 J Clin Aesthet Dermatol. 2021;14(8):49–51
J Clin Aesthet Dermatol. 2021;14(8):49–51
by Payal M. Patel, MD and Peter A. Lio, MD
Dr. Patel is with the Department of Dermatology at the University of Illinois at Chicago in Chicago, Illinois. Dr. Lio is with Northwestern University Feinberg School of Medicine, and Medical Dermatology Associates of Chicago in Chicago, Illinois.
FUNDING: No funding was provided for this article.
DISCLOSURES: Dr. Lio reports research grants/funding from the National Eczema Association, Regeneron/Sanofi Genzyme, and AbbVie; is on the speaker’s bureau for Regeneron/Sanofi Genzyme, Pfizer, and L’Oreal; and reports consulting/advisory board work for UCB, Dermavant, Regeneron/Sanofi Genzyme, Dermira, Pfizer, LEO Pharmaceuticals, AbbVie, Kiniksa, Eli Lilly, Micreos (stock options), La Roche Posay/L’Oreal, Pierre-Fabre, Johnson & Johnson, Unilever, Menlo Therapeutics, Theraplex, IntraDerm, Exeltis, AOBiome, Realm Therapeutics, Franklin Bioscience/Altus Labs (stock options), Verrica, TopMD, Arbonne, Amyris, Bodewell, and Burt’s Bees. In addition, Dr. Lio has a patent pending for a Theraplex product, with royalties paid, and is a board member and Scientific Advisory Committee member of the National Eczema Association Dr. Patel reports no conflicts of interest relevant to the content of this article.
ABSTRACT: Background. Topical cannabinoid products are increasingly being recommended and used for a variety of dermatologic conditions. Despite this, safety and efficacy data of topical preparations are lacking, and the differences between topical and oral formulations are not well characterized.
Objective. We reviewed the literature to gather published data on topical cannabinoid products and the differences between topical and oral formulations.
Methods. The PubMed/MEDLINE literature database was searched using the terms “cannabinoids,” “cannabidiol,” “CBD,” “topical cannabidiol,” “transdermal cannabidiol,” “hemp” and “skin.” Results were manually screened to identify published data on topical formulations of cannabinoids or cannabidiol use, adverse effects, sourcing, and solubility.
Results. Topical formulations of cannabinoids might be more nuanced than oral formulations, due not only to dosing differences, but also to potential differences in transcutaneous absorption. Safety and efficacy might need to be evaluated on a product-by-product basis until universal standards for topical preparations are better established.
Conclusion. Topical cannabinoid products might be an important addition to the dermatologic armamentarium, with the potential to dose cannabinoids directly to the skin while minimizing systemic exposure. However, before this can be done reliably, important formulation parameters must be established and verified.
Keywords: Topical cannabidiol, cannabinoids, CBD, medical marijuana, cannabis
In the past several years, there has been a noteworthy surge in the availability and demand of topical cannabidiol (CBD) products for medical uses, including for pain, pruritus, and general skincare.1–4 However, while there is increasing acceptance of cannabinoids in both medical and consumer cultures, many questions have been raised regarding their safety, bioavailability, and sourcing. We sought to examine the literature for what is known regarding topical CBD formulations.
Since orally consumed CBD is subject to first-pass metabolism and transdermal CBD has low aqueous solubility, finding ways to increase the therapeutic efficacy of CBD are imperative.5,6 Transdermal delivery systems are designed to overcome the skin barrier in order to increase the systemic bioavailability of therapeutics, unlike topical formulations that are not meant to enter systemic circulation.7,8 If the drug has poor solubility and diffusivity through the skin, it may accumulate within the layers of the skin, rendering it inefficient systemically.8 Therefore, the efficiency of penetration enhancers in improving the bioavailability of highly lipophilic CBD has been a recent point of investigation.
In nude mice, occluded application of ethanolized liposomes greatly increased drug accumulation in the skin and the underlying muscle. Steady-state levels were reached at about 24 hours and lasted at least until 72 hours, while also preventing carrageenan-induced inflammation and edema in the same animal model.6 Comparatively, in human skin, the solubility of CBD is 5.72umol/mL and the addition of 30.8% ethanol increased the solubility nearly three-fold to 16.2umol/mL, establishing ethanol as an important additive ingredient to enhance transdermal CBD bioavailability. CBD’s increased hydrophobicity also allowed for increased retention time relative to delta-9-tetrahydrocannabinol (THC).9 In a later experiment using guinea pigs, transdermal CBD was found to have high accumulation in the skin, but plasma concentration was increased 3.7-fold using an ethanol-derived permeation enhancer (Transcutol HP; Gattefossé, Saint-Priest, France).10 Together, these studies confirm that transdermal CBD with enhancing agents serves as a promising delivery route for CBD, but also underscore that simply standardizing the amount of CBD in a topical product might not be a valid indicator of the final bioavailability across products and vehicles.
Another common obstacle to CBD use is the lack of regulation of commercially available CBD products and the need for analytical testing to evaluate the sourcing of the active compound. For CBD products, a method incorporating gas chromatography-mass spectrometry has been validated for the qualitative analysis of cannabinoids in food and topicals, among others.11 For quantitative analysis of CBD products, however, a high-performance liquid chromatography-diode array detection method might be suitable, but extensive validation is still required.12 CBD products undergoing routine analysis with analytical studies could allow companies to manufacture purified compounds and remove impurities, such as those found in conventional plant-based samples.11
Of particular importance for patients using topical CBD products is possible contamination with THC due to the laws and mandated drug testing by individual organizations. As they remain unregulated and widely available, it might be difficult to definitively answer this question across commercial CBD products. It was found that oral consumption of low-content THC hemp oil (0.046mg of THC per 5-mL dose) did not result in positive biological assessments. No THC was detected in oral fluid, blood, or urine samples at any time point following consumption of low-content THC oil, with the exception of trace amounts of 11-nor-delta9-tetrahydrocannabinol-9-carboxylic acid (M=0.0001mg/L) in urine at four hours postconsumption.13 Additionally, while drug tests are primarily designed to detect the metabolites of smoked cannabinoids, some molecules cross-react with the test, generating false positives.14 Fortunately, CBD has low cross-reactivity (<0.1%) in at least some varieties of THC assays.14 However, no studies have confirmed the aforementioned findings using transdermal CBD preparations (with or without THC), and drug testing kits use different THC assays based on regional standards, rendering this a complex, unknown problem.
Without rigorous safety studies for transdermal CBD, data on adverse effects must be inferred through studies evaluating oral CBD treatment for epilepsy. CBD doses up to 300mg daily can be used safely for up to six months.15 However, some commonly reported adverse effects of oral CBD oil (Epidiolex; Greenwich Biosciences, Carlsbad, California) include somnolence, low appetite, diarrhea, and elevated liver function test results.16 CBD metabolism by cytochrome P450 might also result in drug-drug interactions, but these adverse effects might be minimized through the transdermal route due to delayed accumulation of drug levels.17 Moreover, since CBD oil preparations are not standardized, there are varying amounts of CBD/THC concentrations in commercial products.18
Cannabinoids do not appear to be highly allergenic or common contact allergens thus far and might actually be helpful in attenuating allergic contact dermatitis.19 However, the final products may contain contact allergens or irritants in the excipient and potentially aggravate dermatitis in patients using transdermal CBD preparations, reinforcing the need for appropriate labeling of these products.
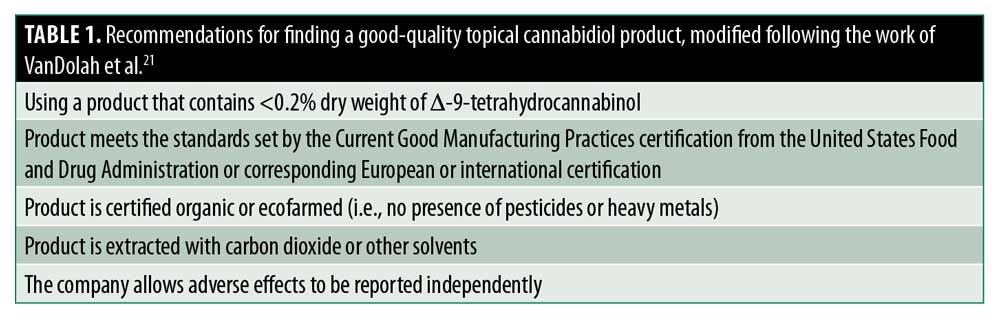
When educating patients on how to find a quality CBD/hemp oil product, products imported from Europe have been recommended over those originating in the United States due to stricter regulations.20 VanDolah et al21 have developed helpful guidelines that are worth enumerating (Table 1).
Despite the increased legalization of cannabis derivatives across multiple regions of the United States,21 CBD/hemp oils remain Schedule 1 substances federally. Following changes implemented under the 2018 Farm Bill, the United States Food and Drug Administration (FDA) has clarified some rules on cannabis derivatives and removed hemp from controls under the Controlled Substances Act.22 Although the FDA has stated that this can streamline the process to study CBD (that falls under the definition of hemp), it recognizes that the regulatory framework for CBD still needs updating. There are no standardization processes to ensure that commercially available CBD/hemp oil products are appropriately sourced or prepared. However, the FDA recommends that drug development follows the following general principles: characterization of CBD via a chemical fingerprint, routine testing for residual pesticides applicable to substances originating from botanical raw materials, microbial enumeration testing, elemental impurities testing, and principles on the assessment of extractables/leachables associated with pharmaceutical packaging or delivery.23 Selling CBD and hemp oils is legal if the THC content is below the 0.3% threshold in a majority of the United States. For solutions or solids, the THC percentage should be calculated with the amount of water removed from excipients (for more detail, see work from the Center for Drug Evaluation and Research23). The FDA routinely tests CBD products and warns organizations when data show irregularities in the labeling of the packages or concerns of additives, such as nitrosamines. Some of their concerns include false marketing and unproven medical claims, such as those touting CBD to be a viable treatment for coronavirus disease 2019.24
Moreover, regardless of these regulations, certain positions and private organizations have separate standards that mandate drug testing, so these questions will continue to be relevant, even in the event of federal legalization. If the source is certified to be free of THC or contain very low amounts of THC (defined as 0.046mg of THC per 5-mL dose), then topical application is unlikely to be detected in biological assessments. However, without regulations, patients and practitioners alike must exercise their use with caution due to differences in regional/local laws and the paucity of data regarding the efficacy and safety of other additive compounds
References
- Eagleston LRM, Kalani NK, Patel RR, et al. Cannabinoids in dermatology: a scoping review. Dermatol Online J. 2018;24(6):13030/qt7pn8c0sb.
- Jhawar N, Schoenberg E, Wang JV, Saedi N. The growing trend of cannabidiol in skincare products. Clin Dermatol. 2019;37(3):279–281.
- Chelliah MP, Zinn Z, Khuu P, Teng JMC. Self-initiated use of topical cannabidiol oil for epidermolysis bullosa. Pediatr Dermatol. 2018;35(4):e224–e227.
- Nickles MA, Lio PA. Cannabinoids in dermatology: hope or hype? Cannabis Cannabinoid Res. 2020;5(4):279–282.
- Samara E, Bialer M, Mechoulam R. Pharmacokinetics of cannabidiol in dogs. Drug Metab Dispos. 1988;16(3):469–472.
- Lodzki M, Godin B, Rakou L, et al. Cannabidiol-transdermal delivery and anti-inflammatory effect in a murine model. J Control Release. 2003;93(3):377–387.
- Benson HAE, Watkinson AC. Topical and Transdermal Drug Delivery: Principles and Practice. Hoboken, NJ: John Wiley & Sons; 2012: 464.
- Alexander A, Dwivedi S, Ajazuddin, Giri TK, Saraf S, Saraf S, et al. Approaches for breaking the barriers of drug permeation through transdermal drug delivery. J Control Release. 2012;164(1):26–40.
- Stinchcomb AL, Valiveti S, Hammell DC, Ramsey DR. Human skin permeation of Delta8-tetrahydrocannabinol, cannabidiol and cannabinol. J Pharm Pharmacol. 2004;56(3):291–297.
- Paudel KS, Hammell DC, Agu RU, Valiveti S, Stinchcomb AL. Cannabidiol bioavailability after nasal and transdermal application: effect of permeation enhancers. Drug Dev Ind Pharm. 2010;36(9):1088–1097.
- Ciolino LA, Ranieri TL, Taylor AM. Commercial cannabis consumer products part 1: GC-MS qualitative analysis of cannabis cannabinoids. Forensic Sci Int. 2018;289:429–437.
- Ciolino LA, Ranieri TL, Taylor AM. Commercial cannabis consumer products part 2: HPLC-DAD quantitative analysis of cannabis cannabinoids. Forensic Sci Int. 2018;289: 438–447.
- Hayley AC, Downey LA, Hansen G, et al. Detection of delta-9-tetrahydrocannabinol (THC) in oral fluid, blood and urine following oral consumption of low-content THC hemp oil. Forensic Sci Int. 2018;284:101–106.
- Grauwiler SB, Drewe J, Scholer A. Sensitivity and specificity of urinary cannabinoid detection with two immunoassays after controlled oral administration of cannabinoids to humans. Ther Drug Monit. 2008;30(4): 530–535.
- Cunha JM, Carlini EA, Pereira AE, et al. Chronic administration of cannabidiol to healthy volunteers and epileptic patients. Pharmacology. 1980;21(3):175–185.
- Franco V, Perucca E. Pharmacological and therapeutic properties of cannabidiol for epilepsy. Drugs. 2019;79(13):1435–1454.
- Lucas CJ, Galettis P, Schneider J. The pharmacokinetics and the pharmacodynamics of cannabinoids. Br J Clin Pharmacol. 2018;84(11):2477–2482.
- Bonn-Miller MO, Loflin MJE, Thomas BF, et al. Labeling accuracy of cannabidiol extracts sold online. JAMA. 2017;318(17):1708–1709.
- Karsak M, Gaffal E, Date R, et al. Attenuation of allergic contact dermatitis through the endocannabinoid system. Science. 2007;316(5830):1494–1497.
- Cherney JH, Small E. Industrial hemp in North America: production, politics and potential. Agronomy. 2016;6(4):58.
- VanDolah HJ, Bauer BA, Mauck KF. Clinicians’ guide to cannabidiol and hemp oils. Mayo Clin Proc. 2019;94(9):1840–1851.
- Conaway KM. Agriculture Improvement Act of 2018. Available at: https://www.congress.gov/bill/115th-congress/house-bill/2/text. Accessed September 18, 2020.
- Center for Drug Evaluation and Research. Cannabis and cannabis-derived compounds: quality considerations for Cl. Available at: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/cannabis-and-cannabis-derived-compounds-quality-considerations-clinical-research-guidance-industry. Accessed September 18, 2020.
- Office of the Commissioner. Warning letters and test results for cannabidiol-related products. Available at: https://www.fda.gov/news-events/public-health-focus/warning-letters-and-test-results-cannabidiol-related-products. Accessed September 18, 2020.

