 J Clin Aesthet Dermatol. 2021;14(5):56–58.
J Clin Aesthet Dermatol. 2021;14(5):56–58.
by Ersilia Tolino, MD; Nevena Skroza, MD; Alessandra Mambrin, MD; Ilaria Proietti, MD; Nicoletta Bernardini, MD; Veronica Balduzzi, MD; Anna Marchesiello, MD; Marco Di Fraia, MD; Simone Michelini, MD; and Concetta Potenza, MD
All authors are with the Dermatology Unit “Daniele Innocenzi”, Department of Medical-Surgical Sciences and Biotechnologies, at the Sapienza University of Rome in Polo Pontino, Latina, Italy.
FUNDING: No funding was provided for this article.
DISCLOSURES: The authors report no conflicts of interest relevant to the content of this article.
ABSTRACT: Background: Acne is a chronic multifactorial skin disease with a high prevalence among adolescents. The therapeutic approach for mild to moderate papulopustular acne includes the use of systemic tetracycline. Increased risk of antibiotic resistance necessitates research into alternative therapeutic approaches, such as zinc sulphate. Efficacy of zinc sulphate in acne treatment is widely reported in the literature, but drug comparison studies are lacking.
Objective: We sought to compare the efficacy and safety of zinc sulphate to lymecycline for the treatment of mild to moderate papulopustular acne.
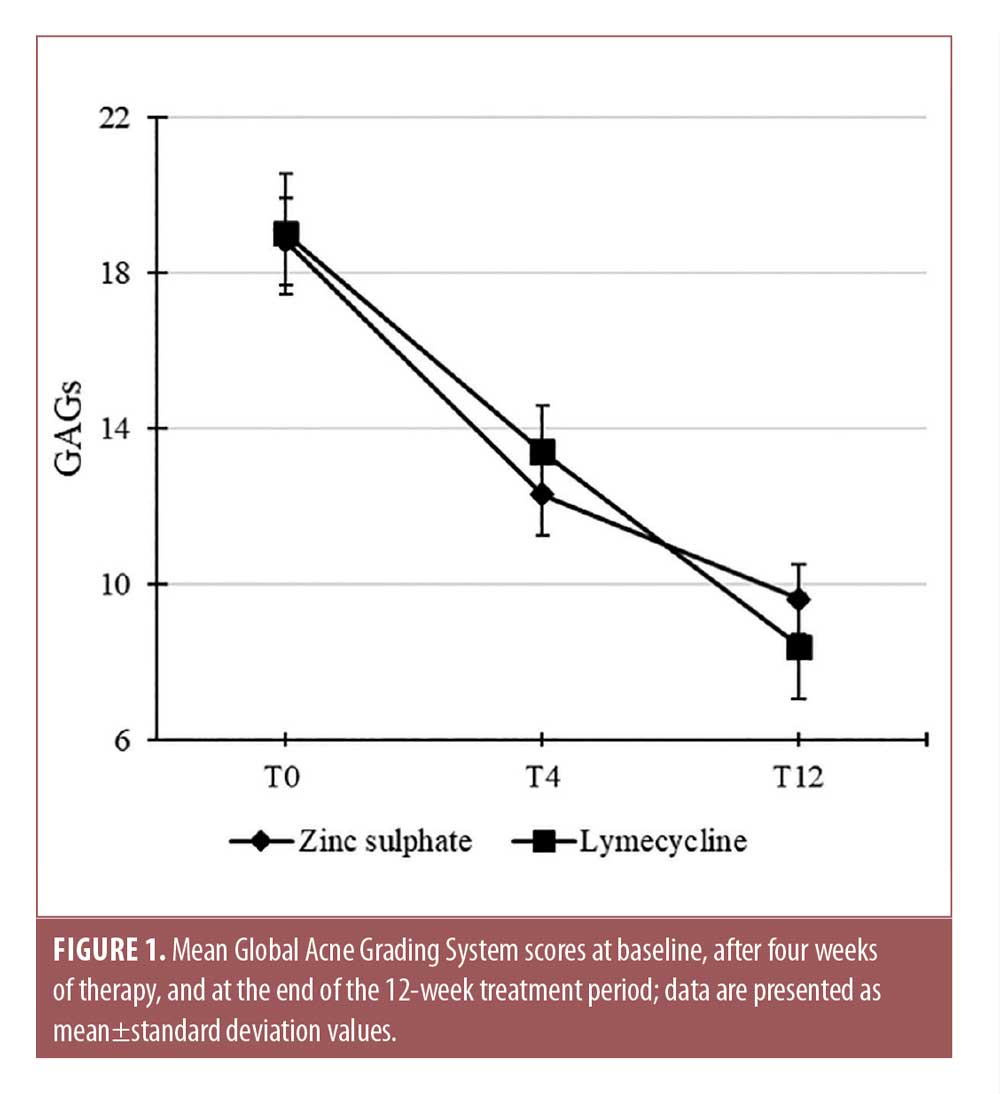
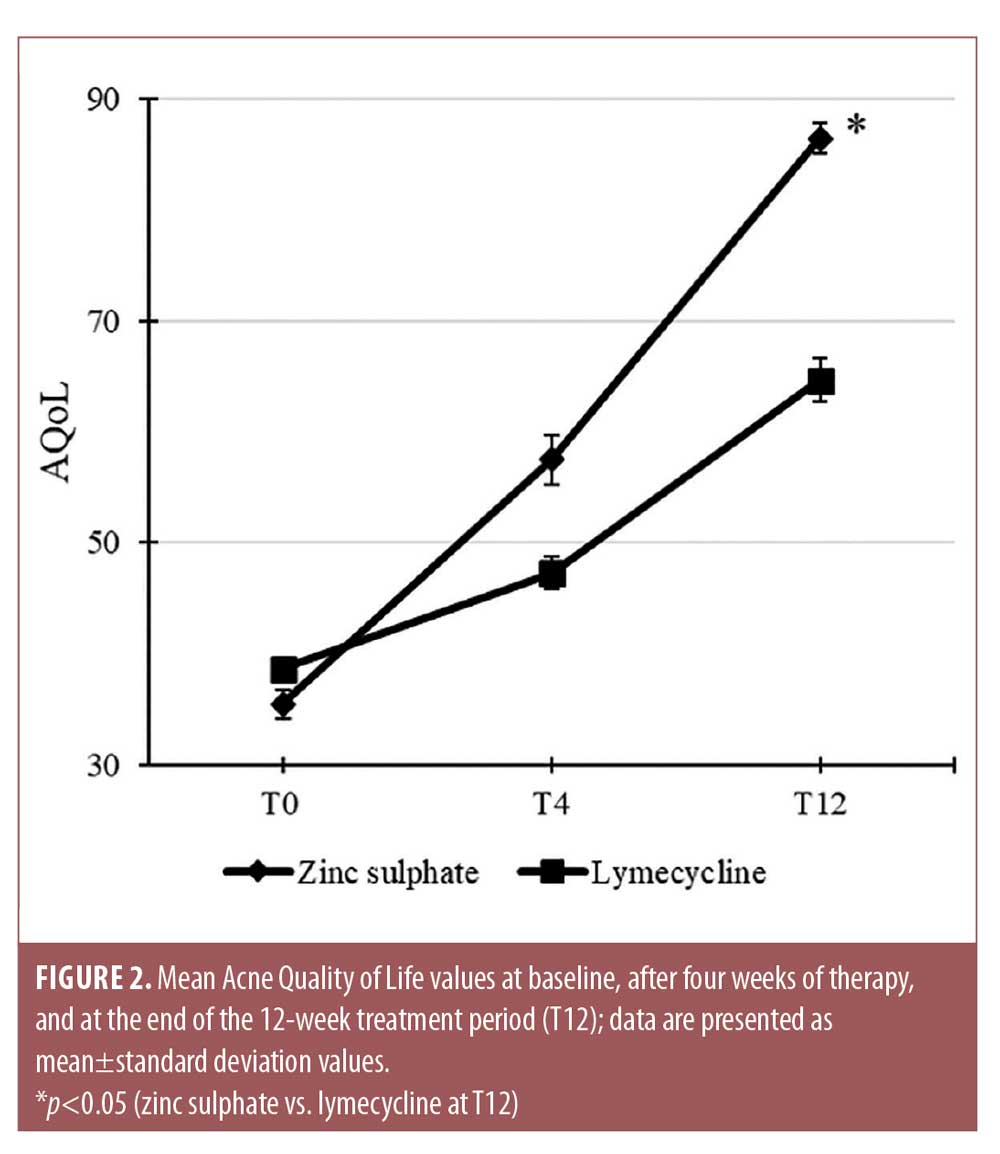
Methods: One hundred patients were equally randomized to receive either zinc sulphate or lymecycline. Acne severity was evaluated using the subjective Global Acne Grading System (GAGS) and the Acne-specific Quality of Life (AQoL) questionnaire at baseline and after four and 12 weeks.
Results: Both zinc sulphate and lymecycline induced a statistically significant reduction in GAGS scores at four and 12 weeks of treatment. The improvements in AQoL scores in patients treated with zinc sulphate were significantly higher than those in the lymecycline group.
Conclusions: Our study suggests that zinc sulphate is a valid alternative therapeutic approach in the treatment of mild to moderate papulopustular acne relative to lymecycline in terms of clinical efficacy, tolerability, and the occurrence of side effects.
Keywords: Acne, lymecycline, zinc
Acne is an inflammatory chronic disease of the pilosebaceous unit. Management of acne requires a therapeutic approach acting on all pathogenetic factors. Combination therapy, including oral antibiotics (i.e., tetracyclines) represents the first-line treatment for moderate acne.1 Antibiotic therapy should be limited to three months due to antibiotic resistance risk and possible reduction of efficacy.1 Moreover, tetracyclines are not recommended during pregnancy and in pediatric patients and are included among the potentially photosensitizing drugs.2
A recent review by Walsh et al3 emphasizes the importance of limiting antibiotic use in the treatment of mild to moderate acne to reduce the risk of antibiotic resistance. Thus, alternative treatments are required. Among these, the European Dermatology Forum guidelines for the treatment of acne suggests oral zinc for the treatment of mild to moderate papulopustular acne.4
Zinc is an essential micronutrient and a cofactor of many metalloenzymes. It is a key modulator of the immune system and could be reduced in inflammatory skin diseases.5 Systemic zinc intake can reduce inflammation through different mechanisms. In patients with acne, zinc is able to inhibit leucocyte chemotaxis and reduce sebum secretion, most likely by inhibiting the activity of androgenetic hormones.6 Furthermore, zinc inhibits Toll-like receptor 2 expression on human keratinocytes, which is stimulated by the presence of Cutibacterium acnes, reducing the synthesis and the release of pro-inflammatory cytokines.7 Finally, it has been observed that zinc has a specific antimicrobial activity against C. acnes as it can interfere with the activity of bacterial lipases.8 Several studies support that zinc sulphate, administered orally in doses ranging from 400 to 600mg per day (corresponding to 90–150mg of Zn2+/day) for up to 12 weeks is effective in reducing inflammatory lesions in patients with moderate inflammatory acne.9–12 The most common side effects are associated with gastrointestinal disorders, such as nausea, vomiting, and diarrhea.13
Lymecycline is a semisynthetic, short-acting tetracycline whose use in acne treatment is well documented in the literature.14,15 Tetracyclines have both antibacterial and anti-inflammatory functions, inhibiting bacterial protein synthesis, neutrophil chemotaxis, cytokine production, and macrophage function.16 They can be administered in the form of a single daily dose and are rapidly absorbed by the gastrointestinal tract. Common side effects include nausea, diarrhea, and headache.17
Methods
We enrolled 100 patients from our outpatient clinic who were affected by mild to moderate papulopustular acne. Included patients were older than 16 years of age, had no local or systemic acne treatment in the previous three weeks, and no history of therapy with isotretinoin. Patients affected by severe acne or other dermatologic conditions that required systemic therapy, those who were pregnant or breastfeeding, and nonadherent subjects were excluded from this study. Age- and sex-stratified randomization into two groups was conducted before baseline assessment. The 50 patients in the zinc sulphate group were given a 200-mg tablet twice daily (400mg/day), while the 50 patients in the lymecycline group were given a 300-mg tablet one daily. The treatment period was 12 weeks, from October 2018 to March 2019. Patients were evaluated at baseline (T0), after four weeks of therapy (T4), and at the end of the treatment period (T12).
All patients gave written informed consent to be enrolled in the present study. The present study was conducted in accordance with the World Medical Association’s Declaration of Helsinki on ethical principles for medical research.
During the entire study period, no other topical or systemic treatments were allowed. Patients underwent a washout period of at least two weeks for topical therapy, four weeks for oral antibiotics, and 24 weeks for oral retinoids. To prevent eventual photosensitivity reactions due to lymecycline administration, patients were counseled to avoid direct sunlight exposure.
Acne was evaluated according to the Global Acne Grading System (GAGS), a subjective method that classifies acne as mild (0–18), moderate (19–32), severe (31–38), and very severe (>39).18 Quality of life was assessed by the Acne Quality of Life (AQoL) questionnaire, which contains 19 questions organized into four domains (self-perception, role-social, role-emotional, and acne symptoms).19 Clinical evaluation, questionnaire administration, and the recording of any side effects were performed at each visit (T0, T4, T12).
Statistics. All data were expressed using mean±standard deviation values. Comparisons between treatments was performed using two-way analysis of variance followed by Bonferroni’s post-hoc test. P-values of less than 0.05 were considered statistically significant. Correlation coefficient was performed using Pearson’s analysis.
Results
Age (mean age 17.7±3.1 years in the zinc sulphate group and 18.5±4.2 years in the lymecycline group) and sex distribution were almost equal in both groups (55.3% female and 44.7% male in the zinc sulphate group and 54.5% female and 45.5% male in the lymecycline group). The mean T0 GAGS score in the zinc sulphate group was 18.8±2.2 points and that in the lymecycline group was 19.0±3.1 points. Both zinc sulphate and lymecycline induced a statistically significant reduction in GAGS scores at T4 (12.3±2.1 vs. 13.4±2.4 points) and at T12 (9.6±1.8 vs. 8.4±2.7 points) (Figure 1). However, no statistical difference was observed between the two treatments. AQoL scores were significantly improved over time in both groups. The average T0 AQoL scores were 35.5±2.7 points in the zinc sulphate group and 38.7±1.4 points in the lymecycline group, respectively; however, AQoL scores in the zinc sulphate group were significantly superior to those in the lymecycline group at both T4 (57.5±4.6 vs. 47.3±2.8 points) and T12 (86.5±2.7 vs. 64.7±3.9 pints) (Figure 2). Side effects were present in both groups, including two cases of headache and two cases of stomach ache in the lymecycline group while, in the zinc group, six patients complained of nausea. No therapy discontinuation was reported due to side effects.
 Discussion
Discussion
Several studies have been conducted to assess the role of zinc in acne treatment. In a review by Cervantes et al20 on the role of zinc in the treatment of acne, the authors found 12 studies that supported its efficacy as a single-agent product and 10 studies that compared zinc with an antibiotic such as clindamycin, oral tetracycline, erythromycin, and minocycline. These 10 studies found that zinc was equally as effective or less effective than oral tetracycline, equally as effective or more effective than erythromycin and clindamycin, and less effective than oral minocycline.20
As far as we know, our study is the first study to compare the efficacy of zinc to lymecycline in the treatment of acne. Our results shows that treatment with zinc sulphate is similar to lymecycline in terms of reducing acne severity assessed by GAGs. Patients included in the two study groups had similar baseline GAGs values, and, at T4 and T12, they decreased similarly. No statistical difference was observed between the two groups. Regarding the impact of acne on quality of life, the mean AQoL scores increased significantly at T4 and T12 in both groups, with significant higher values recorded in the group receiving zinc sulphate therapy.
In our study, a daily dose of 400mg of zinc sulphate, administered for 12 weeks, appeared to be a safe treatment, as reported side effects were in line with those reported in the literature13,20 and did modify adherence to therapy. Compared to lymecycline, advantages of zinc include its safety in pediatric patients and during pregnancy. Most importantly, zinc is not included among the photosensitive agents and has no risk of triggering antibiotic resistance, which represents an increasing public health issue.3
Limitations. Limitations of this study include its open-label study design, which might have biased the interpretation of the observed results, and the use of a subjective scoring system like GAGS instead of an objective one (e.g., lesion count), which weakens the strength of the obtained results.
Conclusion
Our work not only supports the efficacy and safety of oral zinc sulphate for the treatment of mild to moderate papulopustular acne, but also represents the first evidence of treatment equivalence between zinc and lymecycline. Larger, randomized, controlled trials are needed before meaningful
References
- Zaenglein AL, Pathy AL, Schlosser BJ et al. Guidelines of acne for the managment of acne vulgaris. J Am Acad Dermatol. 2016;74(5): 945–973.
- Botros PA, Tsai G, Pujalte GG. Evaluation and management of acne. Prime Care. 2015;42(4):465–471.
- Walsh TR, Efthimiou J, Dréno B. Systematic review of antibiotic resistance in acne: an increasing topical and oral threat. Lancet Infect Dis. 2016;16(3):e23–e33.
- Nast A, Dréno B, Bettoli V. European evidence-based (S3) guideline for the treatment of acne-update 2016. J Eur Acad Dermatol Venerol. 2016;30(8):1261–1268.
- Brocard A, Dréno B. Innate immunity: a crucial target for zinc in the treatment of inflammatory dermatosis. J Eur Acad Dermatol Venerol. 2011;25(10):1146–1152.
- Dréno B, Trossaert M, Boiteau HL, Litoux P. Zinc salts effects on granulocyte zinc concentration and chemotaxis in acne patients. Acta Derm Venereol. 1992;72(4):250–252.
- Jarrousse V, Castex-Rizzi N, Khammari A, et al. Zinc salts inhibit in vitro Toll-like receptor 2 surface expression by keratinocytes. Eur J Dermatol. 2007;17(6):492–496.
- Brocard A, Dréno B. Innate immunity: a crucial target for zinc in the treatment of inflammatory dermatosis. J Eur Acad Dermatol Venereol. 2011;25(10):1146–1152.
- Göransson K, Lidén S, Odsell L. Oral zinc in acne vulgaris: a clinical and methodological study. Acta Derm Venereol. 1978;58(5):443–448.
- Kobayashi H, Aiba S, Tagami H. Successful treatment of dissecting cellulitis and acne conglobata with oral zinc. Br J Dermatol. 1999;141(6):1137–1138.
- Michaëlsson G, Juhlin L, Vahlquist A. Effects of oral zinc and vitamin A in acne. Arch Dermatol. 1977;113(1):31–36.
- Verma KC, Saini AS, Dhamija SK. Oral zinc sulphate therapy in acne vulgaris: a double-blind trial. Acta Derm Venereol. 1980;60(4): 337–340.
- Samman S, Roberts DC. The effect of zinc supplements on plasma zinc and copper levels and the reported symptoms in healthy volunteers. Med J Aust. 1987;146(5):246–249.
- Bossuyt L, Bosschaert J, Richert B, et al. Lymecycline in the treatment of acne: an efficacious, safe and cost-effective alternative to minocycline. Eur J Dermatol. 2003;13(2): 130–135.
- Ocampo-Candiani J, Velazquez-Arenas LL, de la Fuente-Garcia A, Trevino-Gomezharper C, Berber A. Safety and efficacy comparison of minocycline microgranules vs lymecycline in the treatment of mild to moderate acne: randomized, evaluator-blinded, parallel, and prospective clinical trial for 8 weeks. J Drugs Dermatol. 2014;13(6):671–676.
- Bienenfeld A, Nagler AR, Orlow SJ. Oral antibacterial therapy for acne vulgaris: an evidence-based review. Am J Clin Dermatol. 2017;18(4):469–490.
- Agwuh KN, MacGowan A. Pharmacokinetics and pharmacodynamics of the tetracyclines including glycylcyclines. J Antimicrob Chemother. 2006;58(2):256–265.
- Doshi A, Zaheer A, Stiller MJ. A comparison of current acne grading systems and proposal of a novel system. Int J Dermatol. 1997;36(6): 416–418.
- Martin AR, Lookingbill DP, Botek A, et al. Health-related quality of life among patients with facial acne—assessment of a new acne-specific questionnaire. Clin Exp Dermatol. 2001;26(5):380–385.
- Cervantes J, Eber AE, Perper M, et al. The role of zinc in the treatment of acne: a review of the literature. Dermatol Ther. 2018;31(1).

