by Komal A. Paradkar, BS, and Alisha N. Plotner, MD
by Komal A. Paradkar, BS, and Alisha N. Plotner, MD
Ms. Paradkar is with The Ohio State University College of Medicine in Columbus, Ohio. Dr. Plotner is with Division of Dermatology, The Ohio State University in Columbus, Ohio.
J Clin Aesthet Dermatol. 2023;16(12):55–56.
ABSTRACT: Keratoacanthoma (KA) is an epidermal cell tumor with a central keratin plug known to be a variant of keratinocyte carcinoma (KC). KAs typically arise from ultraviolet (UV)-damaged skin and thus are particularly prevalent on extremities. KAs can also be a consequence of local skin trauma. 5-fluorouracil (5-FU) is a topical therapy used to treat early KC, as well as actinic keratoses (AKs). In this paper, we describe the unique cases of two elderly female patients who were treated with 5-FU for AKs of the lower extremities but developed severe inflammatory reactions and reactive KAs to the topical therapy. Keywords: Keratoacanthoma, reactive keratoacanthoma, keratinocyte carcinoma, 5-fluorouracil
FUNDING: No funding was provided for this article.
DISCLOSURES: The authors report no conflicts of interest relevant to the content of this article.
Keratoacanthoma (KA) is an epidermal tumor with a central keratin plug known for initial rapid growth with a potential for spontaneous resolution.1 KAs are a variant of keratinocyte carcinoma (KC), but they typically lack the ability to metastasize.1,2 They classically arise from photodamaged skin, often within an area of field cancerization, but may develop as a reaction to local cutaneous trauma as well.1 Sun-exposed areas, particularly the lower legs of elderly adults, are a site of common predilection.3 5-fluorouracil (5-FU) is a topical chemotherapeutic used for actinic keratosis (AK) and early KC. Treatment with 5-FU causes an inflammatory reaction that may be severe. Herein, we describe two patients treated with 5-FU for AKs on the lower legs who developed severe inflammatory reactions and reactive KAs.
Case 1
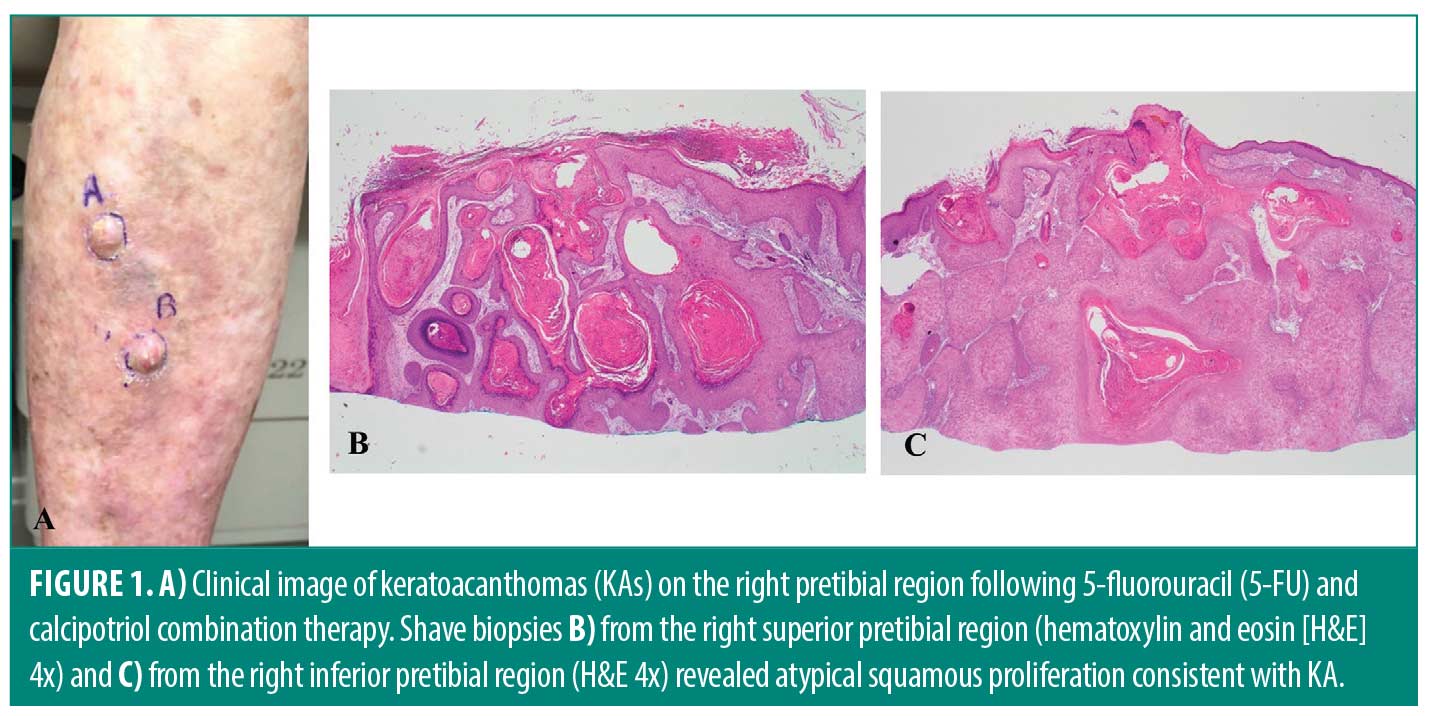
A 71-year-old White female patient with a history of KC and melanoma presented with diffuse AKs on her lower legs. She was treated with a compounded 5-FU and calcipotriol cream twice daily for four weeks. She had a vigorous inflammatory reaction, characterized by pain, swelling, intense erythema, and focal erosions. As her legs were healing, she noticed the abrupt onset of two rapidly enlarging painful nodules on her right shin (Figure 1A). Biopsies taken six weeks post-discontinuation of treatment revealed KAs (Figures 1B–C), and both were successfully treated with Mohs micrographic surgery.
Case 2
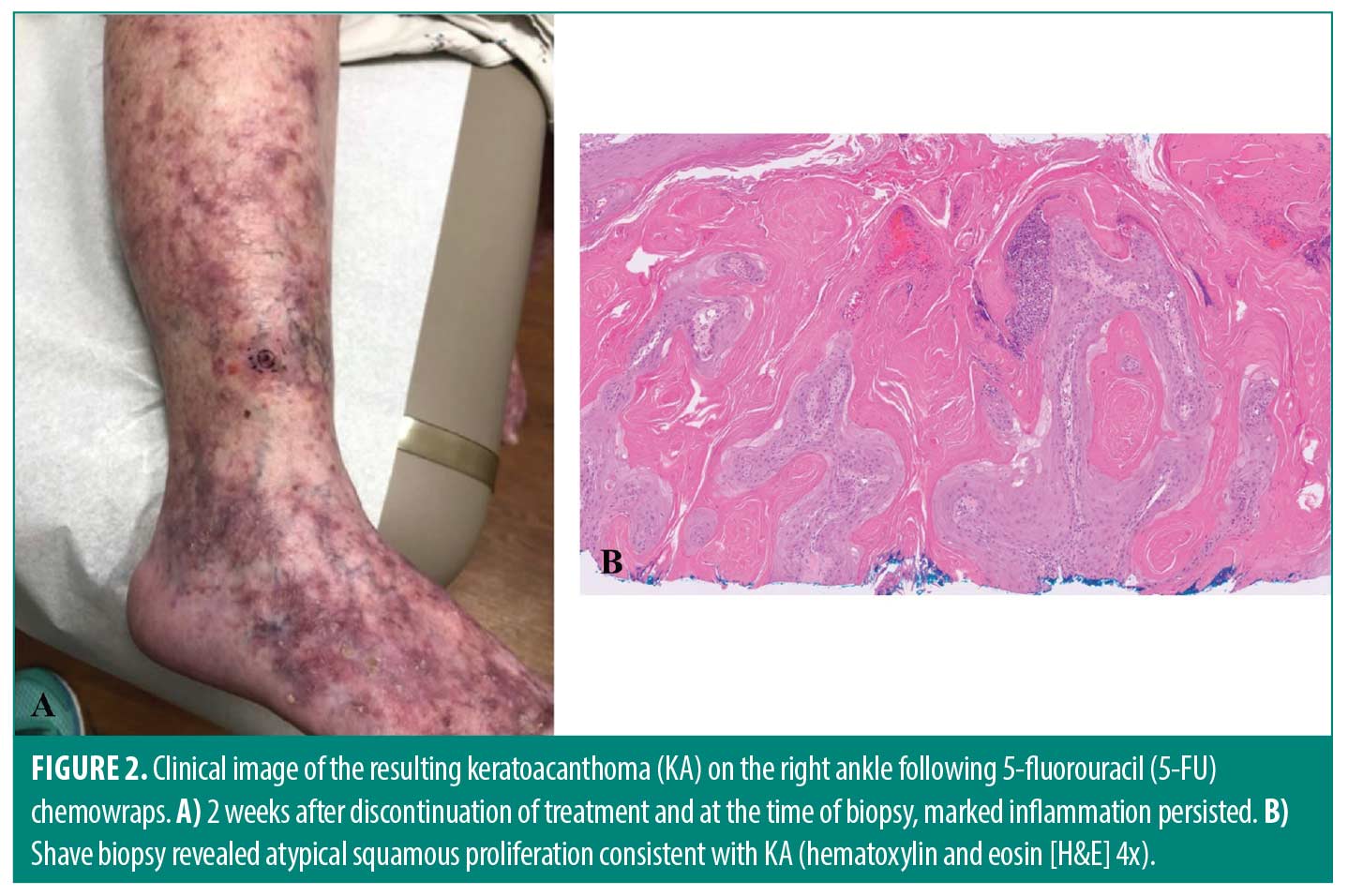
A 70-year-old White female patient with diffuse AKs on her lower legs was treated with 5-FU chemowraps (5-FU applied under an Unna boot, changed weekly) for four weeks. At her last visit, a painful and intense inflammatory response was noted, and she declined additional treatment. She also noted development of a new painful papulonodule on her right ankle (Figure 2A). This was initially treated with clobetasol ointment for two weeks without resolution. A follow-up biopsy revealed KA (Figure 2B), and she was successfully treated with Mohs micrographic surgery.
Discussion and Conclusion
Reactive KAs have been described after accidental or surgical trauma, but these two cases are particularly notable, as the KAs developed toward the end of the 5-FU treatment course. Topical 5-FU is used to treat AKs and early KCs and has even been studied for KAs; in one series of nine patients with KA treated with topical 5-FU, all patients had complete KA resolution.2 Given these findings, it is unexpected for a KA to develop during the 5-FU treatment course. Furthermore, the development of these reactive KAs can be both perplexing and frustrating for the patient undergoing 5-FU treatment to reduce AKs and/or early KCs, often with the goal of avoiding future surgical treatment.
5-FU is expected to cause an inflammatory reaction during the treatment course, characterized by redness, crusting, and tenderness. 5-FU in combination with calcipotriol is superior in reducing the long-term risk of squamous cell carcinoma over 5-FU alone.4 Applying 5-FU in combination with an Unna wrap enhances tolerability of the treatment and allows for treatment of a larger area of skin.5 To the authors’ knowledge, there have not been previous reports of KAs resulting from 5-FU treatment, and the exact mechanism of KA development in these two patients is unknown. In patients with KA secondary to surgical trauma, the presence of cytokines and genetic mutations may stimulate KA growth.6 In our patients, the combination treatments might have caused a severe enough inflammatory and cutaneous wounding response to induce the development of KAs in an area of high predilection. Regardless of the exact etiology, patients undergoing 5-FU treatment on the lower legs should be counseled about this risk.
References
- Kwiek B, Schwartz RA. Keratoacanthoma (KA): an update and review. J Am Acad Dermatol. 2016;74(6):1220–1233.
- Thompson BJ, Ravits M, Silvers DN. Clinical efficacy of short contact topical 5-fluorouracil in the treatment of keratoacanthomas: a retrospective analysis. J Clin Aesthet Dermatol. 2014;7(11):35–37.
- Ko CJ, Glusac EJ, McNiff JM, et al. Squamous proliferations on the legs of women: qualitative examination of histopathology, TP53 sequencing, and implications for diagnosis in a series of 30 cases. J Am Acad Dermatol. 2017;77(6):1126–1132.e1.
- Rosenberg AR, Tabacchi M, Ngo KH, et al. Skin cancer precursor immunotherapy for squamous cell carcinoma prevention. JCI Insight. 2019;4(6):e125476.
- Peuvrel L, Saint-Jean M, Quereux G, et al. 5-fluorouracil chemowraps for the treatment of multiple actinic keratoses. Eur J Dermatol. 2017;27(6):635–640.
- Goldberg LH, Silapunt S, Beyrau KK, et al. Keratoacanthoma as a postoperative complication of skin cancer excision. J Am Acad Dermatol. 2004;50(5):753–758.