J Clin Aesthet Dermatol. 2023;16(12):52–54.
J Clin Aesthet Dermatol. 2023;16(12):52–54.
by Danielle Yee, MD;* Kathryn Lee, BA;* Margaret Y. Huang, BS; Paige Kingston, BS; Edwin Korouri, BS; Hannah Peterson, BS; and April W. Armstrong, MD, MPH
Dr. Yee, Dr. Armstrong, Ms. Huang and Ms. Kingston are with the Division of Dermatology, University of California in Los Angeles, Los Angeles, California. Ms. Lee is with Saint Louis University School of Medicine in Saint Louis, Missouri. Mr. Korouri is with Chicago Medical School in North Chicago, Illinois. Ms. Peterson is with Loma Linda University School of Medicine in Loma Linda, California. *Dr. Yee and Ms. Lee share co-first authorship of this article.
FUNDING: No funding was provided for this article.
DISCLOSURES: Dr. Armstrong has served as a research investigator, scientific advisor, and/or speaker to AbbVie, Almirall, Arcutis, ASLAN, Beiersdorf, BI, BMS, EPI, Incyte, Leo, UCB, Janssen, Eli Lilly, Mindera, Nimbus, Novartis, Ortho Dermatologics, Sun Pharmaceutical Industries, Dermavant, Dermira, Sanofi, Regeneron, and Pfizer. All other authors have no conflicts of interest relevant to the content of this article.
Keywords: Psoriasis, skin of color, online patient health information, patient education
Psoriasis is a chronic inflammatory skin disease with considerable physical and quality of life burden that affects approximately eight million adults in the United States (US).1 Reported psoriasis prevalence in skin of color (SOC) populations is lower than in White populations, and treatment disparities exist among patients of different races.1,2 Black patients with psoriasis have been found to be less familiar with biologic therapies and are less likely to receive these treatments, compared to White patients.2,3 The level of quality, readability, and comprehensiveness regarding online educational materials focused on SOC patients with psoriasis is unknown. Given that 80 percent of internet users report searching online for health information,4 our study aimed to evaluate the quality, comprehensiveness, and readability of the top-searched websites for patient information about psoriasis in SOC.
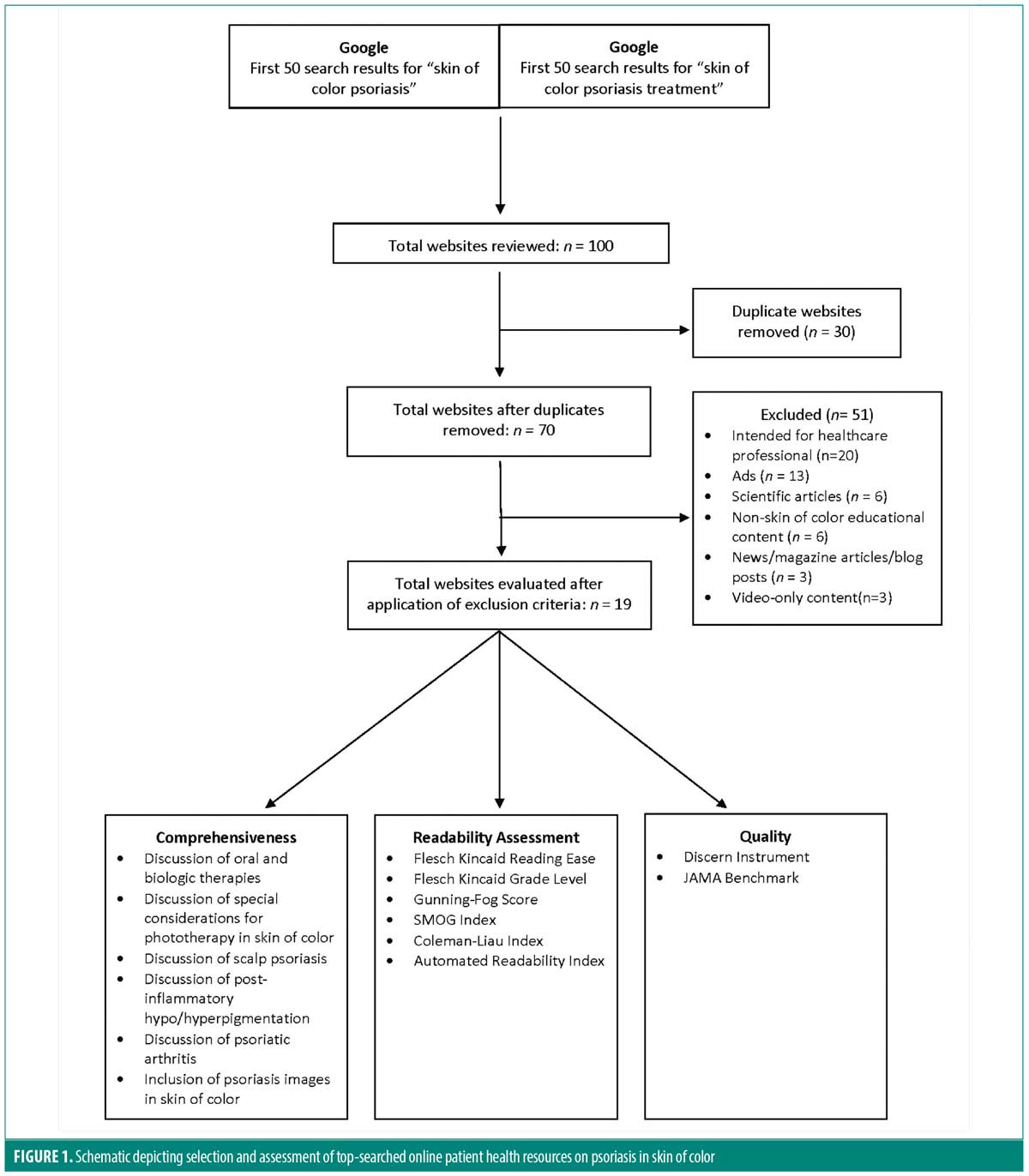
An internet search for the terms “skin of color psoriasis” and “skin of color psoriasis treatment” was performed using Google in October 2022. We evaluated the first 50 search results for each search term (Figure 1). Inclusion criteria included reference to psoriasis, reference to SOC, and patients as the primary intended audience. Text was extracted from each website and run through six validated readability assessment tools: Flesch-Kincaid Reading Ease, Flesch-Kincaid Grade Level, Gunning-Fog Score, SMOG Index, Coleman-Liau Index, and Automated Readability Index. These indices employ different formulas to analyze variables, such as sentence length, syllables per word, and letters per word. Website quality was assessed using Journal of the American Medical Association (JAMA) Benchmark criteria and the DISCERN Instrument. For the DISCERN score, two reviewers independently graded webpages. Scores within one point were averaged; discrepancies greater than two points were discussed to consensus.
Our analysis included a total of 19 websites. The American Medical Association (AMA) recommends patient reading materials be written at a sixth-grade reading level or lower. The average grade level for readability across all webpages was the twelfth-grade level (12.0, range: 8.7–14.7). All sources were found to be above the recommended reading level. Average readability scores are presented in Table 1.
Quality of the websites was variable. The average modified DISCERN score was 47 out of 80, which is categorized as fair (range: 27–64). The average JAMA Benchmark score was 2.3 out of 4 (range: 0–4, where 4 signifies higher quality). Most sources provided a publication/modification date (78.9%), provided references (63.2%), and identified an author (73.7%). Two websites listed disclosures. The majority of sources discussed postinflammatory hypo-/hyperpigmentation (73.7%, 14/19), oral and biologic therapies (63.2%, 12/19), and scalp psoriasis (57.9%, 11/19). Nearly half of the websites discussed special consideration of phototherapy in SOC patients, and 26.3 percent discussed psoriatic arthritis. Around 30 percent of the online resources included images of psoriasis in SOC.
Given the accessibility of online health information, dermatologists should be aware of psoriasis-related online health resources to foster patient education and reduce treatment disparities among all patients. The average DISCERN score for top-searched websites discussing psoriasis in SOC was classified as fair. Additionally, the average reading level for these resources was the twelfth-grade level, which is six grade levels above the recommended reading level. This might prevent patients from understanding accessible information related to psoriasis symptoms and treatments.
It is important to note that the examined benchmarks represent only one method of assessing the quality of online websites available to patients. Other factors, such as reader engagement, must also be considered. Patients might understand an engaging website more than a non-engaging website despite the lack of certain details, such as disclosures, publication dates, and reference citations. Dermatologists should strive to create readable, high-quality, and engaging online health resources for patients of all races to facilitate shared decision-making practices.
References
- Armstrong AW, Mehta MD, Schupp CW, et al. Psoriasis prevalence in adults in the United States. JAMA Dermatol. 2021;157(8):940–946.
- Takeshita J, Gelfand JM, Li P, et al. Psoriasis in the US Medicare population: prevalence, treatment, and factors associated with biologic use. J Invest Dermatol. 2015;135(12):2955–2963.
- Takeshita J, Eriksen WT, Raziano VT, et al. Racial differences in perceptions of psoriasis therapies: implications for racial disparities in psoriasis treatment. J Invest Dermatol. 2019;139(8):1672–1679.e1.
- Fox S. The social life of health information. Pew Research Center. 12 May 2011. https://www.pewresearch.org/internet/wp-content/uploads/sites/9/media/Files/Reports/2011/PIP_Social_Life_of_Health_Info.pdf. Accessed 12 Feb 2023.