J Clin Aesthet Dermatol. 2019;12(1):32–34
 by Verónica Olvera-Cortés, MD, and Nancy Pulido-Díaz, MD
by Verónica Olvera-Cortés, MD, and Nancy Pulido-Díaz, MD
Drs. Olvera-Cortés and Pulido-Díaz are with the Dermatology Department at the Mexican Institute of Social Security and National Medical Center La Raza in Mexico City, Mexico.
Funding: No funding was received for this study.
Disclosures: The authors have no conflicts of interest relevant to the content of this article.
Abstract: Morbihan’s disease is characterized by the presence of chronic and persistent edema of the periorbital tissue, forehead, glabella, nose, and cheeks. In some cases, it is related to acne and rosacea, but its exact etiology remains unknown. A defined therapeutic approach has yet to be established for the treatment of Morbihan’s disease. To date, the systemic and surgical options attempted have not been very successful and/or do not yield sustained results. Isotretinoin is a key systemic treatment used for the treatment of various skin conditions. However, there are few reports of isotretinoin being used to treat Morbihan’s disease. Here, we present the details of three patients with Morbihan’s disease who were successfully treated long-term with isotretinoin.
Keywords: Chronic persistent edema, Morbihan’s disease, isotretinoin
Morbihan’s disease was first reported by Degos,1 who described the condition as a chronic and persistent erythema and edema that mainly affects periorbital tissue, but can also affect the forehead, glabella, nose, and cheeks.1 When the eyelids are affected, facial disfiguration can be so severe that patients can present with a narrowing of the visual field.2 Morbihan’s disease has previously been associated with acne and rosacea, but its exact etiology remains unknown and there are no specific laboratory or histologic findings that shed light on the condition. Treatment options are limited and not very successful. Here, we present the details of three patients successfully treated with high-dose, long-term isotretinoin. Photoconsent was received from the patients.
Case Presentations
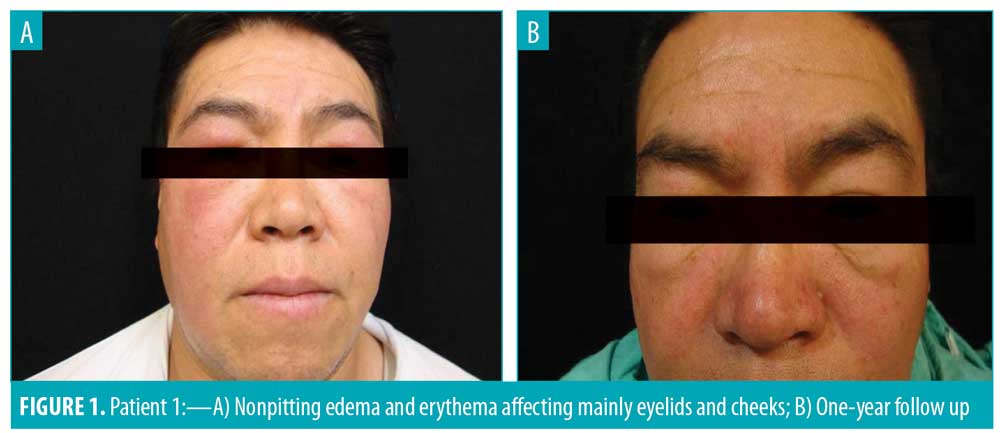
Case 1. A 51-year-old patient presented with a three-year history of edema and erythema affecting the eyelids and cheeks. On examination, a nonpitting edema and erythema was found on both eyelids and the cheeks (Figure 1A). Skin biopsy reported a granulomatous blepharitis. Periodic acid–Schiff (PAS) and Ziehl–Neelsen stains were negative. Initial management was done with isotretinoin 20mg daily and thalidomide 100mg daily for five months, with eventual suspension of thalidomide because of adverse effects. The edema and erythema persisted and isotretinoin was increased to 40mg daily for one year, resulting in an almost complete recovery. Follow-up was continued for one year with no recurrence (Figure 1B).
Case 2. A 62-year-old patient with a one-year history of edema and erythema affecting the periocular region, cheeks, and nasal dorsum presented with exacerbation after use of topical betamethasone, clotrimazole, and gentamicin. On examination, a nonpitting edema and erythema were found on the cheeks and nasal dorsum.
Skin biopsy reported superficial perivascular dermatitis, dermal edema, and chronic lymphoplasmocitic perifolliculitis. Treatment was initiated with 40mg of isotretinoin daily for one year with good response. Posterior adjustment to 20mg of isotretinoin daily was made and maintained for another year, leading to complete remission. Follow-up was continued for three years without relapse.
Case 3. A 29-year-old patient with a four-year history of edema and erythema of the centrofacial region with madarosis presented. On examination, nonpitting edema and erythema was observed on the forehead, eyelids, cheeks, and nasal dorsum (Figure 2A). Skin biopsy revealed superficial and deep perianexial dermatitis with lymphocytic infiltration. Initial management with 40mg daily of isotretinoin was administrated for one year, with clinical improvement. Posterior adjustment of the dose was made to 20mg of isotretinoin daily for six months. The patient is currently participating in follow-up with no reappearance of symptoms (Figure 2b).

Discussion
The term morbus Morbihan refers to a district in Brittany, France, where Morbihan’s disease was first reported.2 Morbihan’s disease is characterized by chronic, recurrent erythema and edema of the central and upper aspect of the face followed by persistent swelling that can eventually lead to fibrotic induration. Symptoms caused by the associated facial disfiguration can negatively impact the patient cosmetically as well as psychologically.2–5 Palpebral involvement can cause a narrowing of the visual field. Morbihan’s disease is also known as rosacea lymphedema or solid persistent facial edema of rosacea.2–5 The disease course is marked by periods of recurrent exacerbations and partial regression of symptoms, as well as pachydermatous and scleromyxoedematous sequelae.6
Of note, persistent facial edema is not pathognomonic of this disease and can be a manifestation of several cutaneous disorders. Connelly and Winkelmann7 have categorized Morbihan’s disease into the groups congenital, infectious, malignant, inflammatory, and miscellaneous.
Morbihan’s disease has been described as a rare complication of mild-to-moderate acne of 2 to 5 years duration in young adults, with the onset of symptoms occuring in a span of 2 or 3 months or 4 to 9 years.8 The exact etiology remains unknown, but several hypotheses have been presented to date. In a review article by Barragán-Estudillo et al,9 the authors discuss a hypothesis by Winkelmann that suggests chronic inflammation can produce cellular inflammation and result in facial edema by a mechanism similar to that of the formation of edema in the extremities of patients with venous insufficiency and chronic cellulitis. Winkelmann also proposed acne as a recurrent focus of infection that perpetuates edema. Barragán-Estudillo et al9 also discuss another hypothesis by Camacho and Winkelmann that suggests the rupture of the follicular wall triggers an outflow of keratin and Demodex mites that migrate into the dermis, generating an inflammatory reaction.
Skin biopsies are typically used to rule out other diagnoses among patients with Morbihan’s disease, as histopathologic findings of this condition are limited and nonspecific. Histopathology typically shows dilated blood vessels, perifollicular fibrosis, and perivascular and perifollicular infiltrate of lymphocytes, histiocytes, and neutrophils associated with stromal edema.4,10 Principal differential diagnoses include Melkersson–Rosenthal syndrome, systemic lupus erythematosus, dermatomyositis, sarcoidosis, chronic actinic dermatitis, and chronic contact dermatitis.4
Diagnosis of Morbihan’s disease is often delayed because, in most cases, the clinical suspicion isn’t established until years after the edema has appeared, with no correlation between acne and edema and a poor improvement following specific acne treatments.9
Currently, there are no guidelines for the treatment of Morbihan’s disease, and therapeutic options are limited. Nonetheless, due to the impact Morbihan’s disease can have on patient quality of life, every attempt should be made to treat the condition.5,11 Systemic therapy includes corticosteroids, antibiotics, thalidomide, and antihistamines.4 Several reports regarding systemic corticosteroid use have shown either no response or a transient effect.5 Systemic corticosteroids can temporarily manage the inflammation, but recurrence of symptoms typically occurs upon discontinuation.8 Promising results, however, have been achieved using a combination of isotretinoin with ketotifen or clofazimine.12 Antibiotics, antihistamines, and corticosteroids have also been used in a variety of combinations but do not demonstrate any advantage over the use of isotretinoin with either ketotifen or clofazimine.13 Ketotifen’s mechanism of action might be its direct interference with mastocyte degranulation, which might be necessary for the formation of collagen deposits and fibrosis.7 However, clinical response with these therapies has been largely inadequate.4 Other reported therapies include facial massage and, in the case of persistent erythema and edema, excision of redundant edematous tissue.12 However, one problem, when evaluating treatment outcomes for Morbihan’s disease, is the absence of standardized reference points.14
One of the most promising therapies for treatment of Morbihan’s disease is long-term use of isotretinoin. Previous reports have recommended doses of 10 to 50mg per day for 4 to 6 weeks.4 Isotretinoin in higher doses (40–80 mg/day) for 10 to 24 months has also led to successful outcomes.11 Smith and Cohen4 reported the details of five patients treated with long-term, high doses of isotretinoin (40–80 mg/day for up to 24 months) with successful and lasting results.
Isotretinoin’s effect is based on the same immunomodulatory and anti-inflammatory properties that make it useful for rosacea. It has a role in the reparation of structural tissue damage made by alterations in the cellular metabolism, as well as inhibitory effects on fibroblast proliferation and migration and proliferation of connective tissue components. Isotretinoin therapy might modify the deleterious effects of chronic inflammation that results in damage to the dermal matrix.4
The prompt treatment of Morbihan’s disease is essential in order to avoid the anatomic complications. Dermatologists should consider the typical clinical picture and exclude several differential diagnoses using histological findings when suspicious of morbus Morbihan in their patients.15
We treated all three of the presented patients with isotretinoin using an initial daily dose of 40mg for a minimum of 12 months, achieving substantial clinical improvement after eight months, seven months, and four months of therapy for Cases 1, 2, and 3, respectively. Dosage was then reduced to 20mg for 6 to 12 months in all three patients. Adverse effects were minimal. Sunblock was recommended as follow-up support treatment. The achieved successful clinical response was maintained with no recurrence of the symptoms in the three patients.
Conclusion
Treatment of Morbihan’s disease is challenging due to its nonspecific etiology and lack of treatment consensus. Many different systemic and even surgical treatment approaches have been used with variable results. The challenge lies in choosing the right treatment that presents a successful and lasting response. Isotretinoin can be good choice for some patients with Morbihan’s disease. The purpose of this report is add data to the existing literature regarding the long-term use of isotretinoin as an effective and safe option with sustained and satisfactory outcomes for treating patients with Morbihan’s disease.
References
- Ranu H, Lee J, Hee TH. Therapeutic hotline: successful treatment of Morbihan’s disease with oral prednisolone and doxycycline. Dermatol Ther. 2010;23(6):682–685.
- Wohlrab J, Lueftl M, Marsch WC. Persistent erythema and edema of the midthird and upper aspect of the face (morbus morbihan): Evidence of hidden immunologic contact urticarial and impaired lymphatic drainage. J Am Acad Dermatol. 2005;52(4):595–602.
- Franco M, Hidalgo-Parra I, Bibiloni N, et al. Enfermedad de Morbihan. Dermatol Argent. 2009;15(6):434–436.
- Smith LA, Cohen DE. Successful long-term use of oral isotretinoin for the management of Morbihan disease. A case series report and review of the literature. Arch Dermatol. 2012;148(12): 1395–1398.
- Fujimoto N, Mitsuru M, Tanaka T. Successful treatment of Morbihan disease with long-term minocycline and its association with mast cell infiltration. Acta Derm Venereol. 2015;95(3): 368–369.
- Leigheb G, Boggio P, Gattoni M, et al. A case of Morbihan’s disease chronic upper facial erythematous oedema. Acta Derm Venerol. 1993;2(2):57–61.
- Harvey DT, Fenske NA, Glass FL. Rosaceous lymphedema: a rare variant of a common disorder. Cutis. 1998;61(6):321–324.
- Hernández-Cano N, De Lucas-Laguna R, Lázaro-Cantalejo TE, et al. Edema sólido facial persistente asociado a acné vulgar: tratamiento con corticoides sistémicos. Actas Dermosifiliogr. 1999;90:185–195.
- Barragán-Estudillo ZF, Rivera-Gómez MI, López-Ibarra MM, et al. Edema sólido facial persistente relacionado con acné (Morbihan). Dermatol Rev Mex. 2012;56(5):341–345.
- Nagasaka T, Koyama T, Matsumura K, et al. Persistent lymphoedema in Morbihan disease: formation of perilymphatic epithelioid cell granulomas as a possible pathogenesis. Clin Exp Dermatol. 2008;33(6):764–767.
- Balakirski, G, Baron JM, Megahed M. Morbus Morbihan als sonderform der rosazea: einblick in die pathogenese und neue therapieoptionen. Der Hautarzt. 2013;64(12):884–886.
- Bechara FG, Jansen T, Losch R, et al. Moribhan’s disease: treatment with CO2 laser blepharoplasty. J Dermatol. 2004;31(2):113–115.
- Mazzatenta C, Giorgino G, Rubegni P, de Aloe G, Fimiani M. Solid persistent facial oedema (Morbihan’s disease) following rosacea, successfully treated with isotretinoin and ketotifen. Br J Dermatol. 1997;137(6):1011–1031.
- Crespo-Cobo P, Martos-Díaz PL, Ruiz-Molina D, et al Drenaje linfático manual en el linfedema facial. Rehabilitación (Madr). 2003;37(5):291–293.
- Lamparter J, Kottler U, Cursiefen C, et al. Morbus Morbihan: seltene ursache ödematöser lidschwellungen. Ophthalmologe (Germany). 2010;107(6):553–557.

