 J Clin Aesthet Dermatol. 2021;14(8):52–56
J Clin Aesthet Dermatol. 2021;14(8):52–56
by Michael J. Murphy, MD and Aileen A. Dow
Dr. Murphy is with the Department of Dermatology, UConn Health in Farmington, Connecticut. Ms. Dow is with Si Skin Organics® in Canton, Connecticut.
FUNDING: No funding was provided for this article.
DISCLOSURES: The authors report no conflicts of interest relevant to the content of this article.
ABSTRACT: Background. Disorders of hyperpigmentation, such as melasma, postinflammatory pigmentary alteration, and lentigines, pose significant cosmetic concerns for women of Hispanic or Latino race and ethnicity. Natural ingredients are gaining popularity as alternative, safe, and effective topical depigmenting agents.
Objective. We sought to review clinical studies evaluating the use of natural ingredients in the topical management of hyperpigmentation in Hispanic and Latino women.
Methods. We conducted a systematic review of scientific and medical electronic databases to identity randomized controlled trials (RCTs) and nonrandomized reports on topical natural agents for the treatment of disorders of hyperpigmentation, using Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines.
Results. Our review of the literature revealed relatively few (N=7) clinical studies (including six RCTs) that evaluated the topical management of hyperpigmentation using natural ingredients with specific reference to women of Hispanic or Latino race and ethnicity. Despite limited research data, a small number (N=7) of natural ingredients demonstrated efficacy and safety as depigmenting agents in this cohort, including niacinamide, soy, azelaic acid, ascorbic acid, licorice, emblica, and belides.
Conclusion. Several natural ingredients have scientific data supporting their potential efficacy as topical treatments for disorders of hyperpigmentation in women of Hispanic or Latino race and ethnicity. However, the paucity of robust cosmetic trials in this setting reflects the generalized low representation of Hispanic and Latino individuals in clinical studies of other skin conditions. Many in-vivo cutaneous trials of natural ingredients are limited by their study design, including with respect to subject selection and short duration. Further research is needed to determine long-term efficacy, safety, optimal concentration, and formulation of natural ingredients for the topical management of hyperpigmentation in Hispanic and Latino women.
Keywords: Natural ingredients, hyperpigmentation, melasma, Hispanic, Latino
There is an increasing demand among consumers for naturally derived ingredients in skin care products with demonstrated efficacy and safety.1 Among patients with darker skin types, there is much interest in novel nonhydroquinone topical formulations that improve hyperpigmentation and promote an even skin tone.1
The terms “Hispanic” and “Latino” describe diverse racial and ethnic groups, encompassing a range of cultures, languages, and biological ancestries. They include individuals of Mexican, Central-to-South American, and Spanish-Caribbean (e.g., Cuban, Puerto Rican, and Dominican) descent.2 While there is much published research on cosmetic approaches in non-Hispanic and non-Latino cohorts, a paucity of data exist on the specific aesthetic needs of Hispanic and Latino patients and consumers.2
The objective of this review was to examine the literary evidence supporting the clinical utility of topical natural ingredients in the treatment of hyperpigmentation in women of Hispanic and/or Latino race and ethnicity.
Methods
According to the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) protocol,3 we performed a systematic search in January 2020 of topical treatments for cutaneous hyperpigmentation, using the PubMed, Cochrane, EMBASE, and SCOPUS databases. Search terms included “hyperpigmentation,” “melasma,” “dyschromia,” “melanosis,” “chloasma,” “lentigo,” “treatment,” “therapy,” “management,” “natural,” “Latino,” “Hispanic,” and “skin of color.”
Two reviewers independently screened articles based on inclusion and exclusion criteria. Included articles were randomized controlled trials (RCTs), nonrandomized reports, and conference abstracts that reported using topical natural (derived from nature; not man-made) ingredients for hyperpigmentation in women of Hispanic or Latino race and ethnicity. We excluded studies using proprietary or undescribed active ingredients, as these studies and outcomes would not be verifiable or reproducible by third parties, and those evaluating non-natural, nontopical agents (i.e., oral medications, bleaching agents, chemical peels, intralesionally administered drugs, and laser and light-based therapies) as stand-alone or combination approaches. Patients were allowed to apply daily sunscreen in the included studies. We examined the bibliographies of included articles and literature reviews to ensure that all relevant scientific reports were included in the systematic search.
Results
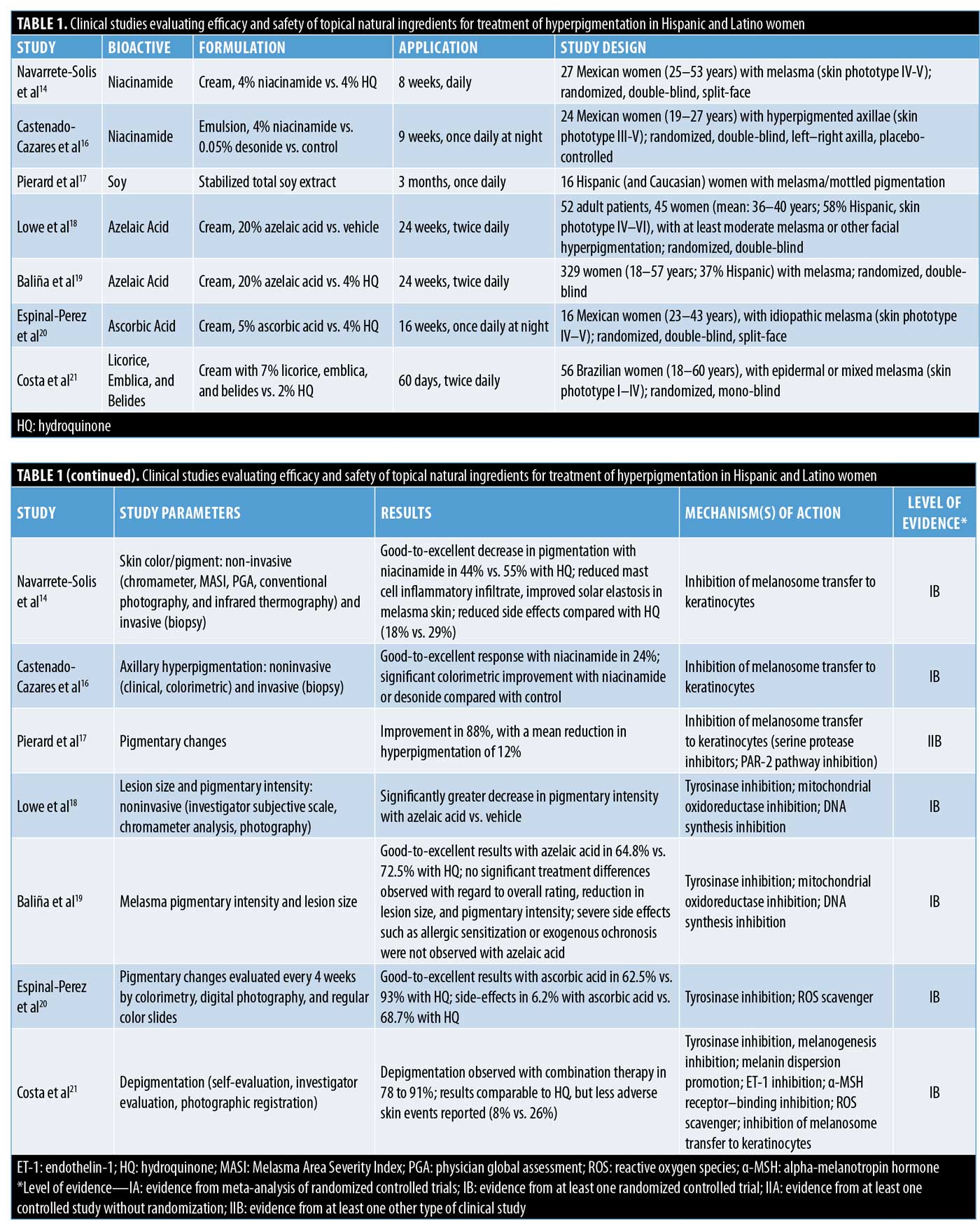
Studies that met our inclusion criteria are summarized in Table 1. Our systematic search identified 9,637 articles published from 2000 to 2020. After screening titles, abstracts, and full-text articles, we identified seven clinical studies (six RCTs and one conference abstract) that evaluated topical natural ingredients for the management of hyperpigmentation with specific reference to women of Hispanic or Latino race and ethnicity. A small number (n=7) of natural ingredients were reported to demonstrate promising efficacy and safety (i.e., low risk for adverse events) as depigmenting agents in this cohort, including niacinamide (n=2 studies); soy (n=1 study); azelaic acid (n=2 studies); ascorbic acid (n=1 study); and licorice, emblica, and belides (n=1 study). Table 1 provides a detailed summary of identified studies using topical natural ingredients for hyperpigmentation in Hispanic and Latino women and highlights study designs, treatment parameters, results, adverse events, and mechanisms of action.
Discussion
Disorders of hyperpigmentation are the fourth most commonly reported dermatoses in Hispanic and Latino individuals, posing significant cosmetic concerns, triggering psychosocial distress, and having negative impacts on self-image and quality of life.4–6 In a recent survey of 401 Hispanic and Latino American women (range: 30–65 years), 63 percent reported that they would consider treatments that address hyperpigmentation.2 Of note, 16 percent of respondents would not favor invasive procedures (i.e., injectables),2 indicating that topical therapies for hyperpigmentation are important for a significant proportion of Hispanic and Latino women. Risks of skin irritation and sensitivity with current treatments are also specific concerns among Hispanic and Latino patients.6 Therefore, identifying safe and effective treatments for disorders of hyperpigmentation are paramount in attaining favorable outcomes in this population.
Topical treatment of hyperpigmentation is largely aimed at reducing the production and/or distribution of epidermal pigment.4 The tyrosinase inhibitor, hydroquinone (HQ), alone or in combination with other bio-actives (i.e., retinoids), is considered the gold-standard topical treatment due to its established efficacy.4 However, the risk of skin irritation with these agents, and specifically exogenous ochronosis with long-term or excessive use of HQ, are limitations.4 Therefore, safety concerns among regulatory agencies and the general public are promoting the discovery and development of novel skincare products for the management of hyperpigmentation.
Natural ingredients have become increasingly popular as alternative topical treatments for hyperpigmentation. A number of these compounds have demonstrated promise in the management of disorders of hyperpigmentation in different racial and ethnic groups, based on the results of clinical trials.1,7–13 However, while efficacy and safety in “multiethnic” and “non-Caucasian” groups are often reported, very few studies specifically address the role of natural ingredients for the treatment of hyperpigmentation in Hispanic and Latino populations.1,7–13 To date, the natural ingredients with data supporting their safety and efficacy in treating disorders of hyperpigmentation in Hispanic/Latino women include niacinamide, soy, azelaic acid, ascorbic acid, licorice, emblica, and belides.
Niacinamide. Niacinamide is the biologically active amide of niacin (vitamin B3).14 This water-soluble vitamin is an important component of the body’s co-enzyme system and is essential to many cellular metabolic processes in the skin, including retaining moisture, maintaining oil balance, and repairing ultraviolet-induced DNA damage. In addition, niacinamide is reported to block the transfer of pigment (melanosomes) from melanocytes to keratinocytes.15 This potential therapeutic action distinguishes niacinamide from many other “brightening” compounds that directly inhibit tyrosinase (a key enzyme in melanin production). Navarrete-Solís et al14 previously evaluated the therapeutic effect of topical niacinamide versus HQ in Mexican patients with melasma; in their eight-week, randomized, double-blind clinical trial, 27 women applied 4% niacinamide cream on one side of the face and 4% HQ cream on the other. Sunscreen was also applied during the observation period. Patients were assessed by noninvasive techniques for the evaluation of skin color, subjective scales, and histological sections initially and after treatment with niacinamide, and all patients showed pigment improvement relative to baseline with both treatments (p<0.001).14 Good-to-excellent results were observed with niacinamide in 44 percent of patients compared to in 55 percent who were using HQ. Colorimetric analysis did not show statistical differences between niacinamide and HQ therapy (p=0.78).14 The lightening effect of niacinamide was noted at the second month of treatment, whereas results were evident with HQ as early as during the first month. However, side effects occurred on the niacinamide side in only 18 percent of patients (most mild) versus in 29 percent of patients on the HQ side (most moderate).14 Niacinamide also resulted in reduced inflammation and improvement of solar elastosis in biopsied skin. Navarrete-Solís et al14 concluded that topical niacinamide is an effective and well-tolerated therapeutic alterative to HQ in Mexican women with melasma. However, the authors cautioned that further clinical studies using niacinamide for longer periods are warranted. In another study of Mexican women, Castenado-Cazares et al16 reported significant improvement in axillary hyperpigmentation with niacinamide relative to placebo (p=0.03).
Soy. A number of biologically active compounds have recently been identified in soybeans, including isoflavones (antioxidants), vitamin E, and small serine protease inhibitors.12 In-vitro studies have confirmed the depigmenting action of serine protease inhibitors through the inhibition of a keratinocyte external membrane receptor called protease-activated receptor 2 (PAR-2). The PAR-2 pathway regulates keratinocyte-mediated phagocytosis of melanosomes. Therefore, PAR-2 inhibition results in decreased melanosome transfer to keratinocytes (similar to the action of niacinamide).12 In a clinical trial by Pierard et al,17 16 Hispanic women with melasma applied a stabilized total soy extract once daily for three months to a single melasma lesion, while a second melasma lesion served as an untreated control. At the end of the study, 14 out of 16 subjects showed some degree of melasma improvement; hyperpigmentation was reduced on average by 12 percent.17
Azelaic acid. Azelaic acid (AzA) is a saturated nine-carbon dicarboxylic acid derived from the fungus Pityrosporum ovale and is found in rye, wheat, and barley.7 It interferes with deoxyribonucleic acid (DNA) synthesis, inhibits mitochondrial oxidoreductase, decreases free radical formation, and competitively inhibits tyrosinase. AzA preferentially targets abnormal and highly active melanocytes, with reported minimal effects on uninvolved skin.7 Lowe et al18 evaluated 20% AzA cream for facial hyperpigmentation in a randomized, double-blind, parallel-group trial of 52 patients (skin phototypes IV–VI), of which 58 percent were Hispanic. Following the 24-week treatment period, AzA produced significantly greater decreases in pigmentary intensity than the vehicle as measured by both the investigator’s subjective scale (p=0.021) and chromameter analysis (p=0.039). There was significantly greater global improvement with AzA at Weeks 12 (p=0.026), 20 (p=0.030), and 24 (p=0.008).18 Despite other measures of efficacy showing AzA superiority, no significant between-group differences with respect to lesion area were identified. AzA produced a slightly but significantly greater amount of burning (Weeks 4 and 12; p or less than 0.046) and stinging (Week 4; p=0.002) compared with vehicle. At the end of the study, more AzA patients reported having much smoother skin and being very satisfied or satisfied with their treatment.18 In another study, Baliña and Graupe19 evaluated the efficacy of 20% AzA versus 4% HQ in the treatment of melasma in 329 women, 37 percent of whom were Hispanic. In this 24-week, randomized, double-blind trial, there was a 71-percent reduction in median lesion size in the AzA group and a 78-percent reduction in lesion size in the HQ group. A greater than 50-percent reduction in initial lesion size was seen in 60 percent and 66 percent of patients using AzA and HQ, respectively.19 A reduction by one to three levels of pigment intensity appeared in 84.2 percent and 89.2 percent of patients using AzA and HQ, respectively. There was no significant difference between the two groups regarding either lesion size or pigment intensity.19 Good or excellent overall results were achieved by 64.8 percent (n=79 patients) of the AzA group versus 72.5 percent (n=87 patients) of the HQ group (p not significant). Pronounced local irritation was observed in one HQ patient (burning) and 18 AzA patients (itching or burning).19
Ascorbic acid. Ascorbic acid has important effects on hyperpigmentation via a number of mechanisms.20 It regulates the monopherase activity of tyrosinase through its ability to decrease enzymatically generated o-quinones, thus reducing melanin synthesis. In addition, ascorbic acid has photoprotective and antioxidant effects, preventing the absorption of ultraviolet radiation (both ultraviolet A and B), inhibiting the production of free radicals, which trigger melanogenesis, and minimizing levels of oxidized melanin.20 In addition, ascorbic acid is a promoter of collagen synthesis, reducing dermal damage and leading to reparative keratinocyte differentiation. In a 16-week clinical study by Espinal-Perez et al,20 16 Mexican women with idiopathic melasma applied 5% ascorbic acid cream nightly on one side of the face and 4% HQ cream nightly on the other side. Sunscreen was applied daily throughout the period of observation. Patients were evaluated every month by colorimetry, digital photography, regular color slides, and subjective review, and good-to-excellent results were found in 62.5 percent of study subjects with ascorbic acid compared to in 93 percent of those using HQ.20 However, side effects were noted in 68.7 percent (11/16) using HQ versus 6.2 percent (1/16) using ascorbic acid. The authors concluded that, although HQ showed a better response, ascorbic acid might have a role in mono- or combination therapy of melasma because of its safety profile.20
Licorice, emblica, and belides. Licorice extract (derived from Glycyrrhiza glabra root) is known to contain a number of flavonoid compounds with depigmenting properties in the skin, including glabridin, liquirtin, and isoliquirtin.7 Glabridin has been shown to inhibit ultraviolet B-induced pigmentation and tyrosinase without affecting DNA synthesis. The skin-lightening effect of glabridin is reported to be 16 times greater than that of HQ.7 Emblica, which is extracted from Indian gooseberry (Emblica officinalis), is also thought to have skin-lightening and antioxidant properties.1 Belides is derived from organic daisy flowers (Bellis perennis) and reduces skin pigmentation via multiple anti-melanogenesis mechanisms (including endothelin-1 inhibition, alpha-melanotropin hormone receptor-binding inhibition, reactive oxygen species scavenging, and the inhibition of melanosome transfer to keratinocytes).21 Costa et al21 evaluated the efficacy and safety of 7% licorice, emblica, and belides combination therapy relative to those of 2% HQ in 56 Brazilian women with melasma. In this 60-day clinical trial, subjects were divided into two different groups: one in which a cream with licorice, emblica, and belides was applied twice daily and one in which a cream with 2% HQ was used at night. Follow-up assessments were performed every 15 days. Depigmentation was observed through investigator evaluation (Group A: 78.3%; Group B: 88.9%) and subjects’ self-evaluation (Group A: 91.3%; Group B: 92.6%); these results were statistically significant (p<0.001), with no differences between the groups (p>0.05).21 This pattern of results was observed by photographic registration (Visia®; Canfield Scientific, Fairfield, New Jersey) in the number (p=0.001) and size and tone (p<0.001) of ultraviolet stains in both groups, with no differences between them (p>0.05). Two volunteers in Group A and seven in Group B had mild cutaneous adverse events. Costa et al21 concluded that, while no statistical differences were observed between groups in the improvement of melasma, the combination of natural ingredients was associated with less skin adverse events. Therefore, the use of topical licorice, emblica, and belides might be a safe and effective alternative to HQ in the treatment of melasma.21
The natural ingredients (n=7) reviewed in this study show promise as safe and effective depigmenting agents in Latino and Hispanic patients, potentially acting via different pathways/mechanisms including the inhibition of melanosome transfer to keratinocytes (niacinamide, soy)14–17 and tyrosinase inhibition (azelaic acid, ascorbic acid, licorice, emblica, belides).18–21 Previous studies have provided evidence-based data supporting the clinical utility of additional natural compounds for the treatment of hyperpigmentation in other populations (including aloesin, mulberry, lignin peroxidase, kojic acid, ellagic acid, arbutin, green tea, turmeric, silymarin, N-acetyl-glucosamine, glutathione, and marine macroalgae-derived actives).1,7–13 Therefore, future research to assess these and other natural ingredients, both alone and in combination (i.e., thereby targeting different steps of the pigmentation pathway, in an effort to produce additive/synergistic effects and improve outcomes), in the treatment of disorders of hyperpigmentation in Hispanic and Latino patients is warranted.
Our research revealed relatively few (n=7) clinical studies of natural topical ingredients for the management of hyperpigmentation specifically in women of Hispanic and/or Latino race and ethnicity. A recent systemic review by Charrow et al,22 evaluating RCTs for a range of dermatologic conditions found that Hispanic and Latino representation among study participants was lower than that of the general population. The paucity of robust cosmetic trials for hyperpigmentation in Hispanic and Latino women identified in our study reflects the generalized low representation of this cohort in other clinical studies of skin disorders. Importantly, in a recent survey of 686 Hispanic and Latino American women (range: 18–50+ years), 66 percent reported feeling underrepresented in skincare advertising and 38 percent did not believe the beauty industry creates products specifically for their cosmetic concerns.23
Conclusion
Disorders of hyperpigmentation represent specific concerns among Hispanic and Latino women, demanding targeted cosmeceutical solutions. However, this population is currently underrepresented in the media, advertisements, and focus product development, testing, and marketing. To date, there are relatively few studies of topical natural ingredients for the treatment of hyperpigmentation in women of Hispanic and/or Latino race and ethnicity. Further research using well-designed clinical trials is needed to determine long-term efficacy, safety, optimal concentration, and formulation of natural ingredients for the topical management of hyperpigmentation in Hispanic and Latino women.
References
- Alexis AF, Blackcloud P. Natural ingredients for darker skin types: growing options for hyperpigmentation. J Drugs Dermatol. 2013;12(9 Suppl):s123–s127.
- Fabi S, Montes JR, Aguilera SB, et al. Understanding the female Hispanic and Latino American facial aesthetic patient. J Drugs Dermatol. 2019;18(7):623–632.
- Moher D, Shamseer L, Clarke M, et al; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1.
- Alexis AF, Obioha JO. Ethnicity and aging skin. J Drugs Dermatol. 2017;16(6):s77–s80.
- Del Bino S, Duval C, Bernerd F. Clinical and biological characterization of skin pigmentation diversity and its consequences on UV impact. Int J Mol Sci. 2018;19(9):2668.
- Hexsel D, Arellano I, Rendon M. Ethnic considerations in the treatment of Hispanic and Latin-American patients with hyperpigmentation. Br J Dermatol. 2006;156 Suppl 1:7–12.
- Hollinger JC, Angra K, Halder RM. Are natural ingredients effective in the management of hyperpigmentation? A systematic review. J Clin Aesthet Dermatol. 2018;11(2):28–37.
- Huerth KA, Hassan S, Callender VD. Therapeutic insights in melasma and hyperpigmentation management. J Drugs Dermatol. 2019;18(8):718–729.
- Fisk WA, Agbai O, Lev-Tov HA, Sivamani RK. The use of botanically derived agents for hyperpigmentation: a systematic review. J Am Acad Dermatol. 2014;70(2):352–365.
- Austin E, Nguyen JK, Jagdeo J. Topical treatments for melasma: a systematic review of randomized controlled trials. J Drugs Dermatol. 2019;18(11):1156–1171.
- Gonzalez N, Perez M. Natural cosmeceutical ingredients for hyperpigmentation. J Drugs Dermatol. 2016;15(1):26–34.
- Leyden JJ, Shergill B, Micali G, et al. Natural options for the management of hyperpigmentation. J Eur Acad Dermatol Venereol. 2011;25(10):1140–1145.
- Fitton JH, Dell’Acqua G, Gardiner VA, et al. Topical benefits of two fucoidan-rich extracts from marine macroalgae. Cosmetics. 2015;2(2):66–81.
- Navarrete-Solís J, Castanedo-Cázares JP, Torres-Álvarez B, et al. A double-blind, randomized clinical trial of niacinamide 4% versus hydroquinone 4% in the treatment of melasma. Dermatol Res Pract. 2011;2011:379173.
- Hakozaki T, Minwalla L, Zhuang J, et al. The effect of niacinamide on reducing cutaneous pigmentation and suppression of melanosome transfer. Br J Dermatol. 2002;147(1):20–31.
- Castanedo-Cazares JP, Lárraga-Piñones G, Ehnis-Pérez A, et al. Topical niacinamide 4% and desonide 0.05% for treatment of axillary hyperpigmentation: a randomized, double-blind, placebo-controlled study. Clin Cosmet Investig Dermatol. 2013;6:29–36.
- Pierard G, Graf J, Gonzalez R, Cauwenbergh G. Effects of soy on hyperpigmentation in Caucasian and Hispanic populations. Poster presented at: 59th Annual Meeting of the American Academy of Dermatology. March 2–7, 2001; Washington, DC.
- Lowe NJ, Rizk D, Grimes P, et al. Azelaic acid 20% cream in the treatment of facial hyperpigmentation in darker-skinned patients. Clin Ther. 1998;20(5):945–959.
- Baliña LM, Graupe K. The treatment of melasma. 20% azelaic acid versus 4% hydroquinone cream. Int J Dermatol. 1991;30(12):893–895.
- Espinal-Perez LE, Moncada B, Castanedo-Cazares JP. A double- blind randomized trial of 5% ascorbic acid vs. 4% hydroquinone in melasma. Int J Dermatol. 2004;43(8):604–607.
- Costa A, Moisés TA, Cordero T, et al. Association of emblica, licorice and belides as an alternative to hydroquinone in the clinical treatment of melasma. An Bras Dermatol. 2010;85(5):613–620.
- Charrow A, Xia FD, Joyce C, Mostaghimi A. Diversity in dermatology clinical trials: a systematic review. JAMA Dermatol. 2017;153(2):193–198.
- Houghton A, Thayer C. Latinos and beauty as we age: a cultural reflection. Available at: https://www.aarp.org/research/topics/life/info-2019/latinos-and-beauty.html. Accessed April 17, 2020.

