J Clin Aesthet Dermatol. 2024;17(1):33–40.
J Clin Aesthet Dermatol. 2024;17(1):33–40.
by Patrícia Froes Meyer, PhD; Fabio dos Santos Borges, ME; Ciro Dantas Soares, PhD;
Angelo Roncalli Oliveira Guerra, PhD; Rodrigo Marcel Valentim da Silva, PhD; Eneida de Morais Carreiro, ME; Custódio L. de Brito Guerra, PhD; Ana Laura Martins de Andrade, PhD; and Glenda Maria De Oliveira, ME
Drs. Carreiro, Soares, and Meyer are with the International Research Group in Rio Grande do Norte, Brazil. Dr. Borges is with the Universidade Estácio de Sá in Rio de Janeiro, Brazil. Drs. Oliveira Guerra and de Brito Guerra are with the Universidade Federal do Rio Grande do Norte in Rio Grande do Norte, Brazil. Dr. Valentim da Silva is with Universidade Estácio de Sá in Rio Grande do Norte, Brazil. Dr. Andrade is with Universidade Brasil in São Paulo, Brazil. Dr. Maria De Oliveira is with Centro Universitário do Rio Grande do Norte in Rio Grande do Norte, Brazil.
FUNDING: No funding was provided for this article.
DISCLOSURES: The authors report no conflicts of interest relevant to the content of this article.
ABSTRACT: The plasma jet is a non-surgical and minimally invasive procedure that acts by heating the superficial region of the skin, providing rejuvenation of the region.
Objective. We sought to compare the clinical and histological effects of direct plasma jet versus electrocarbonization without plasma in the treatment of wrinkles in the upper palpebral region.
Methods. This is a clinical trial in which 20 volunteers participated and divided into two groups: electrocarbonization (EG) and plasma jet (JPG), which were clinically evaluated before and after treatment through evaluation protocols, photographs, and questionnaires. Three treatment sessions were performed in the upper eyelid region with an interval of 30 days. After the treatment, a surgical procedure of upper blepharoplasty was performed on two volunteers to remove a skin fragment and later histological analysis.
Results. The JPG showed better clinical responses in rejuvenation. The EG promoted an increase in the number of fibroblasts, the number of blood vessels and the amount of inflammation. The JPG showed an increase in the number of fibroblasts and blood vessels. It was observed that the JPG generated activation of T lymphocytes (CD3), macrophages (CD68), and plasmocytes (CD138); in addition to reducing the number of positive cells for CD57 (NK cells). The satisfaction analysis shows that 100 percent in the JPG considered themselves satisfied with the treatment.
Conclusion. We verified that in comparison with electrocarbonization, the use of a direct plasma jet promoted tissue improvement at the histological level, in addition to fewer adverse reactions.
Keywords: Facial rejuvenation, plasma jet, Wrinkles
Cutaneous aging is characterized as a complex biological process involving changes in multiple physiological parameters of the skin and has attracted considerable attention from researchers and clinicians from different areas in the search for innovative non-surgical treatments. During the aging process, the characteristics of the skin are altered, with a decrease in fibroblasts, compromising the activity of collagen and elastin proteins, responsible for the support and elasticity of the skin.1,2
One of the most striking signs of the facial aging process is the appearance of periorbital wrinkles and palpebral sagging.3 Such alterations result from factors such as intrinsic aging, gradual loss of skeletal muscle mass, subcutaneous adipose tissue atrophy, and extrinsic factors, which are related to environmental damage, exposure to ultraviolet radiation, and lifestyle habits.2 At the biochemical level, the laminar expansion of the elastic fibers is observed, which become tiny and fragmented, between the collagen bundles, promoting a reduction in the proportion of collagen Type I to Type III.
In the clinical practice of treating facial aging, two resources have stood out with similarity in the form of application, indication and promoted effects, namely the plasma jet and electrocarbonization, however the mechanisms of action of these resources are different.
Generally, we find two types of therapeutic plasma equipment: direct plasma (i.e., dielectric barrier discharge [DBD]) and indirect plasma (i.e., plasma torch). In indirect plasma treatment, plasma is produced in a remote cavity and ejected by a skin gas flow as an effluent. In direct plasma treatment, the skin itself acts as a “counter electrode”. Advantages of direct plasma treatment include higher plasma density and high-frequency electrical current induced in the skin.4
The direct plasma jet has been presented as an innovative resource with promising results in treating skin aging. This resource is characterized by the passage of an electric current that can be alternating or continuous, applied in the “space” between the emitting tip of the equipment and the patient’s skin. Thus, the atmospheric air in that area is subjected to a high voltage, giving rise to an electric current that makes it conductive,5 forming reactive oxygen species (ROS), reactive nitrogen species (RNS), in addition to other gases (OH, NO and O3), which have protective and antibacterial effects on tissues, thus producing controlled thermal lesions on the superficial layers of the skin.6–8 Notably, the humidity present in the air can increase the production of ROS by the plasma jet.6
Electrocarbonization without plasma production uses an electric current, which is activated when the applicator tip of the equipment comes into direct contact with the tissue to be treated, thus promoting a sudden increase in the local temperature, causing vaporization of the water content in the tissue, producing superficial and even deep thermal injuries, which can fragment the tissue.6
Despite the extensive clinical practice regarding these resources, there was a lack of studies comparing the use of plasma jet and electrocarbonization in the treatment of eyelid rejuvenation. In addition, it is observed that the various devices sold as plasma jet all around the world do not emit constant plasma, so it is necessary to identify the quality and quantity of plasma emitted by the devices studied.8 Therefore, this study aims to compare the effects of using the direct plasma jet with the use of electrocarbonization without plasma in the treatment of wrinkles in the upper palpebral region, determining their clinical and histological results, in addition to characterizing the plasma emission of the equipment.
Methods
Characterization, research location and ethical considerations. This was a clinical pilot study in which participants were recruited through project dissemination through media and social platforms. Volunteers who sought to participate in the study were seen at the outpatient clinic of Clínica Eterna do International Research Group (IRG) in Natal/RN. The present study was submitted to the Research Ethics Committee (CEP) of Universidade Potiguar- UnP, approved with opinion number 3,993,426.
After recruiting the volunteers, all were informed about the procedures to be performed and those who agreed signed the free and informed consent term.
Population and sample. The sample included in this study consisted of 20 women, aged between 45 and 65 years, who had facial skin aging in the upper eyelid region (tissue flaccidity of the eyelid, wrinkles, elastosis), who did not have healing problems, keloids, or collagen-related disorders, as well as serious metabolic diseases. Volunteers who gave up the treatment before the end of the interventions, were absent from evaluations or sessions, and who had any complications after the application were excluded.
The volunteers were randomly divided into two groups with 10 volunteers in each. One group received the application of electrocarbonization (EG) as an intervention and the other group applied direct plasma jet (JPG).
Interventions. The procedures were performed on all volunteers in a standardized way, with them positioned in dorsal decubitus. The intervention application area in each participant was the region of both upper eyelids. All volunteers received three treatment sessions with an interval of 30 days between sessions.
Before applying the interventions, the volunteers were instructed to wash the eye region with antiseptic soap to remove sweat, oiliness, makeup, etc. The eyelid region was disinfected using an antiseptic solution soaked in gauze on all participants.
Direct plasma jet. For better use of the plasma jet, the equipment used to certify the quality and quantity of the plasma emission of the equipment used was carried out at the LabPlasma /LAIS of the Federal University of Rio Grande do Norte (UFRN) to determine the dosimetry ideal application of the resource.
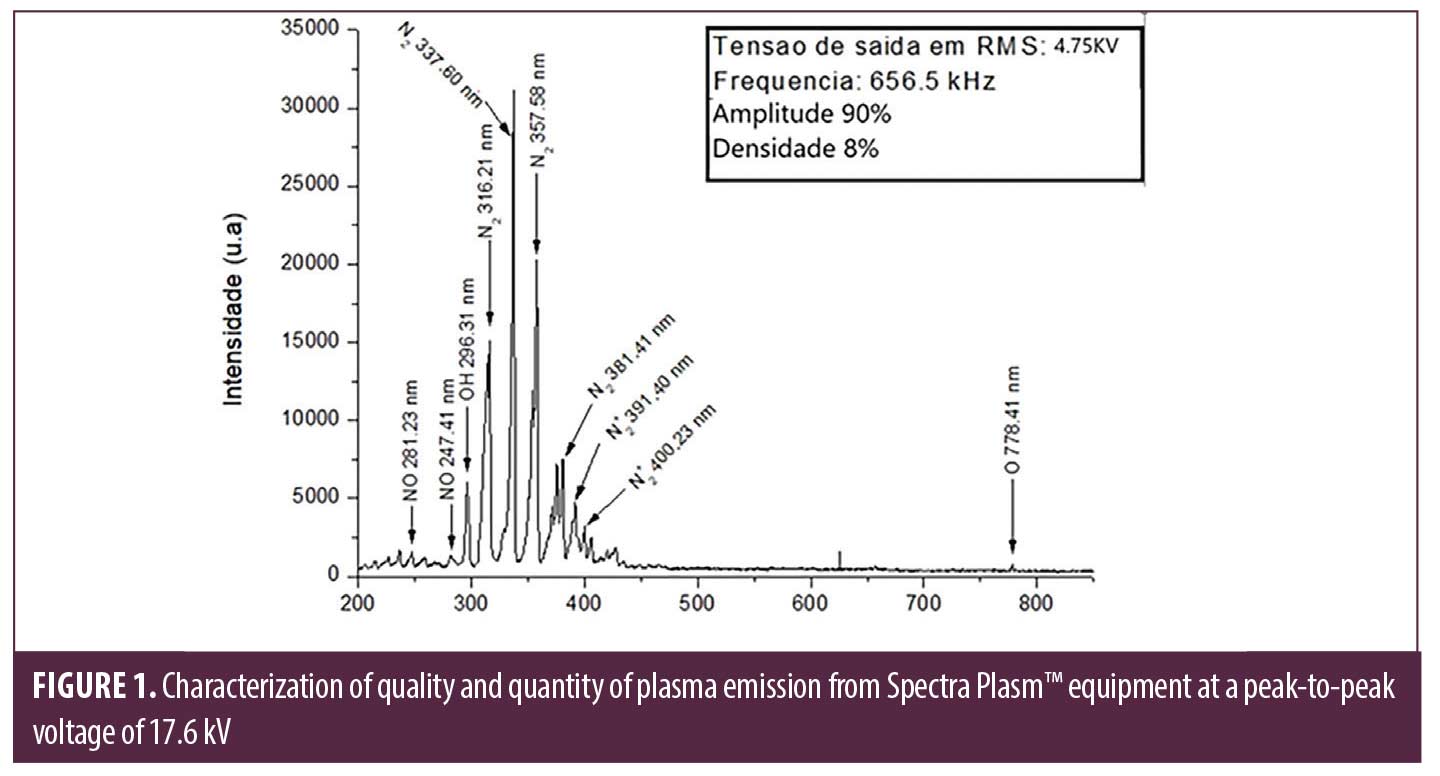
For characterization and subsequent application, the Spectra equipment was used. Artis™ (Tonederm Caxias do Sul/RS, Brazil) being considered for the intervention the parameters that had the capacity to promote the formation of large amounts of nitrogen and isotopes of nitrogen, OH, NO and oxygen (Figure 1). The characterization analysis followed the same protocol described by Guerra et al.8
After laboratory analysis, the following dosimetry parameters were defined for use in the treatment: Continuous mode, amplitude 90 percent, and density 8 percent (Figure 1).
For the treatment, in addition to the adjustments defined in the laboratory analysis, plasma formation was obtained using the isolated needle tip and punctual technique. The applications were performed at a distance of 0.5cm over the palpebral line on both sides.
Before each session, topical anaesthetic (Pliaglis™; Galderma, Lausanne, Switzerland) was applied to the entire palpebral region, then the area was covered with clean, dry gauze. After 30 minutes, the gauze was removed along with the residual anaesthetic, and the treatment began.
Electrocarbonization. Electrocarbonization was carried out using the New Skin® equipment (MM Optics São Carlos/SP, Brazil) adjusting the dosimetry level with the red lights on the panel (totally or partially according to the sensitive threshold of each treated volunteer ), using the formation of the electric arc, the thinnest tip available, with an intensity of 4 to 8mA. The punctual technique was used, concentrating the points above the palpebral wrinkle line with a distance of 0.5cm between each point.
It should be noted that before the electrocarbonization, the anaesthetic was applied to the upper eyelids, as described in the application of the plasma jet.
Evaluation instruments. The application of the PAF (Facial Assessment Protocol) was performed before the beginning of the interventions. The protocol consists of a questionnaire with the main objective of identifying the alterations present in the face, allowing specific and appropriate treatment for each patient. The questionnaire has the following topics: identification, anamnesis, physical examination, analysis of wrinkles and skin sagging through the Goglau and Lapier and Pierard classifications, phototype classification (Fitzpatrick) and Tsuji classification.9 Photographic records were taken before the first treatment session and 30 days after the last session, with a conventional camera and a 3D recording camera. For the conventional record, an iPhone 10 XS cell phone camera was used, with the volunteers positioned in a standardized way, in orthostatism, in the anterior and lateral view (right and left), with a distance from the camera of 55cm, which is positioned on a tripod with 70cm high. The photos were recorded with the same artificial light of the place in both moments.
For the 3D records, the VISIATM scan equipment was used. (MED Systems São Paulo/SP, Brazil) which makes it possible, through 3D images, to accurately identify and quantify skin aesthetic alterations.
Volunteers answered the Patient Satisfaction Analysis questionnaires, Segot-chicq et al10and the Global Aesthetic Scale Improvement Scale – GAIS, by Narins et al,11 which is used to classify responses to treatments, allowing a comparative assessment at different times after therapeutic intervention. These evaluations occurred at two different times: on the first day of treatment and 30 days after the last session.
Morphological evaluation. For a better understanding of the mechanisms of action and effects promoted in the cutaneous tissue after the interventions, the skin biopsy technique of the upper eyelids was performed on two volunteers, one from each group at random, during the surgical procedure of blepharoplasty, 30 days after the last treatment session. The procedure was performed by a plastic surgeon at Hospital Angiovascular, Natal – RN, so a small fragment of skin was removed from each eyelid for analysis.
Notably, the intervention protocol for these volunteers was similar to that described above. Still, for these participants only the upper right palpebral region received the intervention, while the left was maintained as control of the procedures.
For the surgical procedure, the volunteer was sedated, with local anaesthesia, with an injection of 2% lidocaine with 1:200,000 adrenaline, an incision was made in the upper palpebral margin, with the removal of skin flap and adipose tissue, and an absorbable suture was used Vicryl 3-0 for finishing the procedure.
Histological analysis. To make the slides, the samples were embedded in paraffin, and the tissue was sectioned at 5μm thick for qualitative analysis, performed using a light microscope (Olympus, X100). The slides were stained using haematoxylin and eosin (HE) for evaluation of the acute and chronic inflammatory process, presence of fibroblasts, neo collagen. Staining with Masson’s Trichrome was also performed for proper differentiation of collagen fibers.
Birefringence analysis. Slides were stained with Picrosirus Red in order to observe the organisation and quantify the types of collagens I and III. Three images were captured, per section, in a polarised optical microscope (OLYMPUS BX53) with 400x magnification.
Immunohistochemical Analysis (IHC). To detect the inflammatory profile and cellular stimulation promoted by the interventions, IHC analyses were performed using the samples obtained in the blepharoplasty surgery, using the antibodies with their respective dilutions described in Table 1.
Tissue samples were stained with a non-primary negative control and a human skin positive control. Heat-induced antigen retrieval was performed with Leica Bond Epitope Retrieval Buffer 1 (citrate buffer, pH 6.0) for 20 minutes. The binding of non-specific antibodies was blocked with Novolink protein Block for 10 minutes. Primary antibodies (Table 1) were applied following the manufacturer’s recommendations. Colourimetric detection was performed with diaminobenzidine substrate (DAB, SK-4100, Vector Laboratories, Burlingame, CA, USA) and haematoxylin.
Three images of each slide were captured at 40x magnification, and qualitative analysis was performed for each sample.
Data analysis. Descriptive and inferential statistics of the data were performed using the SPSS 22.0 program (Statistical Package for the Social Science- version 22.0). Data normality was observed using the Kolmogorov-Smirnov (KS) test. For comparisons of measurements obtained in all assessments (initial and final), the ANOVA test for repeated measures with post hoc Bonferroni was used. A significance level of 95 percent (p<0.05) was adopted.
Results
Twenty volunteers who met the inclusion and exclusion criteria of the study participated in the study. There were two withdrawals during the research, and the study ended with 18 participants. The age range of the EG was 41.2 ± 2.11 years and the JPG 39.2 ± 1.9 years.
Table 2 presents the results regarding the application of the PAF questionnaire, which describes the characteristics of the population. In both groups there is a predominance of patients with mixed skin (50% in each group), Skin Phototype II, EG (50%) and JPG (60%). On the Goglau scale, there is a predominance of Grade II in the EG (67%) and Grade III in the JPG (80%). Both groups showed associated static and dynamic wrinkles in the electrocarbonization group (67%) and the plasma jet group (67%). In the Tsuji scale, the presence of superficial and dynamic wrinkles was observed in the EG (75%) and JPG (40%) and in the Lapiere and Pierard scale, grade III is predominant in the EG (92%) and JPG (44% ).
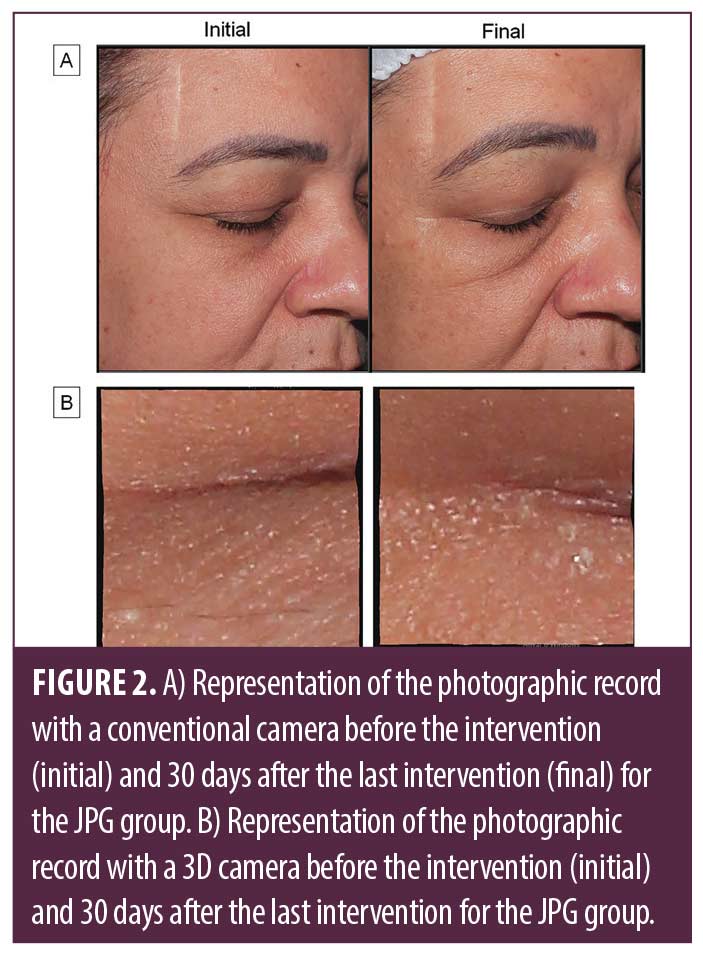
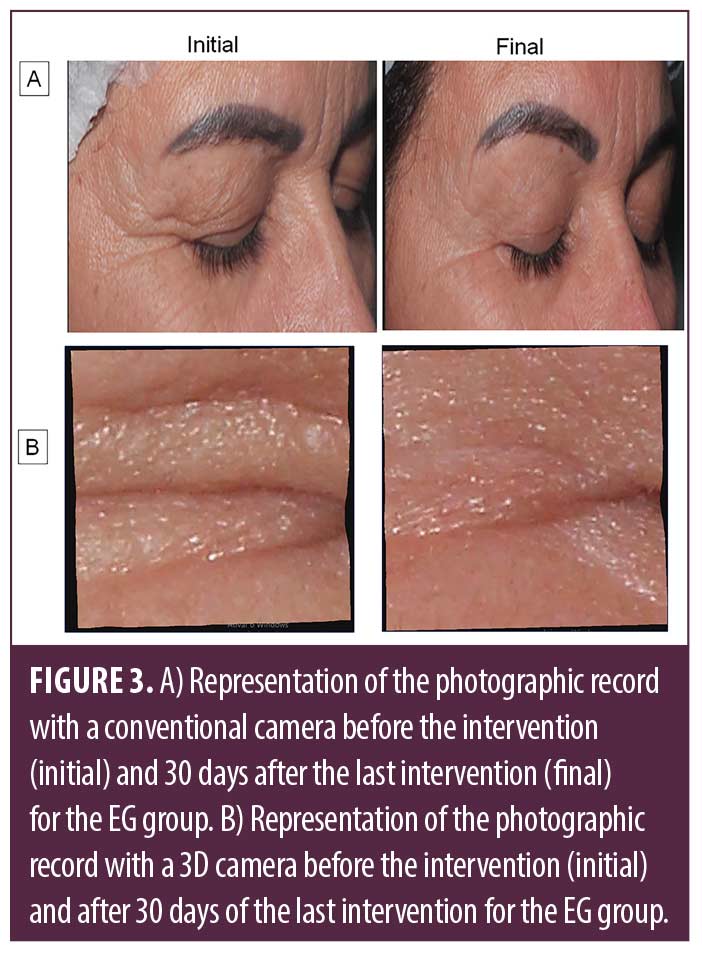
Figure 2 represents the photographic records obtained in the conventional mode and in 3D for the JPG. Through qualitative analysis, it was possible to observe, through the 3D images, the smoothing of periorbital wrinkles and improvement of the general appearance of the skin at the end of the treatment in all participants.
Figure 3 represents the group that received the electrocarbonization (EG) intervention through photographic records. In the 3D images, all participants also showed smoothing of periorbital wrinkles.
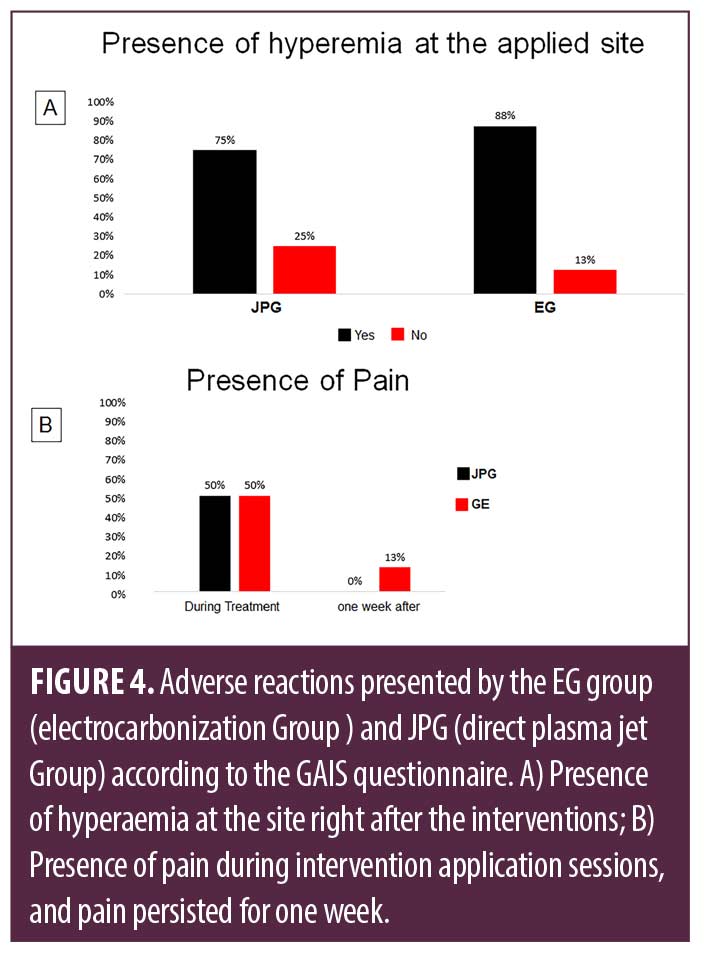
The GAIS questionnaire represented in Figure 4 suggests that the participants who received the treatment with direct plasma jet had fewer adverse effects than those who received the application of electrocarbonization as an intervention. Of the participants, 88 percent of the EG reported hyperaemia at the site after the interventions, while for the JPG the report was 75 percent. In the item about the presence of pain, both groups presented similar responses during treatment, however, 13 percent of the GP volunteers stated that the pain remained for one week.
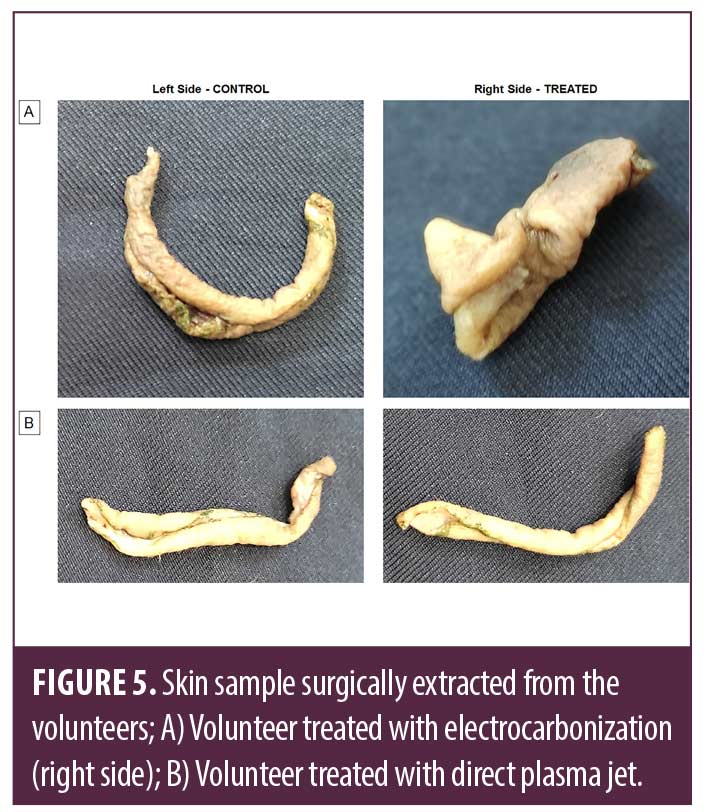
Figure 5 presents the skin tissue samples surgically extracted from the volunteers who received treatment with direct plasma jet and electrocarbonization. It is possible to observe that the volunteer who received the application of the direct plasma jet presented a more intact tissue sample (Figure 5b) compared to the sample of the volunteer treated with electrocarbonization, being visible the retraction of the tissue in the collected sample (Figure 5a).
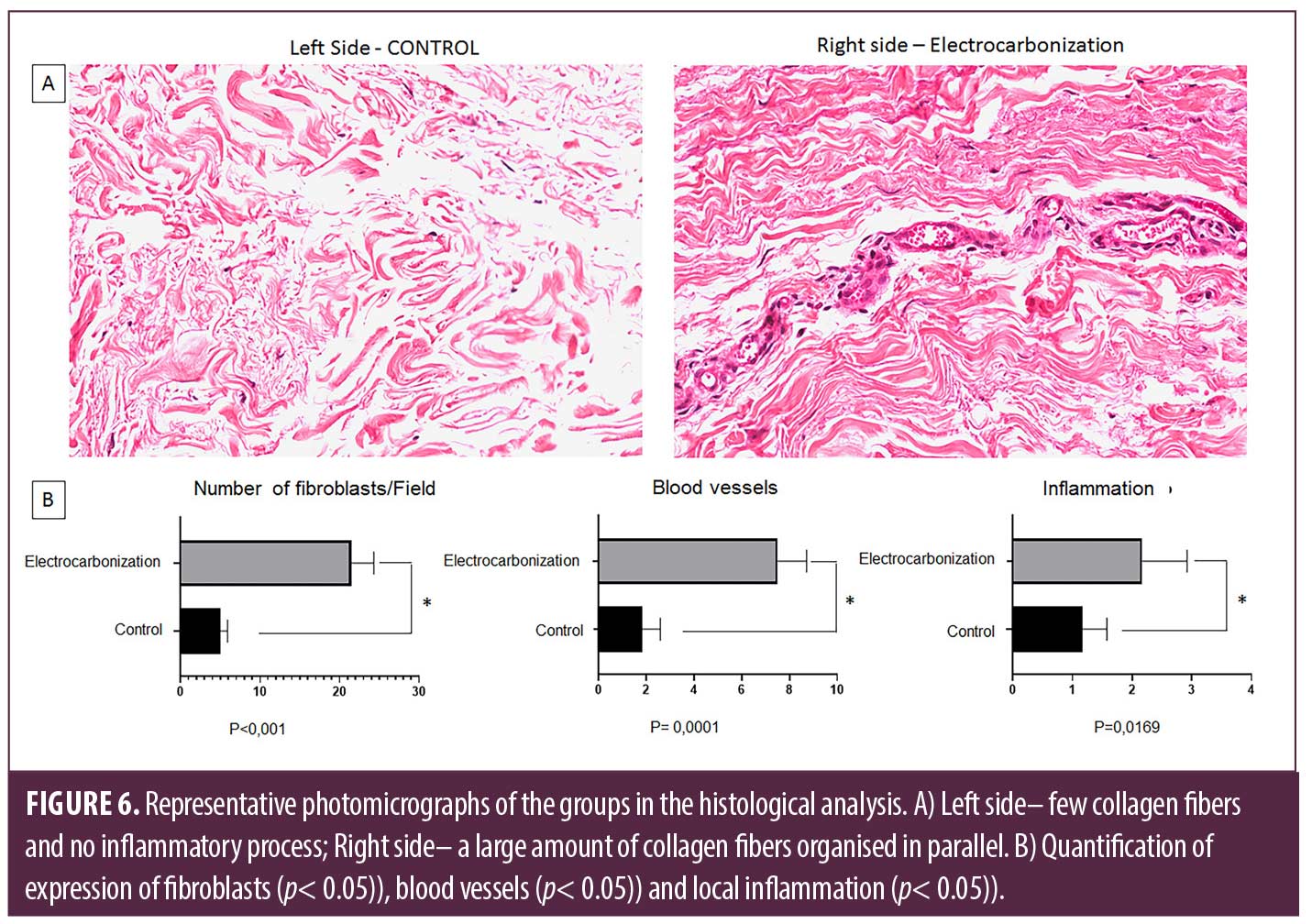
Figure 6 shows the histological analysis of the volunteer treated with electrocarbonization, comparing the left side (control) and the right side (experimental). It can be seen that the side that received the treatment showed an increase in the production of bulky collagen fibers, an increase in the number of fibroblasts (p=0.001), in addition to an increase in the number of blood vessels (p=0.001) and expression of inflammation (p=0.01).
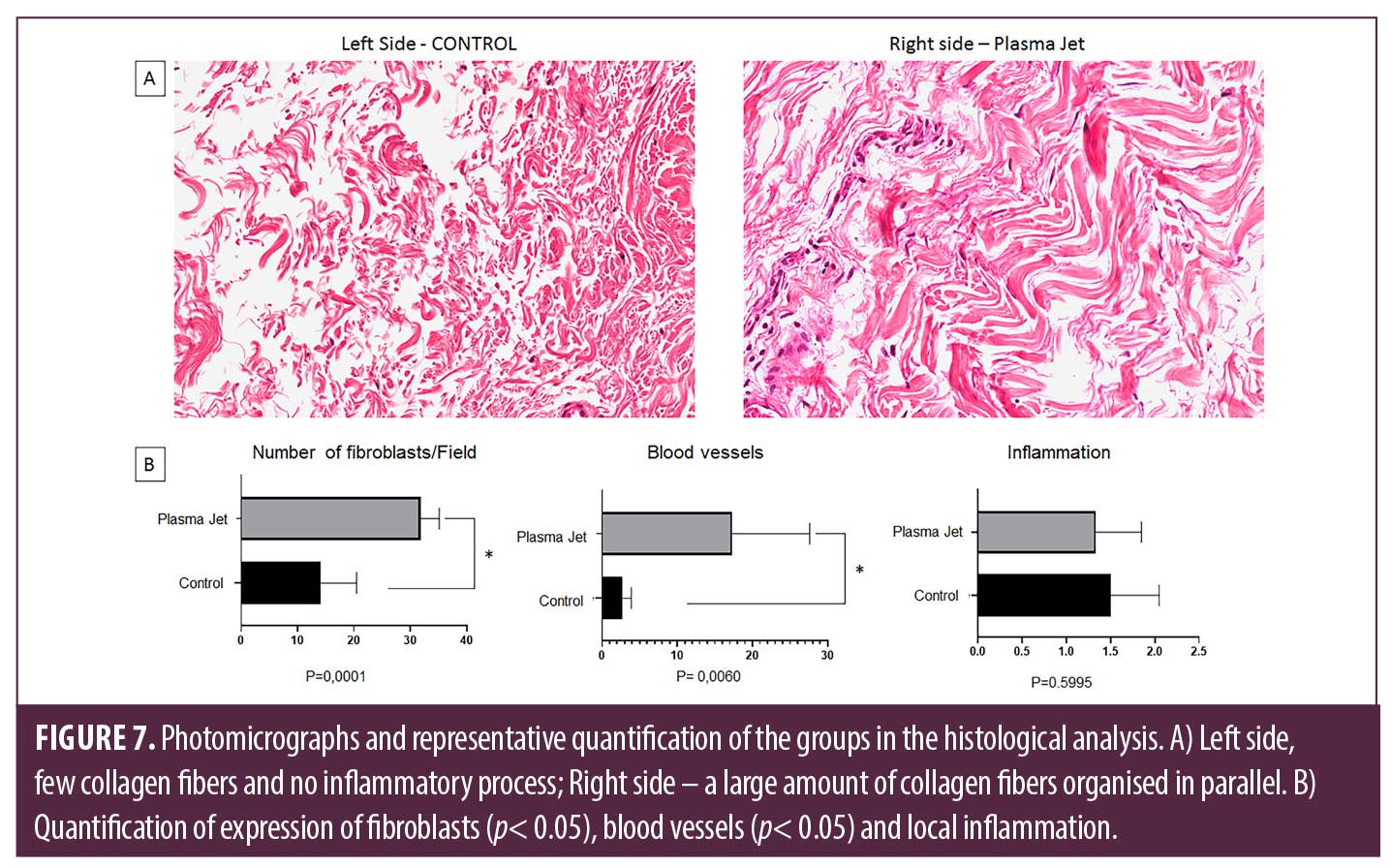
Figure 7 shows the histological analysis of the volunteer treated with direct plasma jet. The treated side has a high collagen production when compared to the control side, with the presence of thick fibers, an increase in the number of fibroblasts (p=0.0001), and a significant increase in blood vessels (p=0.006).
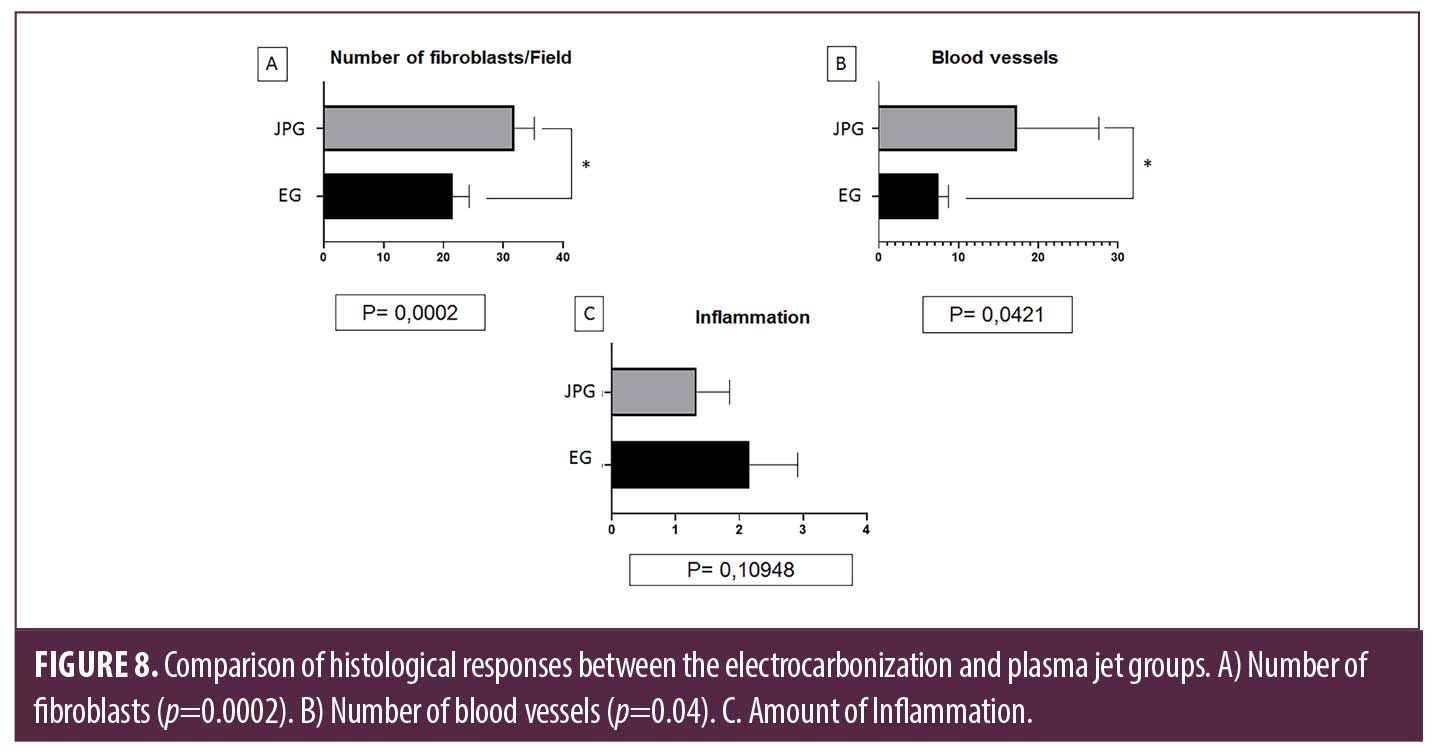
Figure 8 shows the comparison between the volunteers treated with electrocarbonization and plasma jet in the analysis of inflammation, number of fibroblasts and blood vessels. It can be observed that the plasma jet treatment showed a significant difference compared to the electrocarbonization group, such as an increase in the number of fibroblasts (p=0.002) and myofibroblasts, indicating that these cells play a crucial role during the remodelling process and formation of new collagen fibers with greater resistance and quality. There is also an increase in blood vessels (p=0.04).
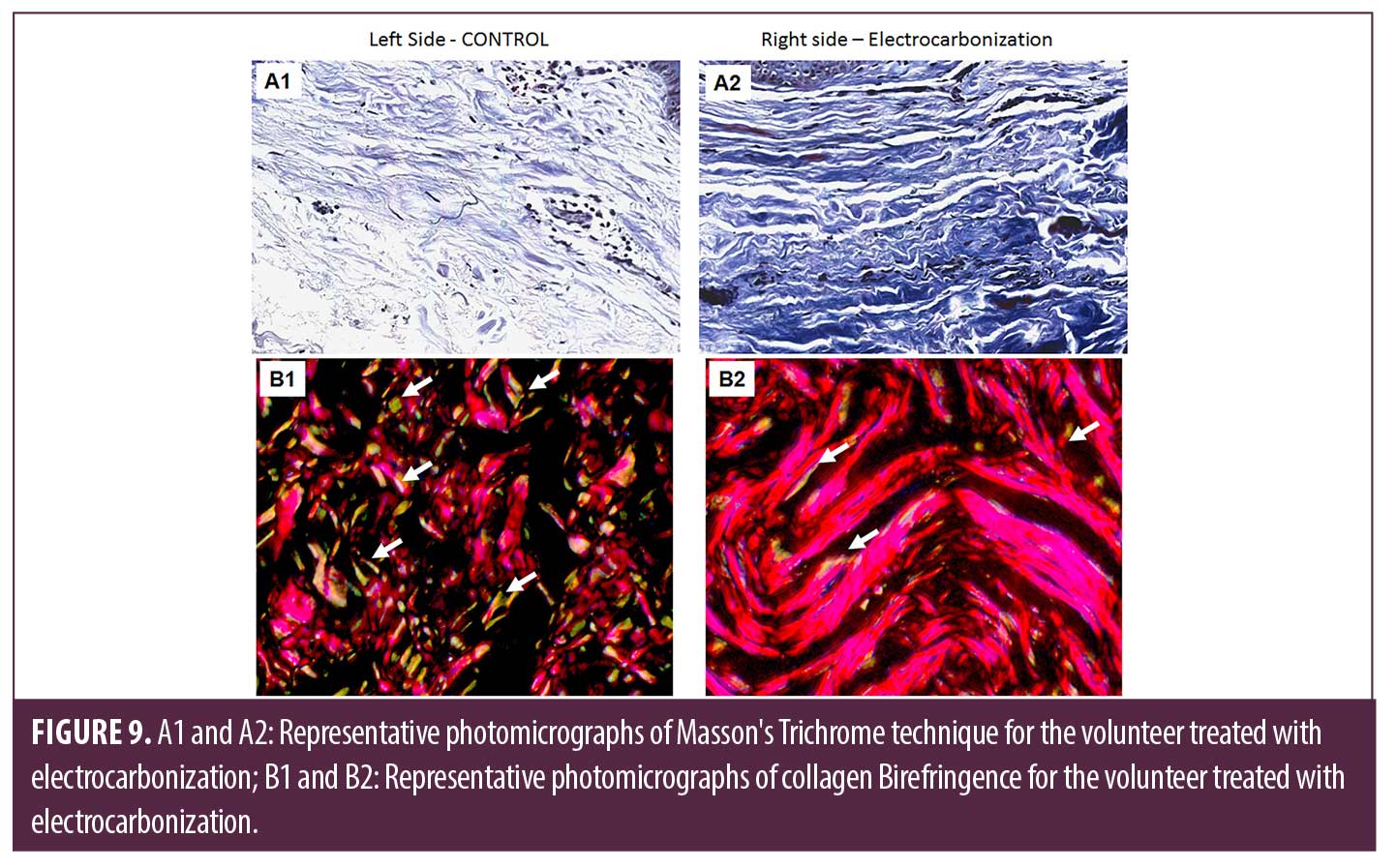
The organization and distribution of the collagen fibers can be seen in Figures 9 and 10, representing Masson’s Trichrome (A1 and A2) and Birefringence (B1 and B2) analyses. For the volunteer who received the treatment with electrocarbonization, it is possible to observe on the left side (control) poorly developed collagen fibers and slight fiber neoformation (Figure 9), in addition to a greater predominance of type III collagen (Figure 9B1). On the right side, thick collagen fibers and a significant neoformation of fibers are observed (Figure 9A2), in addition to a predominance of type I collagen (Figure 9B2).
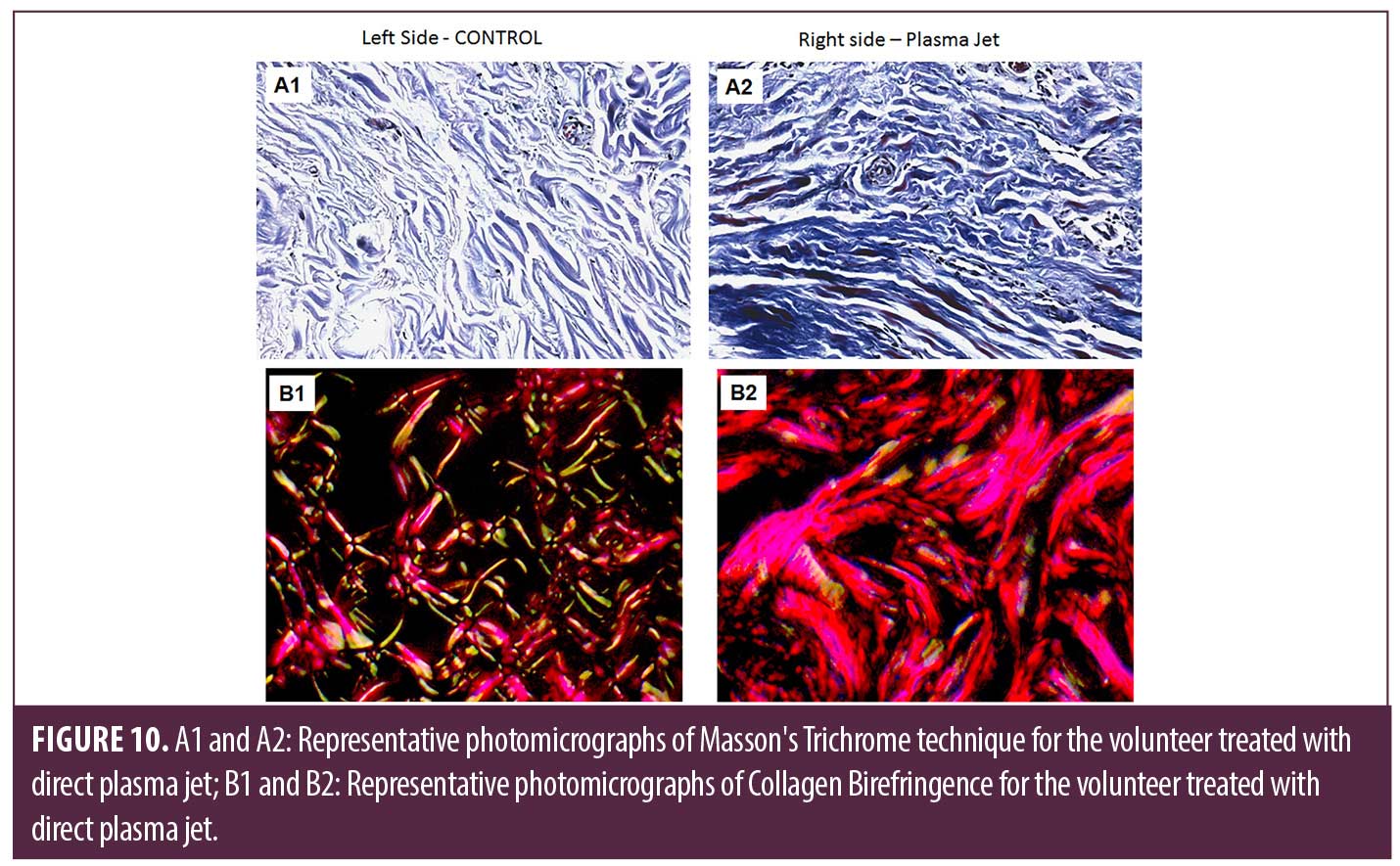
The volunteer who received the intervention with direct plasma jet presented, on the left side (control), tissue quality like that which received treatment with electrocarbonization, that is, a predominance of collagen type III (Figure 10B1) and discreet neoformation of fibers (Figure 10A1). The right side showed thick collagen fibers and an expressive fiber neoformation (Figure 10A2), also with a predominance of type I collagen (Figure 10B2).
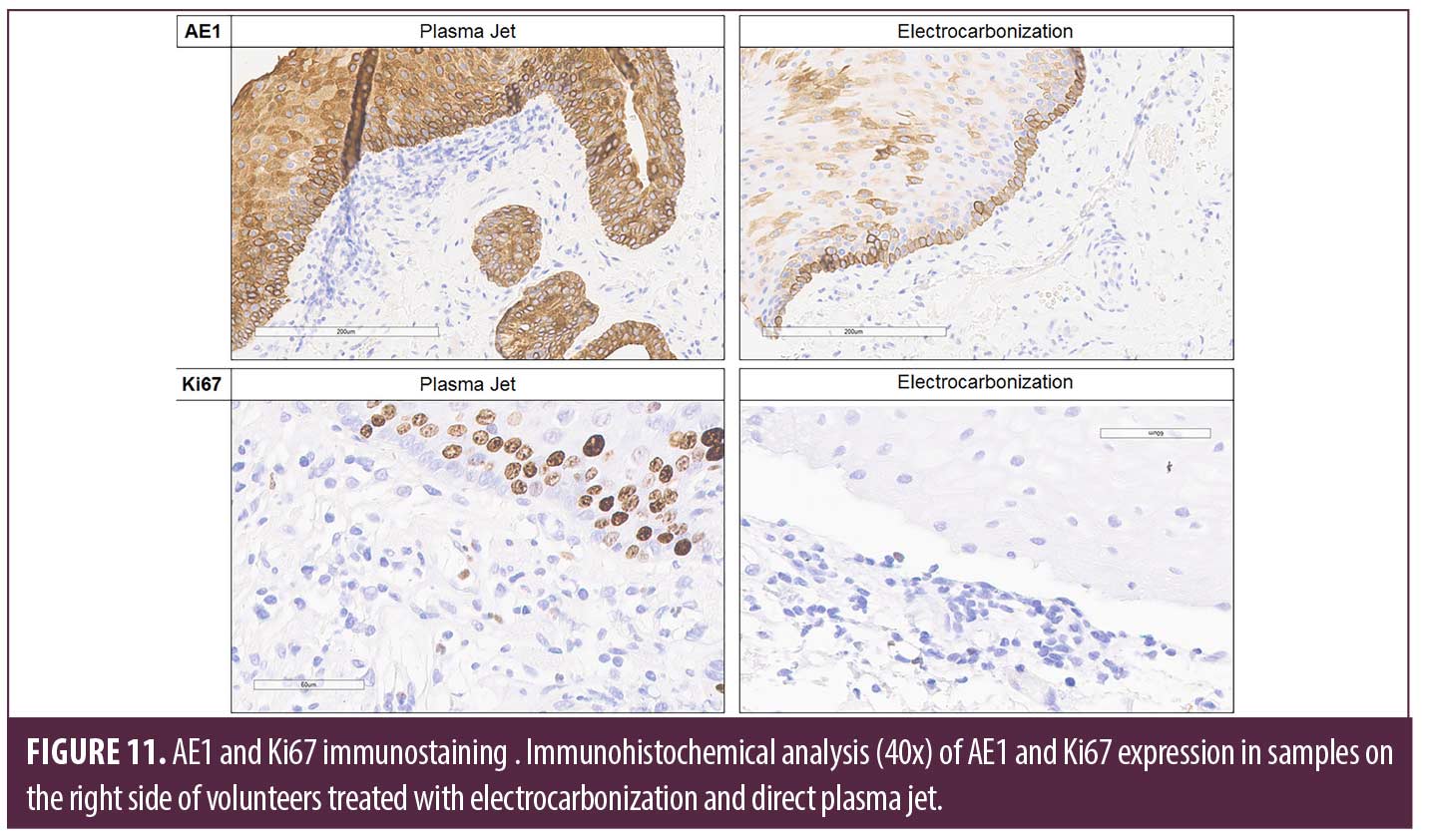
For immunoexpression of AE1 and Ki67, it was observed that the volunteer treated with plasma jet showed higher expression for both markers when compared to the volunteer who received intervention with electrocarbonization (Figure 11), demonstrating that plasma jet promotes better maintenance of the epithelial tissue and cell proliferation.
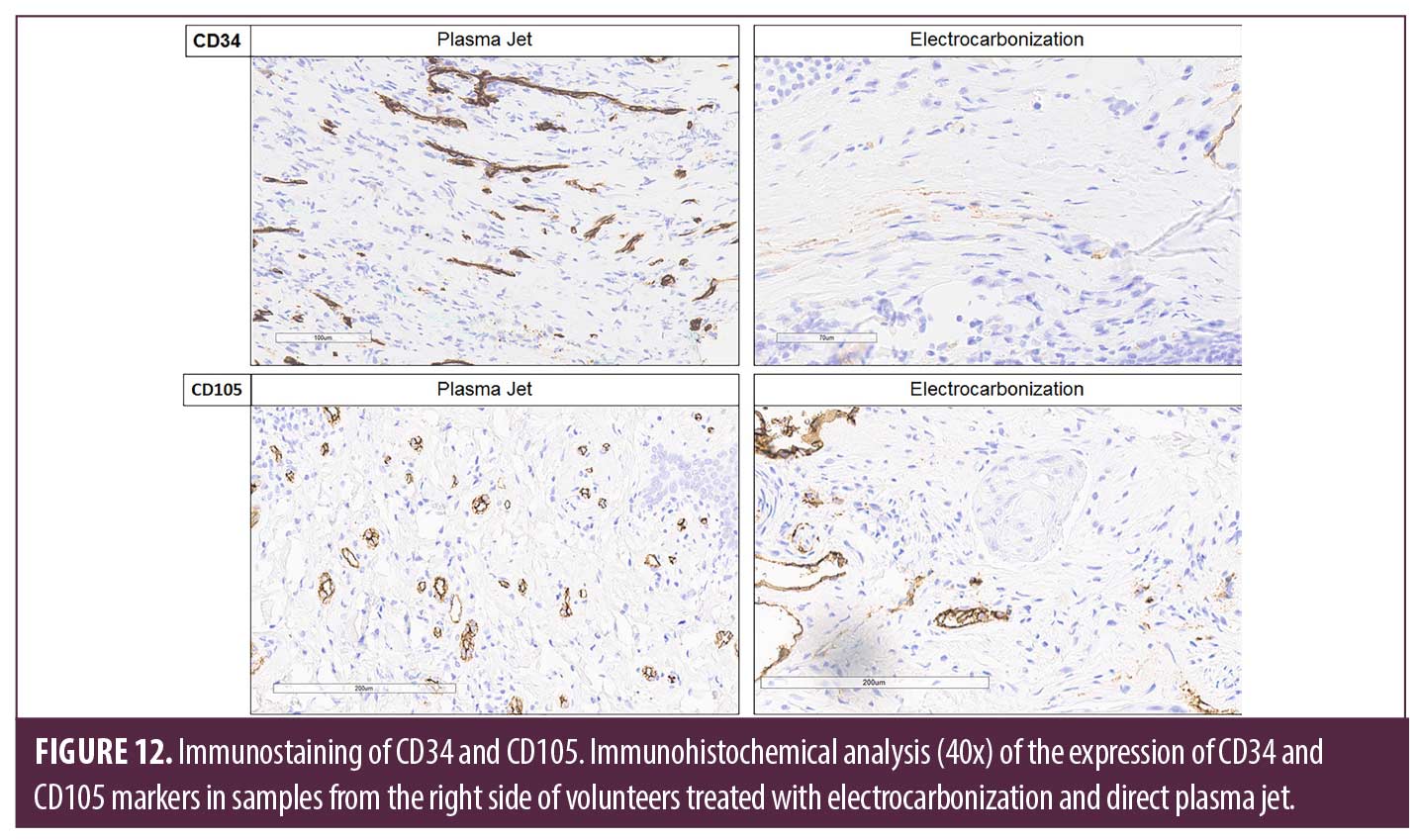
The immunoexpression of CD34 and CD105 sought to analyse the formation of new blood vessels. Thus, it was possible to observe that the plasma jet had a higher expression when compared to electrocarbonization (Figure 12), demonstrating that the plasma jet could stimulate a neoformation of vessels superior to electrocarbonization.
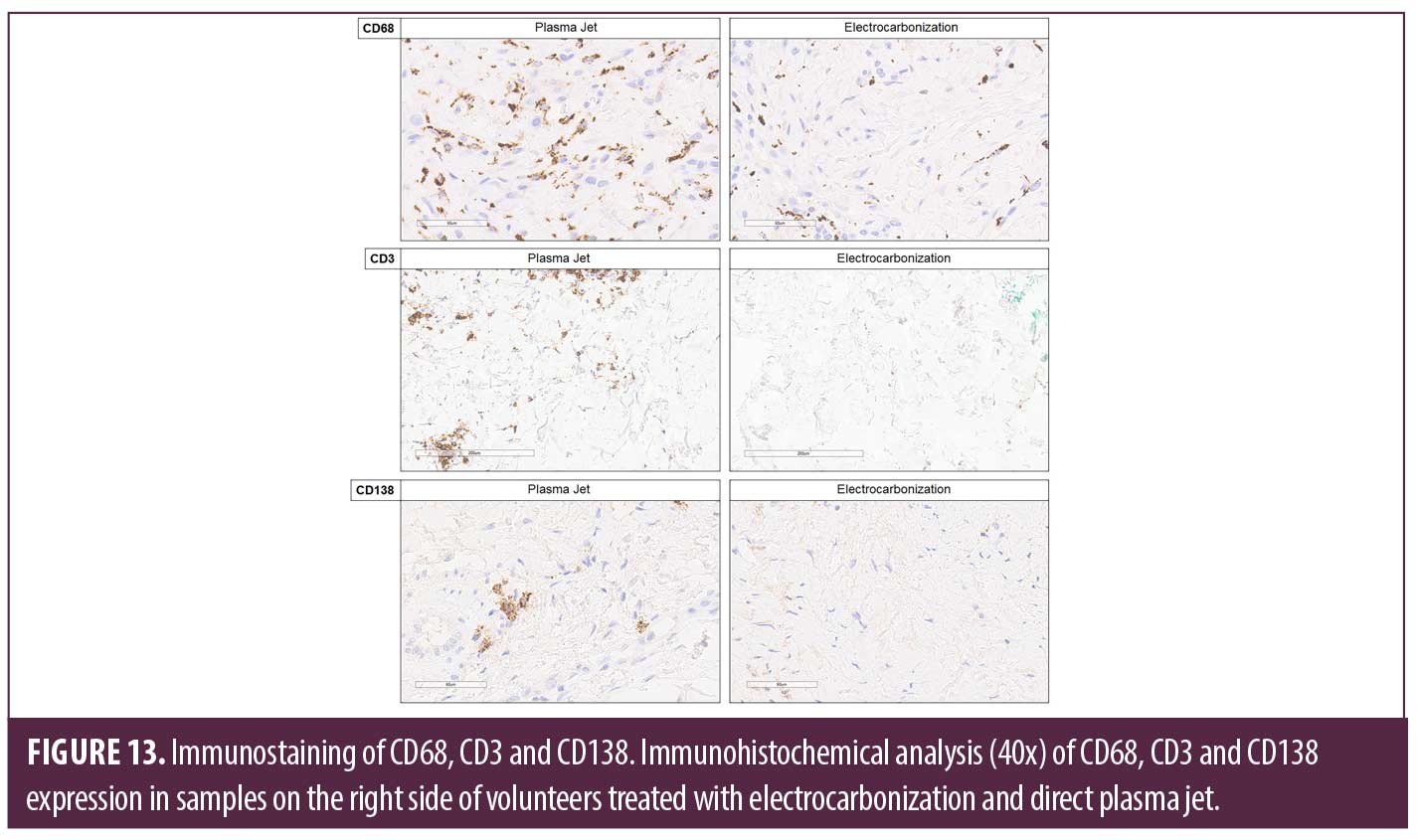
Furthermore, the immunoexpression of the inflammatory markers CD68, CD3 and CD138 was analysed. The images demonstrate that all markers were more expressive with the plasma jet treatment when compared to electrocarbonization (Figure 13), highlighting that the inflammation produced by the plasma jet was controlled.
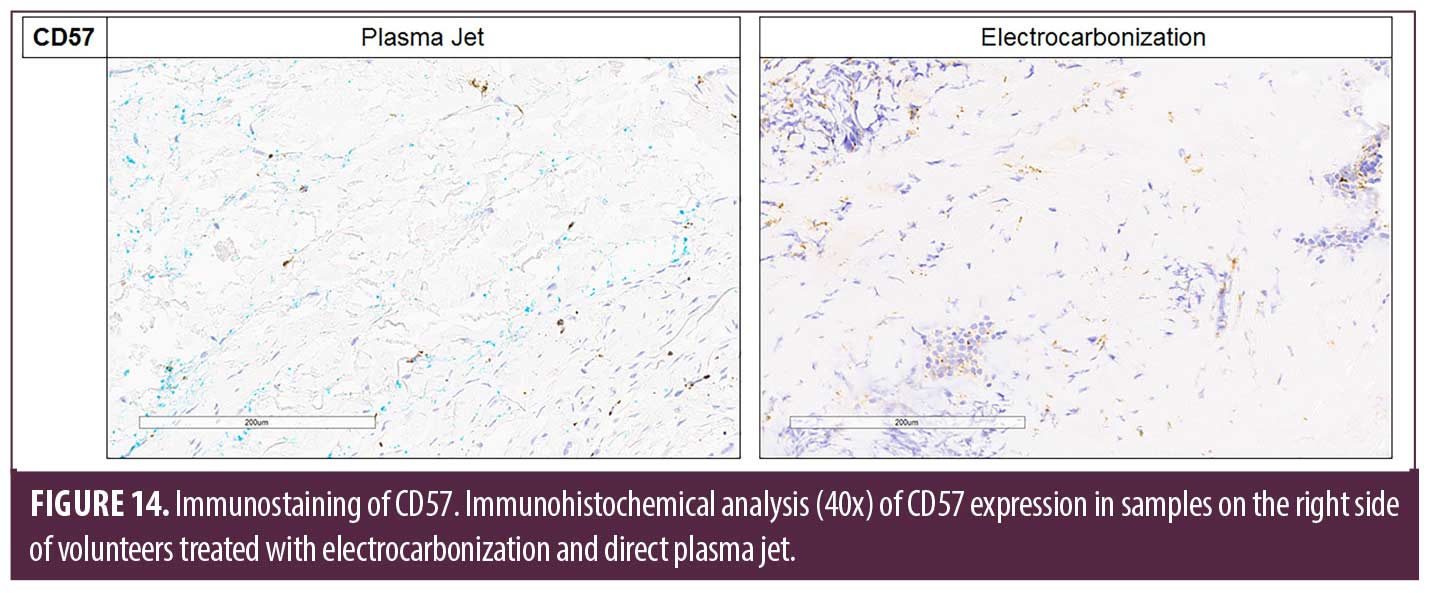
For the IHC analysis of the CD57 marker, a higher expression was identified in the volunteer who received treatment with electrocarbonization, thus highlighting that the resource was able to promote an increase in Natural Killer (NK) cells, which may be harmful to the tissue (Figure 14).
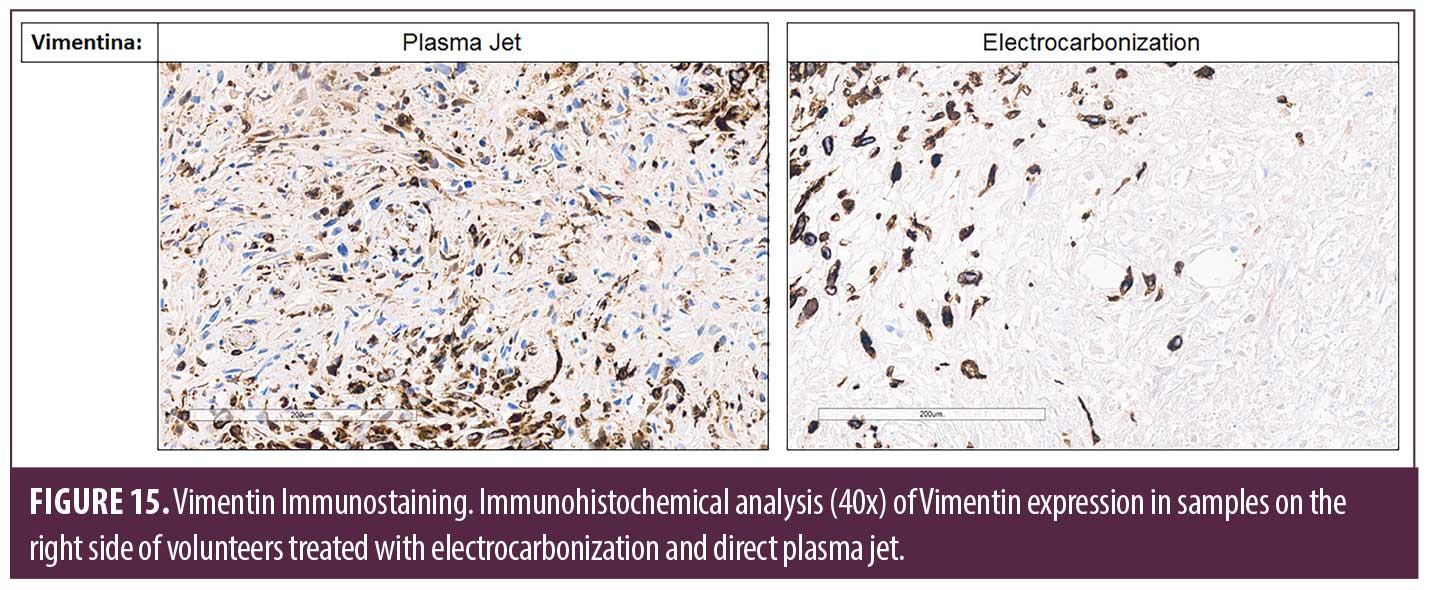
Vimentin expression (Figure 15) was performed to analyse the behavior of fibroblasts and stromal cells in the tissue. The results showed greater expression of this marker for the treatment with plasma jet, indicating a greater capacity to produce collagen fibers.
Discussion
This study aimed to analyze the effects of the direct plasma jet in comparison with electrocarbonization in the treatment of eyelid wrinkles. It can be observed that both treatments promoted a reduction of facial aging, with a decrease in the size and thickness of wrinkles, however, the morphological analyses showed better results regarding the increase in collagen production and control of the inflammatory response for the treatment with the plasma jet.
The photographic records, despite being similar for the groups, demonstrate a change in the skin tissue with rejuvenation, more pronounced in the plasma jet group. This clinical response of reducing flaccidity and wrinkles has been the alternative for several patients in clinical practice to improve this type of alteration. The use of the plasma jet proved effective for this type of response in other studies12–14 where it was applied as a possible intervention to promote skin rejuvenation and the production of collagen fibers and neovascularisation.
It can be seen that the 3D recordings allowed a more detailed analysis of the wrinkle images. A reduction in the size of wrinkles, depth and extension can also be seen, more pronounced in the plasma jet group. We observed that the region close to the eyes and eyelids showed a reduction in flaccidity and ptosis in the region of the eyes. The plasma jet promotes an increase in the skin regeneration process because when applied to the face, it can activate fibroblasts and produce new collagen and elastin fibers. This association of physiological responses allows an improvement in the clinical appearance of wrinkles, favouring an efficient result.15
In the histological analysis, it can be observed that the application of electrocarbonization promoted an increase in the production of bulky collagen fibers, neoformation of fibers, an increase in the number of fibroblasts, in the number of blood vessels and in the amount of inflammation. In the plasma jet group, similarly, there was a high production of collagen, thick fibers, and an increase in the number of fibroblasts, and blood vessels, with a controlled inflammatory response. Although both groups presented favorable results for the treatment of wrinkles, it can be observed that in the comparison between the groups, the one that received the plasma jet treatment showed a difference compared to the electrocarbonization group, with an increase in the number of fibroblasts, presence of blood vessels, with less inflammatory intensity, increased vascularity, which indicates a greater ability to grow and consequently a quick response to the formation of newly formed collagen fibers.15
Furthermore, it is noteworthy that the IHC analyses showed an important difference in the formation of new blood vessels between the two interventions. The immunoexpression of CD105 and CD34 markers was superior for the plasma jet treatment, demonstrating the neovascularisation capacity for the resource. These results corroborate the literature that discusses the formation of new vessels and tissue reorganisation, especially on wrinkles, with plasma jet treatment.15,16
It is also suggested that thermal modification of the papillary dermis is necessary to induce dermal collagen remodelling and neocollagenesis, which is a necessary response to sustain improvement in deep wrinkles.14,15,17,18 Our study corroborates this discussion since the histological findings demonstrate greater proliferation and organisation of collagen, especially in the treatment with the plasma jet, in addition, the immunoexpression of Vimentin increased for this resource proved to be superior to electrocarbonization, confirming the ability to stimulate a greater proliferation of fibroblasts with the plasma jet.
The literature shows that applying the plasma jet promotes stimulation of the immune system, activating inflammatory mediators and tissue regeneration. This activation promotes modulation of the tissue that received the application, favoring skin revitalisation.19–21 Through the analysis of the IHC of the present study, it was possible to observe that the plasma jet, when compared to the electrocarbonization, presented a greater capacity for stimulation and modulation of the immunological activity since the results of the IHC for the immunological markers CD3 and CD68 were superior for the plasma jet. In contrast, the CD57 marker was more expressive in the treatment with electrocarbonization. These results suggest that electrocarbonization promoted an increase in NK cells in the tissue, a marker that signals repair difficulties. These evaluations also found that the plasma jet stimulated the activity of T-lymphocytes and macrophages to control inflammation.
Immunohistochemical and clinical response superior to the group that received the application of electrocarbonization. It is suggested that this positive response from the plasma jet can be explained by immunohistochemical, and histological modulation generated by heating the most superficial layer of the skin, inducing injury and local regeneration. The influence of reactive species released on these applied parameters (nitrogen and isotopes of nitrogen OH, NO and oxygen) is also suspected, which in contact with air humidity produces ozone and helps tissue recovery. All nitrogen isotopes are potential collagen formers present only in plasma jet emission.5,21,22.
Limitations of this study include the absence of a follow-up analysis and the limitation of clinical methods for assessing flaccidity. In addition, it is a pilot study and a new study with a larger number is indicated of participants mainly for the morphological evaluations. It is suggested that new studies should be carried out with other parameters and a follow-up analysis.
Conclusion
Based on the data presented, it can be concluded that despite the two techniques showing benefits in the treatment of eyelid wrinkles, the direct plasma jet showed superior benefits at the tissue level, confirmed by histological and IHC analysis, when comparing electrocarbonization. In addition, the satisfaction and adverse effects reported in the techniques suggest that electrocarbonization presents greater discomfort compared to direct plasma jet.
References
- Fitzgerald R, Graivier MH, Kane M, et al. Atualização em envelhecimento facial. Aesthet Surg J. 2010 Jul-Ago;30 Supl:11S–24S.
- Ko AC, Korn BS, Kikkawa DO. O rosto envelhecido. Surv Oftalmol. 2017 Mar-Abr;62(2):190–202.
- Swift A, Liew S, Weinkle S, et al. The Facial Aging Process From the “Inside Out”. Aesthet Surg J. 2021 Sep 14;41(10):1107–1119.
- Steffen Emmert et al. Atmospheric pressure plasma in dermatology: Ulcus treatment and much more. Clinical Plasma Medicine, Volume 1, Issue 1, 2013, Pages 24-29, ISSN 2212-8166.
- Bernhardt T, Semmler ML, Schäfer M, et al. Plasma Medicine: Applications of Cold Atmospheric Pressure Plasma in Dermatology. Oxid Med Cell Longev. 3 de setembro de 2019;2019:3873928.
- Nishioka M. Eletrocautério e Jato de Plasma. In: Renno ACM, Martignago C, editores. MANUAL PRÁTICO DE COSMETOLOGIA E ESTÉTICA. 1. ed. São Paulo: Manole; 2022. p. 203–224
- Wende K, Williams P, Dalluge J, et al. Identification of the biologically active liquid chemistry induced by a nonthermal atmospheric pressure plasma jet, Biointerphases.10(2015)1–16.
- Guerra ARO, Carreiro EDM, Borges FDS, Vasconcellos LSD, et al. Characterization of plasma jet equipment used in the treatment of aesthetic affections. Int. J. of Adv. Res. 6 (Dec). 595–604.
- Micussi MTA, Oliveira TCM, Meyer PF,et al. Protocolo de avaliação facial: uma proposta fisioterápica Revista Fisioterapia Brasil, Suplemento Especial. 2008.
- Segot-Chicq E, Compan-Zaouati D, Wolkenstein P, Consoli S,et al. Development and validation of a questionnaire to evaluate how a cosmetic product for oily skin is able to improve well‐being in women. Journal of the European Academy of Dermatology and Venereology. 2007 Oct;21(9):1181–1186.
- Narins RS, Brandt F, Leyden J, et al. A randomised, double‐blind, multicenter comparison of the efficacy and tolerability of Restylane versus Zyplast for the correction of nasolabial folds. Dermatologic surgery. 2003 Jun;29(6):588–595.
- Shimizu K, Hayashida K, Blajan M. Novel method to improve transdermal drug delivery by atmospheric microplasma irradiation. Biointerphases. 2015 Jun 6;10(2):029517.
- Graves D, Hamaguchi S, O’Connell D. In Focus: Plasma Medicine. Biointerphases. 2015 Jun 25;10(2):029301.
- Foster KW, Moy RL, Fincher EF. Advances in plasma skin regeneration. J Cosmet Dermatol. 2008 Sep;7(3):169–179.
- Bogle MA, Arndt KA, Dover JS. Evaluation of plasma skin regeneration technology in low-energy full-facial rejuvenation. Arch Dermatol. 2007 Feb;143(2):168–174.
- Kilmer S, Semchyshyn N, Shah G, et al. A pilot study on the use of a plasma skin regeneration device (Portrait PSR3) in full facial rejuvenation procedures. Lasers Med Sci. 2007 Jun;22(2):101–109.
- Holcomb JD, Kent KJ, Rousso DE. Nitrogen plasma skin regeneration and aesthetic facial surgery: multicenter evaluation of concurrent treatment. Arch Facial Plast Surg. 2009 May-Jun;11(3):184–193.
- Elsaie ML, Kammer JN. Evaluation of plasma skin regeneration technology for cutaneous remodeling. J Cosmet Dermatol. 2008 Dec;7(4):309–311.
- Potter MJ, Harrison R, Ramsden A, et al. Facial acne and fine lines: transforming patient outcomes with plasma skin regeneration. Ann Plast Surg. 2007 Jun;58(6):608–613.
- Holcomb JD, Kelly M, Hamilton TK, et al. A Prospective Study Evaluating the Use of Helium Plasma for Dermal Resurfacing. Lasers Surg Med. 2020 Dec;52(10):940–951.
- Theppornpitak N, Udompataikul M, Chalermchai T, et al. Nitrogen plasma skin regeneration for the treatment of mild-to-moderate periorbital wrinkles: A prospective, randomized, controlled evaluator-blinded trial. J Cosmet Dermatol. 2019 Feb;18(1):163–168.
- Fitzpatrick R, Bernstein E, Iyer S, Brown D, et al. A histopathologic evaluation of the Plasma Skin Regeneration System (PSR) versus a standard carbon dioxide resurfacing laser in an animal model. Lasers Surg Med. 2008 Feb;40(2):93–99.