 J Clin Aesthet Dermatol. 2022;15(3):16–20.
J Clin Aesthet Dermatol. 2022;15(3):16–20.
by Teerapong Rattananukrom MD; Poonkiat Suchonwanit MD;
Kunlawat Thadanipon, MD; and Vasanop Vachiramon, MD
All authors are with the Division of Dermatology, Faculty of Medicine, Ramathibodi Hospital at Mahidol University in Bangkok, Thailand. Dr. Thadanipon is also with the Department of Clinical Epidemiology and Biostatistics, Faculty of Medicine, Ramathibodi Hospital at Mahidol University in Bangkok, Thailand.
FUNDING: No funding was provided for this article.
DISCLOSURES: The authors report no conflicts of interest relevant to the content of this article.
ABSTRACT: Background. Dermatoscopy is a noninvasive diagnostic tool for pigmented lesions. However, data regarding dermatoscopic features in melasma and Hori’s nevus, which are commonly found in Asian populations, are still lacking. In addition, melasma coexisting with Hori’s nevus presents a particular diagnostic challenge and they generally require different treatments.
Objective. We sought to describe the dermatoscopic features of melasma and Hori’s nevus and to establish diagnostic clues for each condition.
Methods. Fifty patients with melasma and 46 patients with Hori’s nevus were enrolled in the study. Dermatoscopic pictures were taken with Dermlite DL200 HR (3Gen, San Juan Capistrano, Califorinia) and evaluated by two blinded board-certified dermatologists.
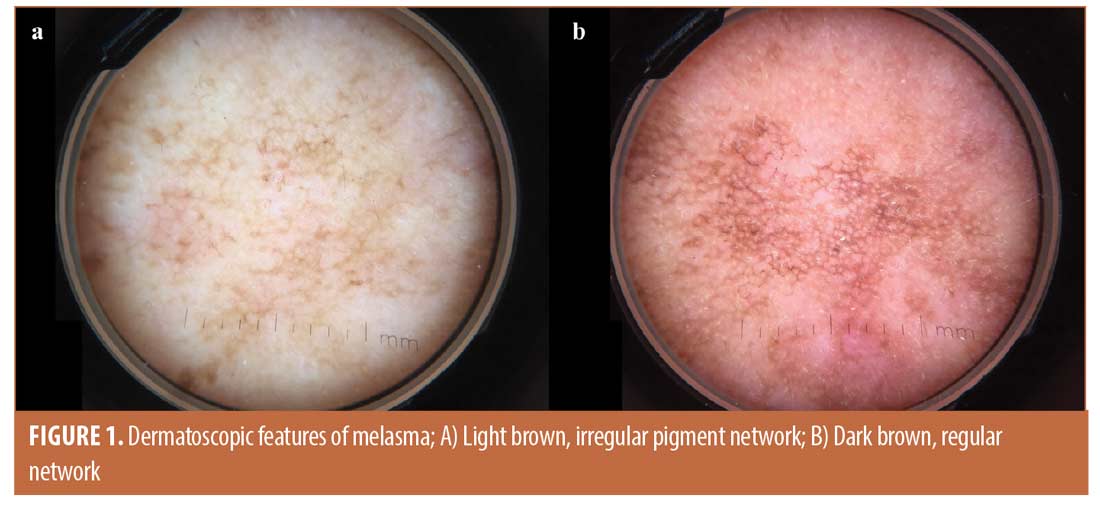
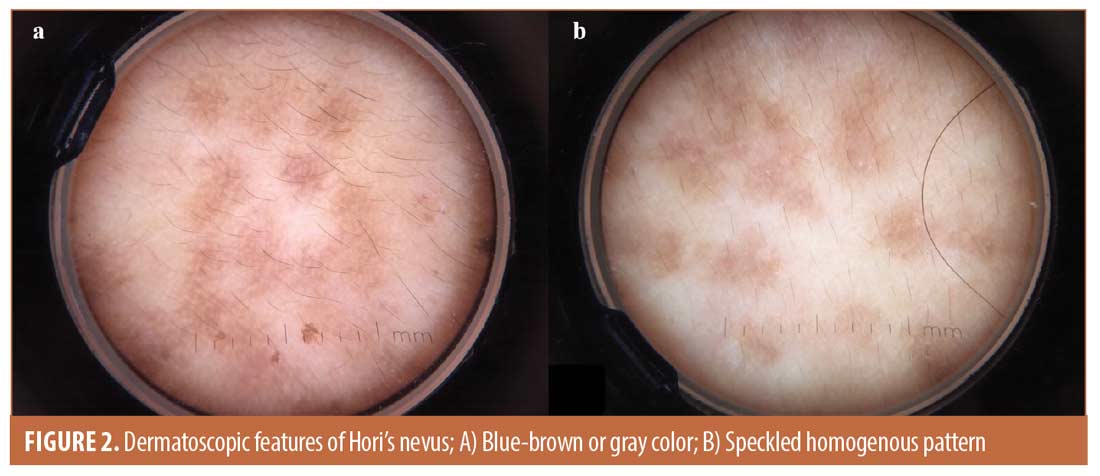
Results. The dermatoscopic features more prominently seen in melasma compared to Hori’s nevus include light brown pigmentation (98% vs. 10.9%, P<0.001), regular pigment network (38% vs. 2.2%, P<0.001), irregular pigment network (98% vs. 63%, P<0.001), arcuate structure (68% vs. 13%, P<0.001), circles (48% vs. 10.9%, P<0.001), sparing of follicles and sweat gland openings (98% vs. 4.3%, P<0.001), and telangiectasias (52% vs. 19.6%, P=0.001). In contrast, the common features of Hori’s nevus include blue-brown or grey pigmentation (63% vs. 0%, P=0.001) and speckled homogenous pattern (52.2% vs. 0%, P<0.001).
Conclusion. Dermatoscopy is a useful diagnostic tool for distinguishing between melasma and Hori’s nevus. In patients with coexistence of both conditions, dermatoscopy can be used to confirm the diagnosis and aid the proper treatment.
Keywords. Acquired bilateral nevus of Ota-like macules, chloasma, dermoscopy, Hori’s nevus, hyperpigmentation
Melasma and Hori’s nevus (acquired bilateral nevus of Ota-like macules, ABNOM) are common acquired pigmentary disorders that bring about cosmetic concerns among Asian patients. Melasma is caused by hyperfunctional melanocytes, increased melanin synthesis in the epidermis, and increased melanophages in the dermis. It usually presents with symmetrical, hyperpigmented patches with an irregular border, occurring on sun-exposed areas, especially on the face and malar area.1,2 Unlike melasma, Hori’s nevus is a form of acquired dermal melanocytosis caused by misplaced dendritic and spindle-shaped melanocytes dispersed in the papillary and mid dermis. It is characterized by bilateral, multiple speckled blue-brown and/or slate-gray macules predominantly on the malar area. Both disorders could be aggravated by sunlight, oral contraceptives, or other unknown factors,1-4 but each of them requires different treatment approaches. The first-line treatment for melasma includes topical medications, whereas, chemical peeling, non-ablative lasers, and energy-based devices (e.g., low fluence Q-switched Nd:YAG laser, picosecond lasers, copper-bromide laser, fractional non-ablative lasers, intense pulsed light, etc.) are considered second-line treatments.5 On the contrary, the first-line treatment of Hori’s nevus includes pigment-specific lasers with higher fluence settings (e.g., 1,064-nm Q-switched Nd:YAG laser, 755-nm picosecond alexandrite laser, etc.).6 Melasma coexisting with Hori’s nevus, which is not uncommon in Asian patients, presents a particular diagnostic challenge and requires multimodal treatments. Although histopathology should be used to establish a definite diagnosis, the practicality of skin biopsy on the face is limited due to cosmetic concerns. Dermatoscopy may be a good option for making a diagnosis.
Dermatoscopy is a noninvasive diagnostic tool that can identify colors, morphology, and patterns of pigmented lesions. According to a literature review, dermatoscopic features commonly found in melasma are brown or gray pigmentation, regular and/or irregular pigment network, arcuate or curved structure, circles, and follicular sparing.7-9 However, dermatoscopic features of Hori’s nevus have not been well investigated. In addition, a comparative study of dermatoscopic features between melasma and Hori’s nevus is lacking. Our study aimed to describe dermatoscopic features of melasma and Hori’s nevus, and to compare their dermatoscopic features in order to establish diagnostic clues for each condition.
Methods
This was a cross-sectional pilot study which included patients with either of melasma or Hori’s nevus who attended the dermatology clinic of a university-based hospital (Ramathibodi Hospital, Mahidol University, Bangkok, Thailand). Melasma and Hori’s nevus were diagnosed clinically by a board-certified dermatologist who specializes in pigmentary disorders and dermatoscopy. The clinical criteria for melasma can be defined as symmetrical reticulated hyperpigmented patches with irregular borders sometimes admixed with brownish macules on the centrofacial region, malar cheeks, and mandible. The macules of melasma have an irregular, geographical edge and involve large areas of the cheek.10 In contrast, the clinical criteria for Hori’s nevus include speckled blue-brown and or slate-gray macules with a discrete border which occur in clusters on the malar area, zygomas, upper eyelids, and lateral sides of the forehead.11
Patients who had coexistence of melasma and Hori’s nevus, pregnancy, thyroid diseases, previous laser treatments, use of oral contraceptives, and other medications such as phenytoin, antimalarials, amiodarone, and phototoxic drugs were excluded. The study protocol was approved by the Mahidol University Institutional Review Board for Ethics in Human Research (protocol number MURA2017/667). Written informed consent was obtained from all patients before enrollment.
Dermatoscopy was performed by the same investigator throughout the study using a polarized light handheld dermatoscope with 10-fold magnification (Dermlite DL200 HR; 3Gen, San Juan Capistrano, California). Three or more dermatoscopic pictures on malar areas of each patient were taken using a smartphone with a high resolution of eight million pixels (iPhone 6, Apple Inc, Cupertino, California). The pictures were evaluated independently by two blinded board-certified dermatologists in three main aspects: colors, morphological patterns, and other findings such as sparing of the follicles and sweat gland openings, and patterns of telangiectasias. When the readings by the two dermatologists were dissimilar, a third opinion was given by another blinded dermatologist and the disagreement was solved by a consensus.
SPSS Statistics version 18 (SPSS Inc., Chicago, Illinois) was used for statistical analysis. P<0.05 was considered statistically significant. Differences in each dermatoscopic feature between melasma and Hori’s nevus were analyzed using the chi-square or Fisher’s exact test. Inter-rater reliability between the two dermatologists who evaluated the dermatoscopic pictures was assessed using kappa statistic, of which the values >0.6 indicated substantial strength of agreement.
Results
Demographic data. Fifty patients with melasma and 46 patients with Hori’s nevus were recruited in the study. The mean age of onset in patients with melasma and Hori’s nevus was 43±8 and 33±10 years, respectively. Forty-eight female patients (96%) were presented in the melasma group, whereas 44 female patients (95.7%) were identified in the Hori’s nevus group. In the melasma group, 29 and 21 patients had Fitzpatrick Skin Type (FPT) III and FPT IV, respectively. Thirty-nine patients and seven patients had FPT III and FPT IV, respectively, in the Hori’s nevus group. Both conditions followed a symmetrical distribution in which melasma was presented predominantly on both cheeks and forehead, while Hori’s nevus was located mainly on the malar area. The characteristics of the patients were shown in Table 1.
Dermatoscopic findings. The dermatoscopic features between melasma and Hori’s nevus were summarized in Table 2. Regarding colors, there was a significantly higher percentage of light brown color in melasma. This color was observed in 98 percent of patients with melasma and 10% of those with Hori’s nevus (P<0.001, Figure. 1A). A dark brown color was seen in both groups without any significant difference (P=0.117). On the other hand, blue-brown or gray color was found only in Hori’s nevus in 63 percent of patients (P<0.001, Figure 2A).
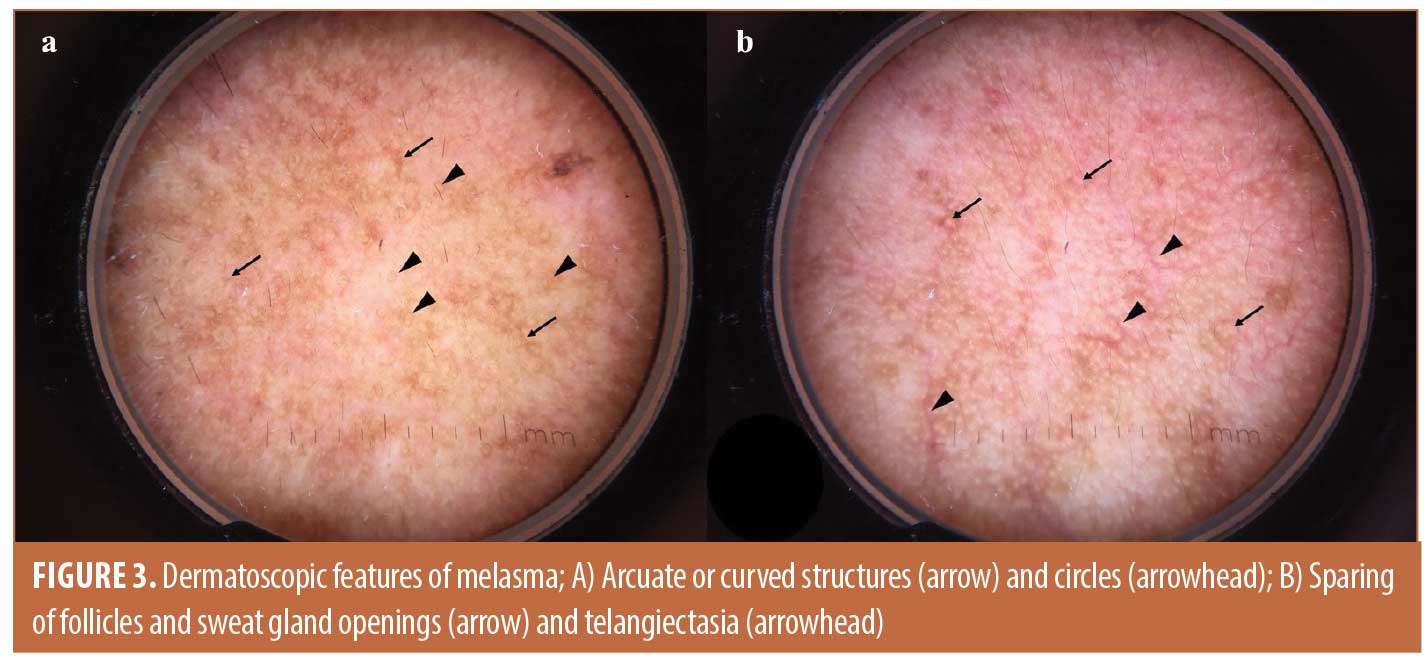
In terms of morphological patterns, certain morphology which was substantially more common in melasma (P<0.001). These include an irregular pigment network which accounts for 98% (Figure 1A), regular pigment network which was detected in up to 38 percent (Figure 1B), arcuate structure which was found in 68% and circles which were seen in 48 percent of patients (Figure 3a). However, the speckled homogenous pattern was exclusively found in Hori’s nevus, with a prevalence of 52% (P< 0.001, Figure 2b).
Regarding the other features, sparing of the follicles and sweat gland openings was significantly more common in melasma than Hori’s nevus (98% vs. 4.3%, P<0.001). In addition, telangiectasias were significantly more common in melasma than Hori’s nevus (52% vs. 19.6%, P=0.001, Figure 3b).
Discussion
Although melasma and Hori’s nevus are usually diagnosed clinically, sometimes coexistence of both conditions in the same area can be challenging for dermatologists to make the diagnosis. In general, dermatoscopy is a noninvasive technique to evaluate pigmented cutaneous lesions. Our study demonstrated that it is helpful in visualizing some patterns to differentiate melasma from Hori’s nevus, leading to a proper management which is different in the two conditions.
Dermatoscopy should help in distinguishing the types of melasma in clinical practice because it is a better tool for determining the depth of pigmentation and identifying the pigment network and vasculature patterns, compared to Wood’s lamp.7 Melasma can be classified based on the depth of melanin in the layers of skin into epidermal, dermal, and mixed-type melasma. Based on previous studies of dermatoscopic changes in melasma, dark brown and well-defined or regular network indicates melanin in the upper epidermis, while light brown and irregular network suggests melanin in the lower epidermis or papillary dermis.8 It is assumed that epidermal melasma reveals brown color variations and regular or irregular pigment network clinically. However, sparing of the follicles, pseudonetwork, and bluish-gray color most likely signify melanin in the mid- to deep dermis which could be found in dermal melasma.7,8 Accordingly, mixed-type melasma should bear the dermatoscopic features of both epidermal and dermal melasma.
Our study found that regular pigment network was presented in 38 percent of melasma patients, which is consistent with previous studies by Tamler et al8 and Manjunath et al7 that reported a prevalence of 40 percent and 36 percent, respectively. However, the color of the irregular network in our study was mostly light brown in 60 percent of melasma patients, whereas the predominant color in previous Indian studies was bluish gray, as shown by the bluish-gray pigment found in 46 percent of melasma patients.7,8 This discrepancy in color may be explained by the difference in melanosome size and density of melanin between different ethnic groups. The majority of our patients had FPT III which is associated with smaller melanosome sizes and less melanin in the dermis than the Indian population. In terms of the sparing of follicles and sweat gland openings, our study showed a prevalence of 98 percent in melasma, which is similar to that reported in a previous study by Yalamanchili et al.9 This could be explained by histopathology of melasma which reveals melanin and/or melanophages in the upper to mid-dermis without follicular or sweat gland involvement. In addition, melanin and/or melanophages may also disperse in the deep dermis with minimal perivascular lymphocytic infiltrate in the superficial dermis.12
On the other hand, dermatoscopic features in Hori’s nevus have not been reported. As Hori’s nevus and nevus of Ota are both diseases of misplaced dermal melanocytes, we hypothesize that they share some common features in dermatoscopy. According to a study by El Jouari et al,13 nevus of Ota shows a homogenous pigment pattern with a bluish-gray color. Similarly, in our study, we found that Hori’s nevus also frequently shows blue-brown or gray color, accounting for 63 percent of patients. It seems that the color in Hori’s nevus was lighter than that found in nevus of Ota. It is possible that the melanocytes in Hori’s nevus are situated more superficially, with a lower density of melanocytes in the papillary and mid-dermis compared to melanocytes in nevus of Ota which are located diffusely throughout the papillary and reticular dermis.14 Moreover, we reported that a speckled homogenous pattern is seen in 52 percent of Hori’s nevus patients. A possible explanation of this pattern is the late reactivation and aggregation of misplaced dermal melanocytes, which could be a consequence of their transfer from the basal layer of epidermis and abnormal migration during embryological development. Furthermore, the misplaced dermal melanocytes could also migrate from the follicular bulb.15 This would lead to the homogenous pattern without sparing of follicular and sweat gland openings in Hori’s nevus. In our study, sparing of the follicles and sweat gland openings was found in only four percent of patients with Hori’s nevus compared with in 98 percent of patients with melasma.
Telangiectasias have been demonstrated to be a characteristic feature of melasma due to ultraviolet-induced upregulation of vascular endothelial growth factor (VEGF), which is linked with melanogenesis in melasma.15 In our study, telangiectasias were significantly more common in melasma (52%) than in Hori’s nevus (19%). The association between melasma and telangiectasias is a controversial issue due to the possible confounding effects from such factors as photodamage, side effects of topical treatments, and differences in ethnic background which can predispose melasma patients to telangiectasias. According to a study by Kim et al, the increased angiogenesis of dermal blood vessels is a crucial pathogenesis in melasma.16 Without inattention that previous sun exposure and use of topical agents such as corticosteroids and hydroquinone would lead to erythema and telangiectasias, these studies reported that VEGF was expressed more prominently in the lesion of melasma than perilesional normal skin. It is acknowledged that VEGF would be not only a potential regulator in the new vascular formation in melasma, but it might stimulate melanogenesis in melasma lesions and hyperpigmentation in the epidermis.16,17
To our knowledge, the present study is the first to report the comparison of dermatoscopic features between melasma and Hori’s nevus in Asian patients. There are some differences in the dermatoscopic features of both conditions. Therefore, we propose the diagnostic clues for melasma and Hori’s nevus in Asian patients based on their significant differences in dermatoscopic findings and high inter-rater reliability scores which reflect the strong agreement between the two dermatologists in the dermatoscopic interpretation (Table 3). The light brown, regular and/or irregular pigment network, and sparing of follicles and sweat gland openings are useful diagnostic clues for melasma in Asian patients. In contrast, the speckled homogenous pattern without sparing of follicles and sweat gland openings is a favorable diagnostic clue for Hori’s nevus.
Limitations. The limitations of our study are the small sample size and lack of definitive histopathological diagnosis. However, performing skin biopsy in every patient would be impractical due to the risk for scarring, which could cause even further cosmetic concerns since melasma and Hori’s nevus mainly affect the face. Therefore, clinical diagnosis had to be relied upon in our study.
Conclusion
Our study describes the dermatoscopic features of melasma and Hori’s nevus in Asian patients. It is important to identify the dermatoscopic patterns as well as to establish the diagnosis of melasma or Hori’s nevus since they require different types of treatment, which have to be combined if the two conditions coexist.
References
- Ogbechie-Godec OA, Elbuluk N. Melasma: an Up-to-Date Comprehensive Review. Dermatol Ther (Heidelb). 2017;7(3):305-318.
- Vachiramon V, Suchonwanit P, Thadanipon K. Melasma in men. J Cosmet Dermatol. 2012;11(2):151-157.
- Ee HL, Wong HC, Goh CL, Ang P. Characteristics of Hori naevus: a prospective analysis. Br J Dermatol. 2006;154(1):50-53.
- Park JM, Tsao H, Tsao S. Acquired bilateral nevus of Ota-like macules (Hori nevus): etiologic and therapeutic considerations. J Am Acad Dermatol. 2009;61(1):88-93.
- McKesey J, Tovar-Garza A, Pandya AG. Melasma Treatment: An Evidence-Based Review. Am J Clin Dermatol. 2020;21(2):173-225.
- Kaur H, Sarma P, Kaur S, et al. Therapeutic options for management of Hori’s nevus: A systematic review. Dermatol Ther. 2020;33(1):e13167.
- Manjunath KG, Kiran C, Sonakshi S, Agrawal R. Melasma: Through the eye of a dermoscope. Int. J. Res. Dermatol. 2016;2(4):113-117.
- Tamler C, Fonseca RMR, Pereira FBC, Barcauí CB. Classification of melasma by dermoscopy: Comparative study with Wood’s lamp. Surg Cosmet Dermatol. 2009;1(3): 115-119.
- Yalamanchili R, Shastry V, Betkerur J. Clinico-epidemiological Study and Quality of Life Assessment in Melasma. Indian J. dermatol. 2015;60(5):519
- Tamega Ade A, Miot LD, Bonfietti C, et al. Clinical patterns and epidemiological characteristics of facial melasma in Brazilian women. J Eur Acad Dermatol Venereol. 2013;27(2):151–156
- Hori Y, Kawashima M, Oohara K, Kukita A. Acquired bilateral nevus of Ota-like macules. J Am Acad Dermatol 1984;10(6):961–964.
- Sanchez NP, Pathak MA, Sato S., et al. Melasma: a clinical, light microscopic, ultrastructural, and immunofluorescence study. J. Am. Acad Dermatol. 1981;4(6):698-710.
- El Jouari O, Senhaji G, Elloudi S, et al. Nevus of Ota. Madridge J Dermatol Res. 2018; 3(2):77-78.
- Hidano A, Kaneko K. Acquired dermal melanocytosis of the face and extremities. Br. J. Dermatol. 1991;124(1):96-99.
- Kim EJ, Park HY, Yaar M, et al. Modulation of vascular endothelial growth factor receptors in melanocytes. Exp dermatol. 2005;14(8):625-633.
- Kim EH, Kim YC, Lee ES, Kang HY. The vascular characteristics of melasma. J Dermatol Sci. 2007;46(2):111-116.
- Rendon MI, Benitez AL, Gaviria JI. Telangiectatic Melasma: A New Entity? J. Cosmet Dermatol. 2007;20(3):17-21.

