 out of 10. Thus, the subcision modality triggered a significantly higher level of pain as compared with pneumatic injection (p<0.001). Also, bruising after treatment took a longer time to resolve in those treated with needle subcision as compared with pneumatic injection (p=0.001). Other adverse reactions were similar in terms of the affected patients and the durations of events between the two groups as shown in Tables 4 and 5.
Discussion
According to our results, treating boxcar and rolling scars by one-time needle subcision yields similar scar resolution compared to three sessions of pneumatic injection with normal saline. In terms of patients’ satisfaction, there were no differences between needle subcision and pneumatic injection with normal saline. By the end of the 12 week after pneumatic injection, boxcar scars were decreased both in terms of volume (11.69%±2.35%) and diameter (3.42%±1.07%). Similarly, rolling scars were decreased both in terms of volume (11.12%±3.01%) and diameter (2.47%±2.19%). At 12 week after needle subcision, boxcar scars were also decreased both in terms of volume (12.03%±3.56) and diameter (1.87%±0.72%). There was no statistically difference in scar size improvement between these two methods. Using serial high-resolution photography, it was revealed that both scar types improved by 25 to 50 percent. According to Lee et al,5 using hyaluronic acid for pneumatic injection instead of normal saline was reported to achieve an improvement of up to 50 to 75 percent. One possible explanation for this is that the normal saline used in this study had no filling effect, unlike hyaluronic acid from the other study. However, it causes more tissue injury.
Noninvasive treatments such as chemical peels and dermabrasion are usually considered in combination with modalities as their outcome alone as monotherapy was not especially great when treating deep scars. According to Ramadan et al,8 needle subcision clearly outperformed chemical reconstruction of skin scars using 100% trichloroacetic acid in decreasing scar size, with a diameter change of 0.3867±0.090 cm2 and 0.08657±0.090 cm2 (p<0.01), respectively.8 Despites the benefits in terms of cost-effectiveness, the adverse events that might occur after using peeling agents for medium-depth scars include stinging, burning sensation, and skin hypo-/hyperpigmentation. Furthermore, cardiotoxicity was noted in deep-peeling using a phenol solution.2 Likewise, following dermabrasion, the study by El-Domyati et al9 reported mild improvement in 45.4 percent and no improvement in 27.3 percent of patients.
Following microneedling and radiofrequency microneedling treatments, acne scars responded poorly as compared with after pneumatic injection, with 15 to 20 percent scar healing associated with microneedling and less than 25 percent scar healing associated with radiofrequency microneedling.10 Although treatment with microneedling has some side effects, such as temporary erythema and edema, the complete treatment requires a significant amount of medical visits.11 Postinflammatory hyperpigmentation was also noted to last up to 30 days following radiofrequency microneedling treatment, while hyperpigmentation from pneumatic injection usually resolves within 14 days.10
Laser treatment or resurfacing is considered to be effective modality for both boxcar and rolling atrophic scars. Fractional CO2 laser (Fraxel)12 and fractional 1,550-nm erbium fiber laser13 achieved scar resolution levels of 43 percent and 26 to 50 percent, respectively. The efficacy is considered similar to pneumatic injection of normal saline with scar resolution of 25 to 50 percent. However, postinflammatory hyperpigmentation could last much longer in laser treatment with a duration of up to 2 to 3 months in contrast with pneumatic injection with a duration of less than two weeks.14,15
Interestingly, the results in those treated with pneumatic injectors include reduced event rates of hematoma and edema as compare with following needle subcision. Also, bruises after subcision take a significantly significant longer time to heal relative to those after pneumatic injection. Pneumatic injection with normal saline causes only half the pain that needle subcision provokes, with scores of 3.61 and 6.56 out of 10, respectively. These findings could possibly be explained by the fact that pneumatic injection requires only a minute entry point in the epidermis and causes limited injury to the dermal layer. All side effects reported in this study were minor and spontaneously resolved within two weeks.
This study has several strengths. First, our results emphasize the validity of performing pneumatic injection of normal saline for atrophic scar treatment. We have devised a methodology to measure the resolution both objectively and subjectively. Second, we choose to perform a split-face comparative study to avoid confounding bias. Third, adverse reactions from both modalities were investigated in detail and demonstrated in comparison.
Limitations. We are aware that our research has several limitations. First, the studied population was relatively small in size. Due to the fact that this is a novel solution for treating atrophic scars, available patients were limited due to costs. Indeed, the previous study considering pneumatic injection of hyaluronic acid included only two patients.16 Still, although our investigations so far have only been on a small scale, we believe it was enough to demonstrate statistically significant outcomes. Second, due to the limited follow-up time, we were unable to identify long-term effects. We suggest that further research with long-term side effects monitoring and the injection of other substances with pneumatic injectors should be conducted.
Conclusion
This study showed that normal saline injection using a pneumatic injector and needle subcision improved scar volume and scar diameter as measured by Visioscan® VC98 and Vernier calipers, respectively, with statistically significant differences from baseline observed. However, there was no statistically significant difference in efficacy between these two modalities. Overall, with good efficacy, minimal adverse effects, and minimal pain, pneumatic injection with normal saline can be considered a promising treatment modality for moderate to severe boxcar and rolling acne scars.
References
- Pavlidis AI, Katsambas AD. Therapeutic approaches to reducing atrophic acne scarring. Clin Dermatol. 2017;35(2):190–194.
- Gozali MV, Zhou B. Effective treatments of atrophic acne scars. J Clin Aesthet Dermatol. 2015;8(5):33–40.
- Cohen BE, Brauer JA, Geronemus RG. Acne scarring: A review of available therapeutic lasers. Lasers Surg Med. 2016;48(2):95–115.
- Fabbrocini G, De Vita V, Pastore F, et al. Combined use of skin needling and platelet-rich plasma in acne scarring treatment. Cosmet Dermatol. 2011;24(4):177–183.
- Lee JW, Kim BJ, Kim MN, Lee CK. Treatment of acne scars using subdermal minimal surgery technology. Dermatol Surg. 2010;36(8): 1281–1287.
- Kwon TR, Seok J, Jang JH, et al. Needle-free jet injection of hyaluronic acid improves skin remodeling in a mouse model. Eur J Pharm Biopharm. 2016;105:69–74.
- Li X, Ruddy B, Taberner A. Characterization of needle-assisted jet injections. J Control Release. 2016;243:195–203.
- El-Rahman Ramadan SA, Medhat El-Komy MH, Bassiouny DA, El-Tobshy SA. Subcision versus 100% trichloroacetic acid in the treatment of rolling acne scars. Dermatol Surg. 2011;37(5):626–633.
- El-Domyati M, Hosam W, Abdel-Azim E, Abdel-Wahab H, Mohamed E. Microdermabrasion: a clinical, histometric, and histopathologic study. J Cosmet Dermatol. 2016;15(4):503–513.
- Vejjabhinanta V, Wanitphakdeedecha R, Limtanyakul P, Manuskiatti W. The efficacy in treatment of facial atrophic acne scars in Asians with a fractional radiofrequency microneedle system. J Eur Acad Dermatol Venereol. 2014;28(9):1219–1225.
- El-Domyati M, Barakat M, Awad S, et al. Microneedling therapy for atrophic acne scars: an objective evaluation. J Clin Aesthet Dermatol. 2015;8(7):36–42.
- Nilforoushzadeh MA, Faghihi G, Jaffary F, et al. Fractional carbon dioxide laser and its combination with subcision in improving atrophic acne scars. Adv Biomed Res. 2017;6:20.
- Thongsai M. The comparison of fractional 1550 nm erbium fiber laser combined with a chemical reonstruction of skin scars (CROSS) method versus fractional 1550 nm erbium fiber laser alone for treatment of moderate to severe atropic acne scar. Srinakharinwirot University; 2015.
- Majid I, Imran S. Fractional CO2 laser resurfacing as monotherapy in the treatment of atrophic facial acne scars. J Cutan Aesthet Surg. 2014;7(2):87–92.
- Chayavichitsilp P, Limtong P, Triyangkulsri K, Pratumchart N. Comparison of fractional neodymium-doped yttrium aluminum garnet (Nd: YAG) 1064-nm picosecond laser and fractional 1550-nm erbium fiber laser in facial acne scar treatment. Lasers Med Sci. 2020;35(3):695–700.
- Patel T, Tevet O. Effective treatment of acne scars using pneumatic injection of hyaluronic acid. J Drugs Dermatol. 2015;14(1):74–76.

