 J Clin Aesthet Dermatol. 2024;17(3):18–20.
J Clin Aesthet Dermatol. 2024;17(3):18–20.
by Ayşe Akman-Karakaş, MD; Raza Khan, MD; and Amor Khachemoune, MD
Dr. Akman-Karakas is with Akdeniz University’s School of Medicine Department of Dermatology and Venereology in Antalya, Turkey. Dr. Khan is with the University of Oklahoma Health Sciences Center College of Medicine in Oklahoma City, Oklahoma. Dr. Khachemoune is with the Department of Dermatology at SUNY Downstate in Brooklyn, New York. Additionally, Dr. Khachemoune is with the Department of Dermatology at Veterans Affairs New York Harbor Healthcare System in Brooklyn, New York.
FUNDING: No funding was provided for this article.
DISCLOSURES: The authors have no conflicts of interest relevant to the contents of this article.
ABSTRACT: Biopsies and excisions of mucosal surfaces can be challenging due to poor visualization and bleeding control. Surgeons have utilized chalazion clamps to overcome these challenges. However, its original design incorporates a locking mechanism which restricts its use to more proximal mucosal surfaces, does not allow for flexible exertional pressure control by the operator, and it is only available in one size. We designed a modified chalazion clamp without a locking mechanism and in two different sizes and ring diameters to overcome these challenges. In this report, we demonstrate the enhanced utility and effectiveness of the modified chalazion clamp in dermatological procedures through different cases. Keywords: Chalazion clamp, modified chalazion clamp, biopsies, bleeding control, mucosal surfaces
Introduction
The chalazion clamp was originally designed to assist with the surgical removal of a chalazion, a well-circumscribed swelling of the eyelid.1 The tool has since been utilized in surgical procedures that involve easily accessible mucosal regions, such as the inner lips or the external genitalia. Structured like forceps, the chalazion clamp features a proximal shaft with a thumbscrew, as well as two distal arms. One distal arm is equipped with a flat, solid plate, while the other with a ring-like aperture. Its unique design allows surgeons to achieve enhanced manipulation, homeostasis, and visibility of the surgical field.1–3
In its current use, the clamp is placed on the targeted area with the ring-like aperture around the biopsy or excision site, and then adequately tightened with the thumbscrew for stabilization. Since mucosal surfaces are particularly vascular, the clamp renders the area temporarily avascular and taut, which allows for enhanced visibility and bleeding control. Once the biopsy or excision is complete, the clamp is loosened to allow for approximation of the wound edges and closure. Any residual bleeding points can then also be easily detected and cauterized, or additional sutures may be placed as necessary for appropriate homeostasis. Finally, the clamp is completely removed.1
Modifications to the traditional chalazion clamp
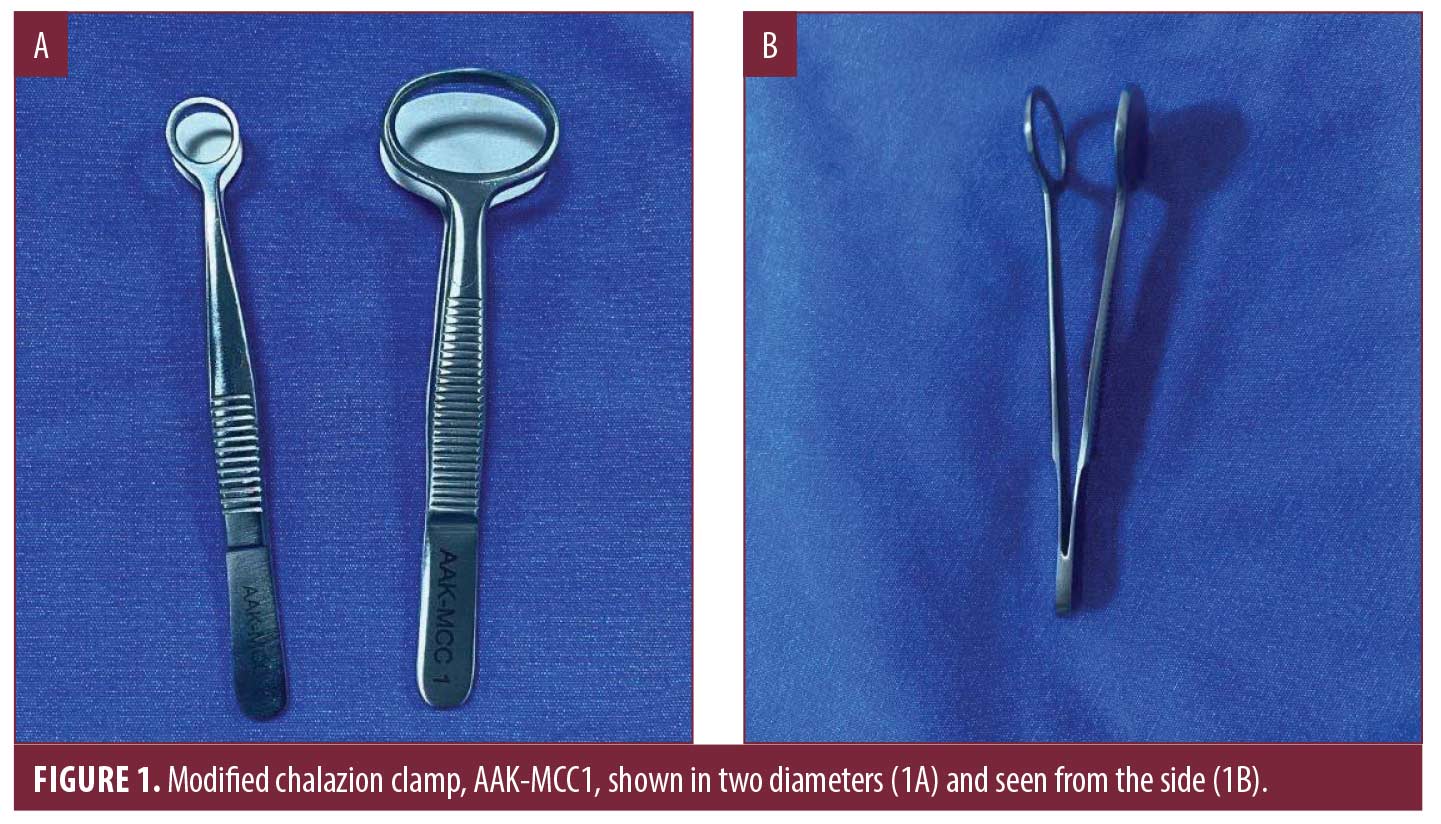
A limitation of the original chalazion clamp is that its design restricts its use to more proximal mucosal surfaces, as the placement of the thumbscrew high on the shaft makes it difficult to access distal surfaces. Therefore, the modified chalazion clamp was designed by Ayşe Akman-Karakaş (AAK), and produced at Samsun Mikrocerrahi Aletler, Samsun, as seen in Figure 1. The modified clamp does not contain a thumbscrew allowing it to be used on distal mucosal surfaces that were previously inaccessible with the original design, while also allowing for greater flexibility of use without having to adjust the thumbscrew. In addition, it was designed in two sizes and ring diameters to allow for more effective use on different lesions.
Serial Case Studies
We present a series of three cases where the modified instrument and techniques were successfully used.
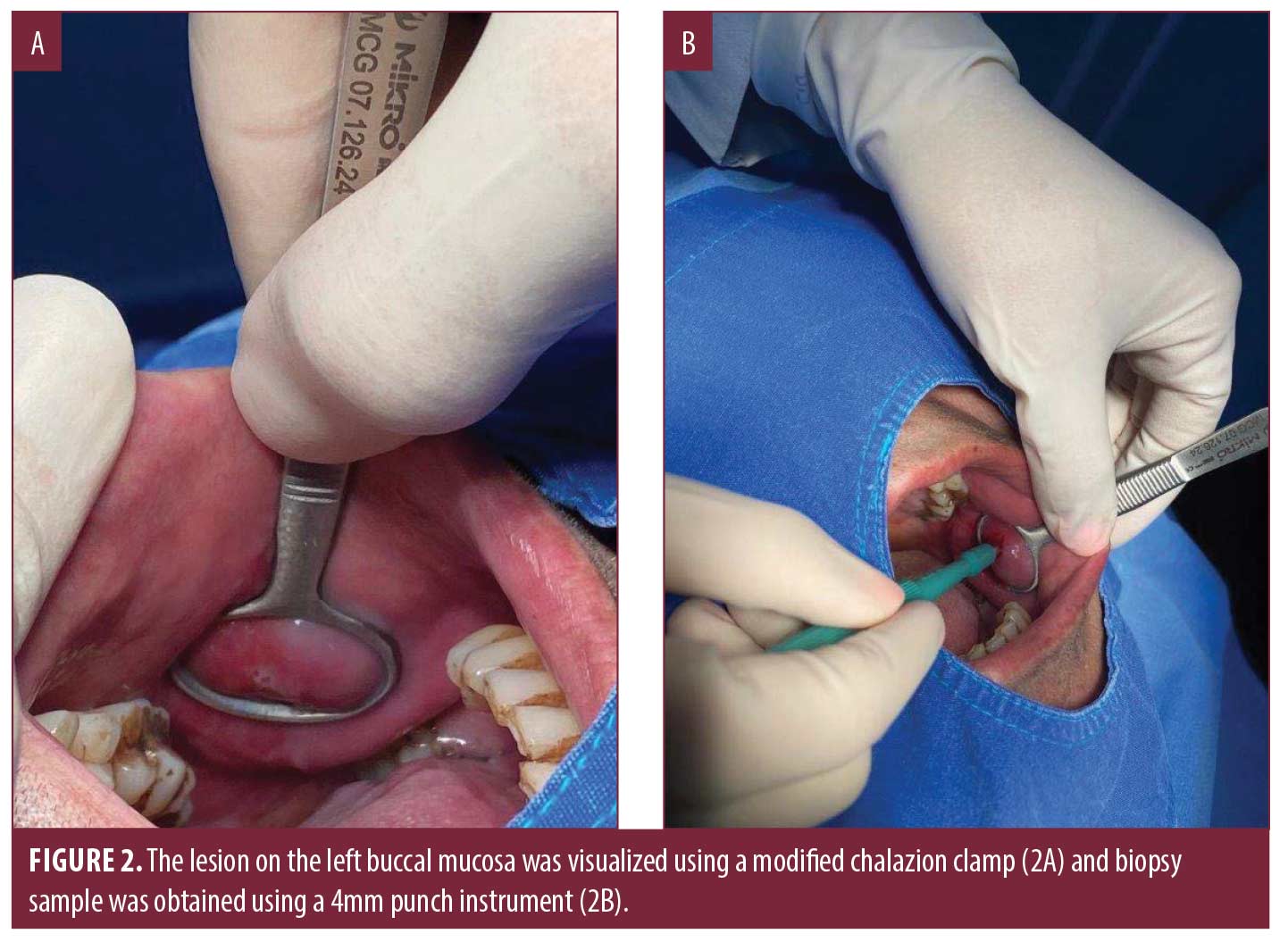
Case 1. A biopsy was planned of an eroded lesion on the left buccal mucosa of a 57-year-old man with the preliminary clinical diagnosis of lichen planus versus pemphigus vulgaris as seen in Figure 2. After administration of local anesthetic using lidocaine/epinephrine, the lesion on the left buccal mucosa was easily manipulated and visualized using the modified chalazion clamp and biopsy sample was obtained using a 4mm punch instrument. Finally, the lesion was sutured achieving homeostasis.
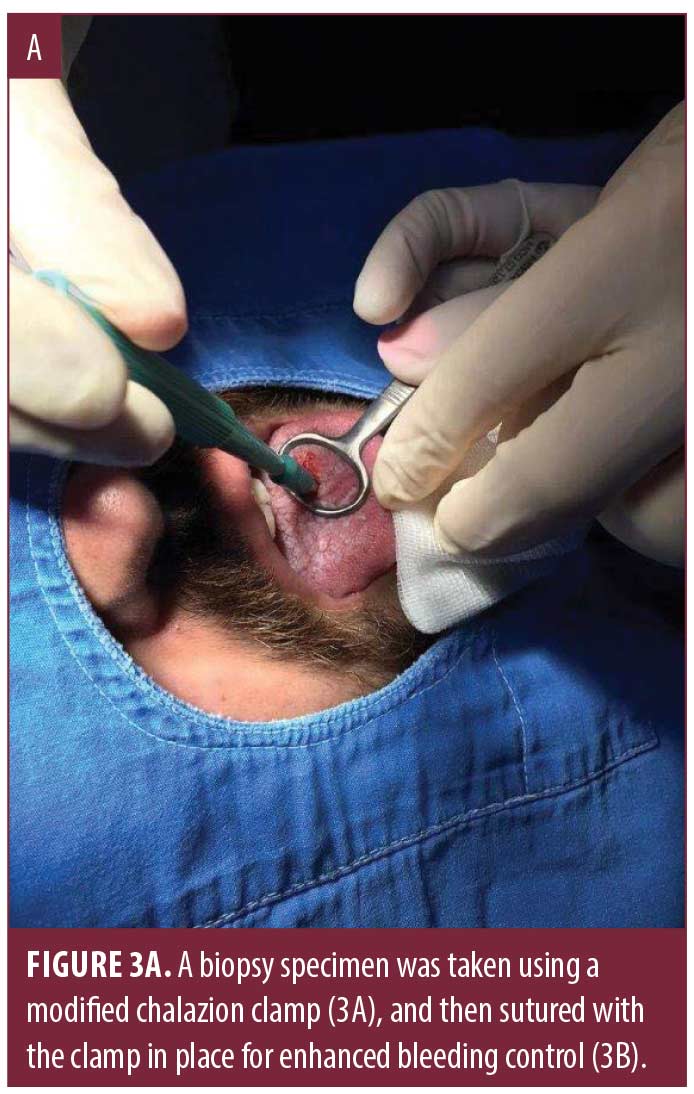
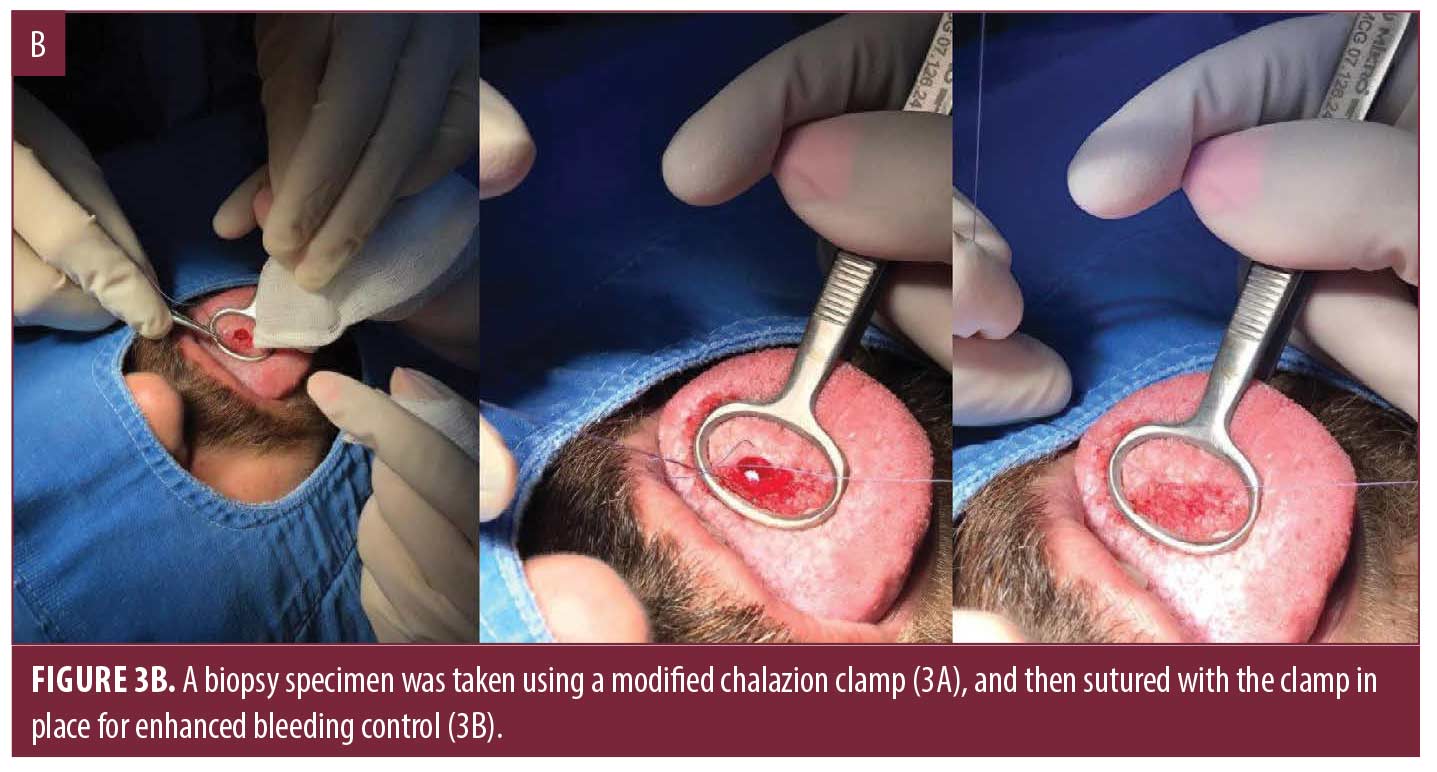
Case 2. A biopsy of a 2x1cm white plaque on the tongue of a 26-year-old man with the preliminary clinical diagnosis of leukokeratosis versus lichen planus was planned as seen in Figure 3. After administration of local anesthetic using lidocaine/epinephrine, the lesion on the tongue was visualized using the modified chalazion clamp and the biopsy sample was obtained using a 4mm punch instrument. The pressure exerted on the clamp during the procedure allowed for enhanced bleeding control on a particularly vascular area. The lesion was then sutured with absorbable sutures to achieve complete homeostasis.
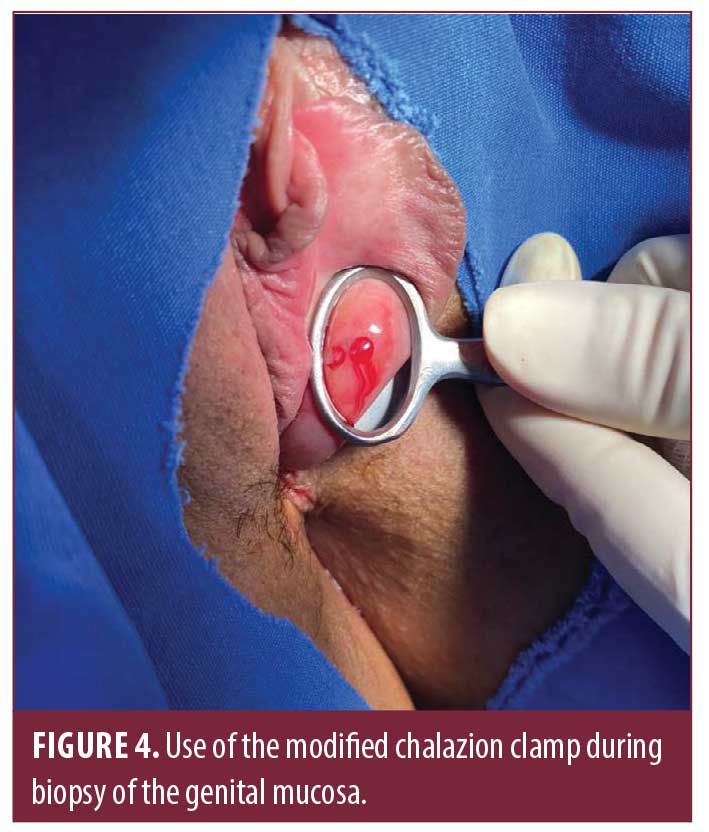
Case 3. A biopsy was taken from an erythematous, edematous, velvety, and slightly eroded area on the inner surface of the vulva of a 46-year-old female with the clinical differential diagnosis of plasma cell vulvitis versus lichen planus versus mucous membrane pemphigoid as seen in Figure 4. The modified chalazion clamp provided easier manipulation and visualization of a sensitive area during the biopsy, while allowing for flexible pressure exertion for bleeding control as opposed to constant readjustment of the thumbscrew.
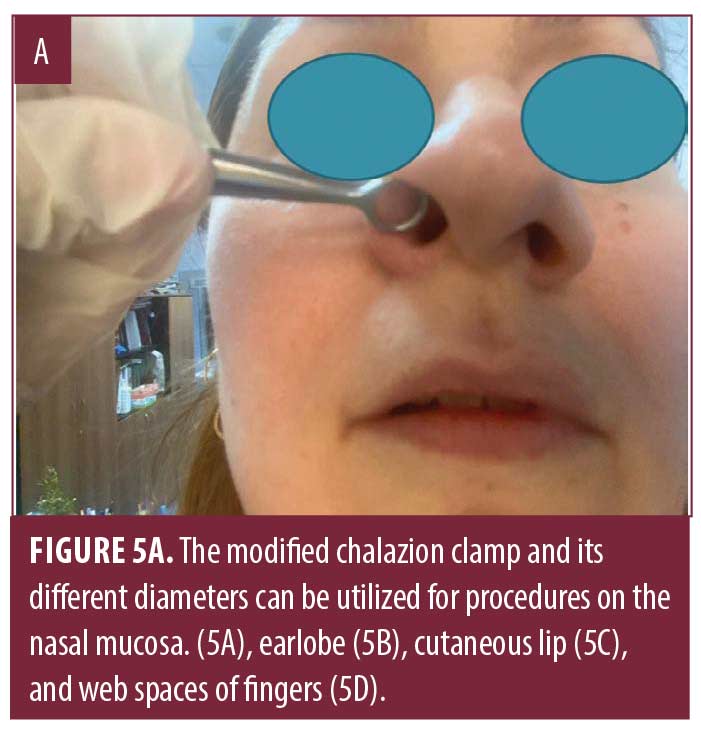
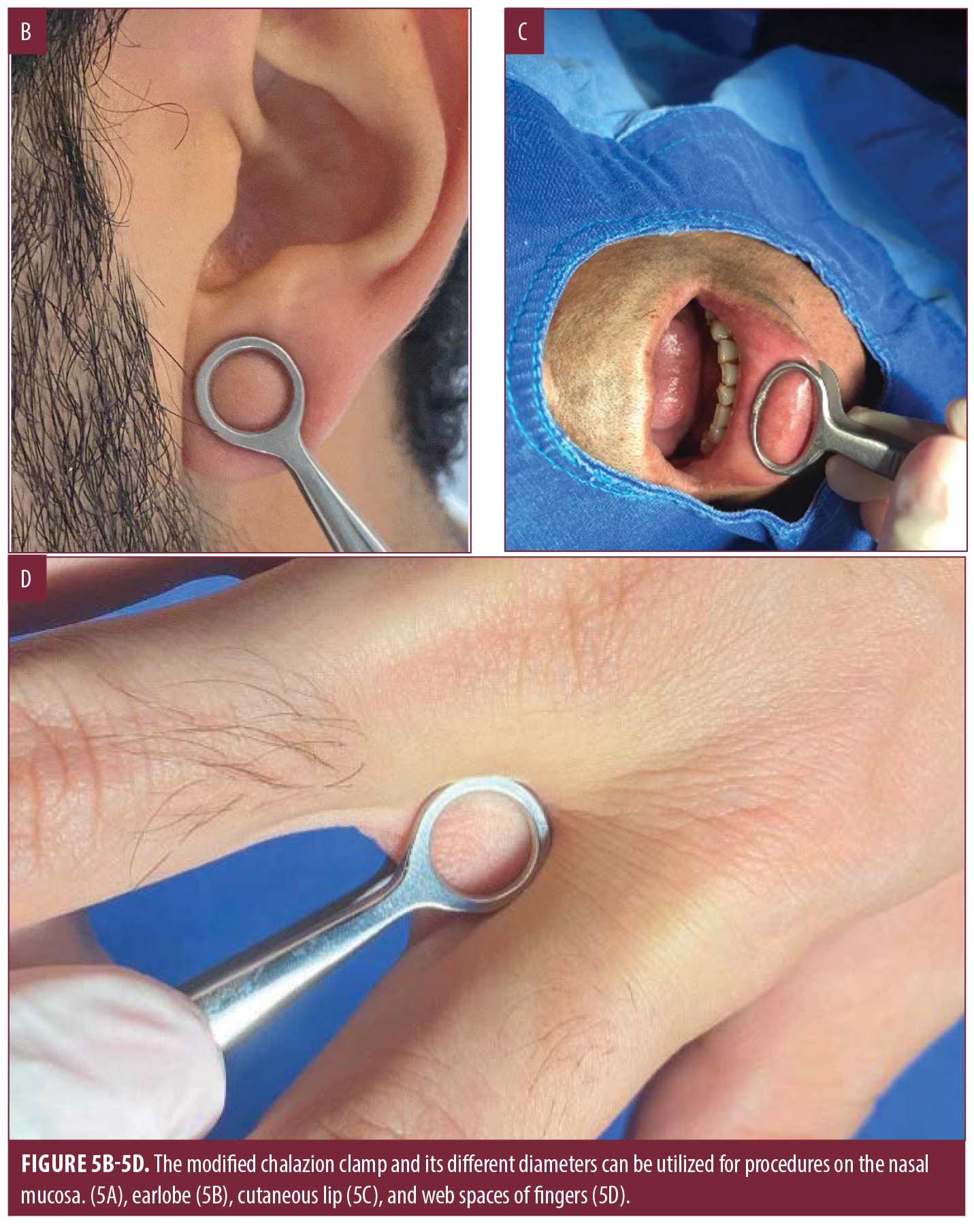
In addition to the areas shown, the modified chalazion clamp can also be used for procedures in areas such as nasal mucosa, earlobes, cutaneous lip, and web spaces of fingers and toes utilizing the two different sizes and ring diameters (Figure 5).
Discussion
Performing biopsies and excisions in mucosal areas can be challenging due to poor visualization and bleeding control. Chalazion clamps with a thumbscrew have been utilized to overcome these challenges. Although the thumbscrew allows for better stabilization during longer procedures, its design hinders use on distal mucosal lesions and can pose an additional potential risk of local ischemia due to compromised vasculature secondary to prolonged locking.
To address these issues, we developed a modified chalazion clamp without a thumbscrew and demonstrated its utility in dermatologic procedures in the cases presented above. The modified chalazion clamp has shown to be mainly superior in three ways. First, it allows for better access to more distal mucosal sites for both diagnostic and therapeutic purposes. Secondly, the lack of a locking mechanism allows for controlled pressure exertion without having to readjust the screw which enhances flexibility during the procedure, minimizes complications from prolonged locking, and makes the procedure more efficient. Finally, the two different sizes available allow for more effective use depending on the lesion size.
With its aforementioned advantages, including avoidance of complications such as ischemia, we anticipate the modified chalazion clamp will be a useful tool for clinicians, such as dentists, ear, nose and throat surgeons, gynecologists and especially dermatologists, for both diagnostic and surgical treatment purposes.
Acknowledgements
We would like to acknowledge Sinan Nane, Ahmet Demir, Servinaz Enli, Aslı Özçentik, Mehmet Ali Koyuncu, and Şeyma Erdoğuş, for their contributions to this work.
References
- Shah L, Fogden S, Majumdar A. Use of a chalazion clamp for intraoral biopsies: a technical note. Br J Oral Maxillofac Surg. 2020 Jan;58(1):105–106.
- Jha AK, Ganguly S. Chalazion clamp in dermatology revisited. Indian J Dermatol Venereol Leprol. 2015 May-Jun;81(3):280–281.
- Agrawal S, Jaiswal S, Hajare S. Use of the Chalazion clamp for stretch and stability of lip mucosa during micropigmentation. J Am Acad Dermatol. 2020 May 19:S0190-9622(20)30927-0.

