 J Clin Aesthet Dermatol. 2024;17(3):21–23.
J Clin Aesthet Dermatol. 2024;17(3):21–23.
by Noureddine Litaiem, MD; Amel Chabbouh, MD; Ines Chabchoub, MD; Radhi Ben Naceur, MD; Mourad Mokni, MD; and Faten Zeglaoui, MD
Drs. Litaiem, Chabbouh, Chabchoub, and Zeglaoui are with the Department of Dermatology at Charles Nicolle Hospital in Tunis, Tunisia. Dr. Mokni is with the Faculty of Medicine of Tunis at University of Tunis El Manar in Tunis, Tunisia. Additionally, Drs. Litaiem, Chabbouh, Chabchoub, and Zeglaoui are with the Faculty of Medicine of Tunis at the University of Tunis El Manar in Tunis, Tunisia. Dr. Ben Naceur is with Institute Salah Azaiez in Tunis, Tunisia. Additionally, Dr. Mokni is with the Department of Dermatology at La Rabta Hospital in Tunis, Tunisia.
FUNDING: No funding was provided for this article.
DISCLOSURES: The authors have no conflicts of interest relevant to the contents of this article.
ABSTRACT: Becker’s nevus syndrome is defined by the association of a Becker nevus with homolateral breast hypoplasia or more rarely skeletal cutaneous or muscle deformities. Early diagnosis is important, especially in female patients to prevent and treat breast hypoplasia. We report two cases of Becker nevus syndrome with serious functional impairment and discuss possible treatment options.
Introduction
Becker’s nevus syndrome was defined in 1997 by Happle and Koopman1 by the association of a Becker nevus with ipsilateral breast hypoplasia or more rarely skeletal cutaneous or muscle deformities. Only a few cases are reported in the literature.2 We report two cases of Becker nevus syndrome with serious functional impairment and discuss the importance of early diagnosis in female patients.
Case presentation
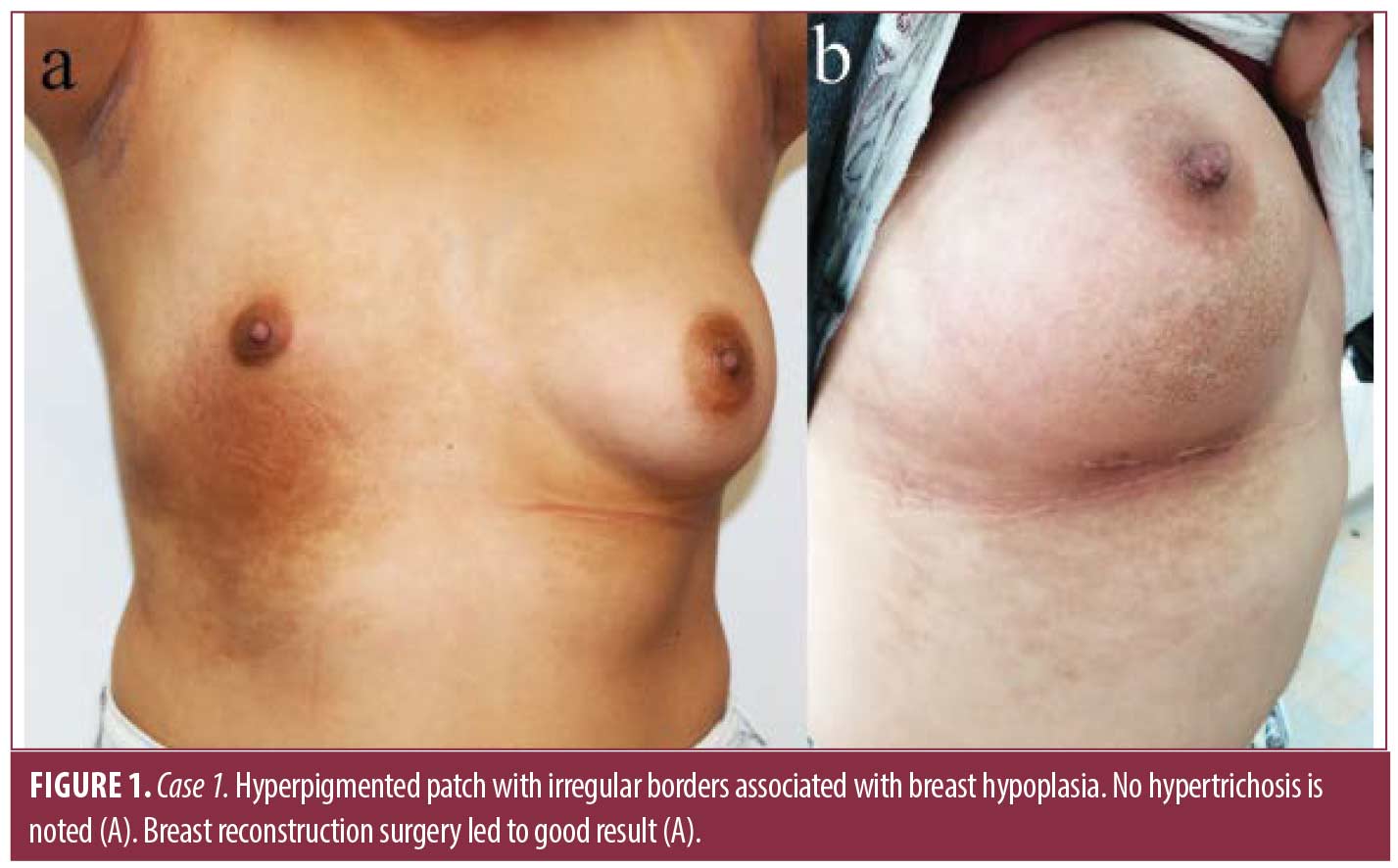
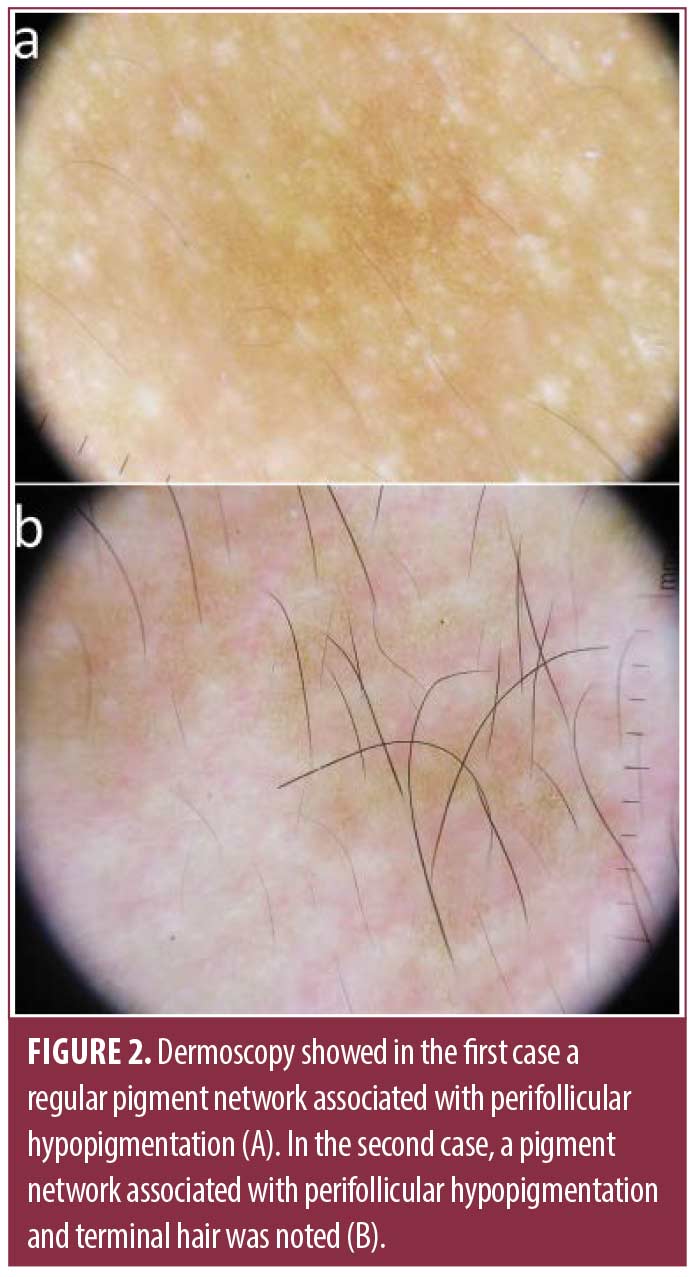
Case 1. A 15-year-old female patient, with no past medical history, presented with a three-year history of a hyperpigmented lesion on the right chest. Physical examination revealed a hyperpigmented skin patch with irregular borders measuring 20cm in size with a velvety texture, without hypertrichosis (Figure 1A). Homolateral breast hypoplasia was noted. Dermoscopy showed a regular pigment network and perifollicular hypopigmentation (Figure 2A). The diagnosis of Becker’s nevus syndrome was made. Breast reconstruction surgery was performed with good results (Figure 1B).
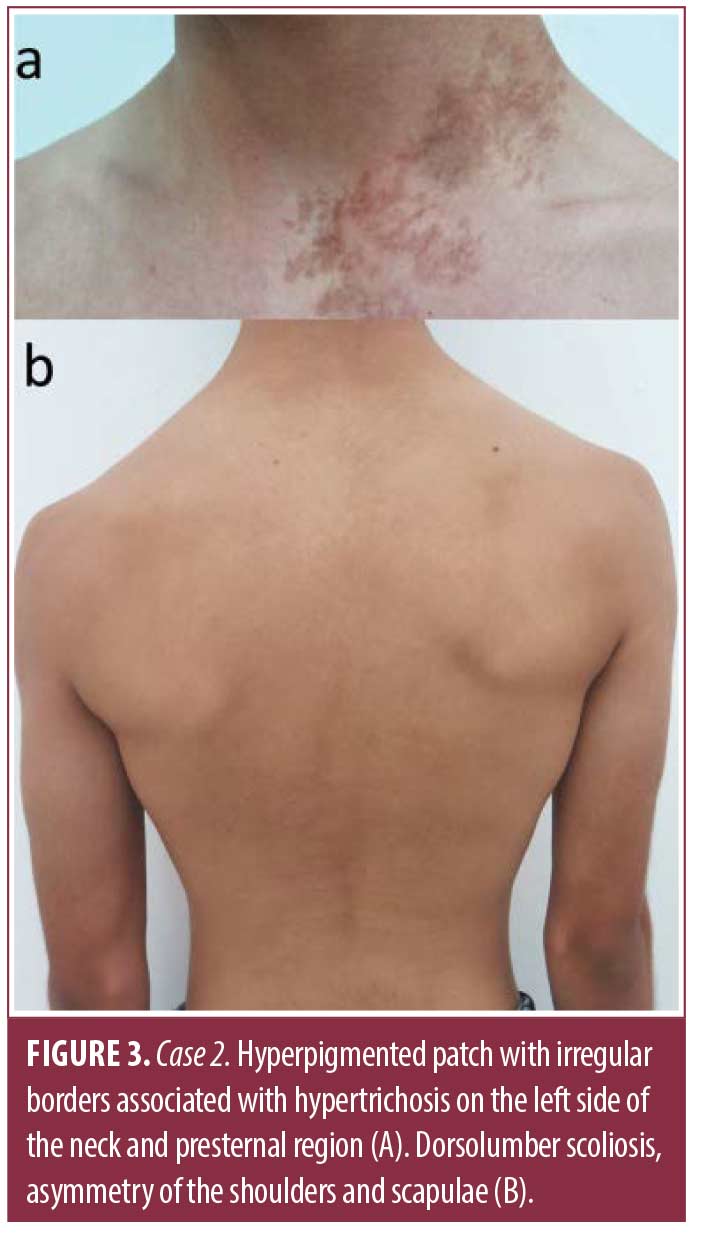
Case 2. An 18-year-old male patient with a history of dorsolumbar scoliosis, asymmetry of the shoulders and scapulae, and retraction of the hamstring muscles presented with a hyperpigmented patch that had been developing for three years, located on the left side of the neck and presternal region. Physical examination showed hyperpigmented patch with irregular borders measuring 15cm associated with hypertrichosis (Figure 3A). Dorsolumbar scoliosis, asymmetry of the shoulder and scapulae, and length discrepancy of the lower limbs were noted. Dermoscopy showed pigment network and perifollicular hypopigmentation (Figure 2B). The diagnosis of Becker’s nevus syndrome was based on characteristic cutaneous findings and hypoplastic defects of the skeleton and muscles (Figure 3B).
Discussion
Becker’s nevus was first described in 1949 by Samuel William Becker.3 It presents as a pigmented patch that may be associated with hypertrichosis or localized acne. It is usually single and unilateral and has irregular borders. It is often located on the back, chest, and shoulders. Less frequently affected body areas include the face, the upper arms, and the lower body.2 Becker’s nevus represents the only epidermal nevus that does not follow Blaschko’s lines.2 The ratio of women to men is 1:3. The mean age at the onset of Becker’s nevus was 6.6 years (0-17 years). The mean age at diagnosis was 19.4 years (2-55 years).2 Dermoscopy provides clues to the diagnosis showing a pigment network, skin furrow hypopigmentation, perifollicular hypopigmentation, and dotted vessels.4
Becker’s nevus syndrome associates Becker’s nevus with other cutaneous and extracutaneous abnormalities. Less than 200 cases have been described worldwide.2 The most common associations are breast hypoplasia, scoliosis, segmental odontomaxillary hypoplasia, and supernumerary nipples.2 These disorders can be located in a different part of the body than Becker’s nevus. The pathogenesis of both Becker nevus and Becker’s nevus syndrome involves postzygotic mutations of the ACTB gene, which codes for beta-actin.6 Beta-actin is an intracellular cytoskeletal molecule involved in cell migration, gene expression, and Hedgehog signaling pathway. The Hedgehog signaling pathway is implicated in hair growth and muscle differentiation. Therefore, postzygotic mutations of the ACTB gene lead to hypertrichosis, epidermal pigmentation, and smooth muscle involvement. Becker’s nevus syndrome may reflect a mutation earlier in development, affecting multiple cell lineages compared to isolated Becker’s nevus.6
Evidence of an increased risk of malignancies in association with Becker’s nevus syndrome is lacking. Two cases of basal cell carcinoma have been reported in a non-photoexposed skin proximal to Becker’s nevus, and about 10 cases of melanoma developing on Becker’s nevus have been described. However, these associations may be purely coincidental due to the increased incidence of melanoma and basal cell carcinoma, and the underestimated incidence of Becker’s nevus. Besides, Becker’s nevus is not associated with melanocytic hyperplasia. To date, no cases of breast cancer associated with Becker’s nevus syndrome have been described in the literature.7–10
There are no formal treatment guidelines for Becker’s nevus syndrome. Several lasers have been used, with limited efficacy and risk of recurrence. Efficacy of the Er:YAG 2940nm is reported to be higher than Q-switched Nd:YAG 1064nm for pigment, although Nd:YAG laser 1064nm may be better for treating darker-skinned individuals.11 Topical flutamide has been used, leading to a satisfactory reduction of hyperpigmentation.12 Spironolactone is used in female patients with breast hypoplasia with remarkable breast development.5 Therefore, early diagnosis of Becker’s nevus syndrome in female patients with breast hypoplasia is critical prompting adequate medical treatment. Spironolactone might even prevent breast hypoplasia if initiated early enough.5 Breast lipofilling is a good alternative, leading to improvement in breast volume and hyperpigmentation.13 Some advanced cases require breast reconstruction surgery.14
Conclusion
Becker’s nevus syndrome is a rare syndrome that associates Becker’s nevus with cutaneous and extra-cutaneous disorders. The most frequently described extracutaneous manifestations are breast hypoplasia, scoliosis, segmental odontomaxillary, supernumerary nipple, and spina bifida. Dermatologists should be aware of this condition prompting early treatment. Screening for Becker’s nevus syndrome in women and early spironolactone treatment may prevent breast hypoplasia. In advanced cases, surgical management is necessary to improve patients’ quality of life.
References
- Happle R, Koopman RJ. Becker nevus syndrome. Am J Med Genet. 1997; 68:357–361.
- Torchia D. Becker nevus syndrome: A 2020 update. J Am Acad Dermatol. 2021 Aug;85(2):e101–e103. Epub 2021 Apr 2. PMID: 33819536.
- Becker SW. Concurrent melanosis and hypertrichosis in distribution of nevus unius lateris. Arch Dermatol Syph. 1949; 60: 155–160.
- Adya K, Inamadar A, Palit A. Dermoscopic Pigment Network: Characteristics in Non-melanocytic Disorders. Indian Dermatol Online J. 2020 Mar 9;11(2):146–153.
- Hernandez-Quiceno S, Uribe-Bojanini E, Ramírez-Jiménez JJ, et al. Becker’s Nevus Syndrome in a Pediatric Female Patient. Case Rep Pediatr. 2016;2016:3856518.
- Cai E, Sun B, Chiang A et al. Postzygotic Mutations in Beta-Actin Are Associated with Becker’s Nevus and Becker’s Nevus Syndrome. J Invest Dermatol. 2017 Aug;137(8):1795–1798.
- Sahu P, Dayal S, Kaur S, et al. Becker’s nevus associated with basal cell carcinoma: an unusual presentation in a sun-protected area. An Bras Dermatol. 2017 Jan-Feb;92(1):145–147.
- Patrizi A, Medri M, Neri I, et al. Becker naevus associated with basal cell carcinoma, melanocytic naevus and smooth-muscle hamartoma. J Eur Acad Dermatol Venereol. 2007 Jan;21(1):130–132.
- Akdogan N, Elcin G, Gokoz O. The co-existence of cutaneous melanoma and urticaria pigmentosa in a patient with Becker’s nevus. J Cosmet Dermatol. 2020 May;19(5):1268–1270.
- Ruto F, Joly P, Fusade T, Lauret P. Becker naevus and malignant melanoma. Dermatology. 1992;184(1):83.
- Zhong Y, Yang B, Huang L, et al. Lasers for Becker’s nevus. Lasers Med Sci. 2019 Aug;34(6):1071–1079.
- Taheri A, Mansoori P, Sandoval LF, et al. Treatment of Becker nevus with topical flutamide. J Am Acad Dermatol. 2013 Sep;69(3):e147–148.
- Ho Quoc C, Fakiha M, Meruta A, et al. Breast lipofilling: A new treatment of Becker nevus syndrome. Ann Chir Plast Esthet. 2015 Aug;60(4):336–339.
- Nunes RB, Silva MFD, Coltro PS, et al. Treatment of Breast Hypoplasia in Becker Nevus Syndrome. Breast J. 2017 Sep;23(5):603–604.