 J Clin Aesthet Dermatol. 2022;15(3):22–25.
J Clin Aesthet Dermatol. 2022;15(3):22–25.
by Domenico Piccolo, MD; Dimitra Kostaki, MD; Caterina Dianzani, MD, PhD; Giuliana Crisman, MD; and Claudio Conforti, MD
Drs. Piccolo, Kostaki, and Crisman are with the Skin Centers in Avezzano-Pescara, Italy. Dr. Conforti is with the Dermatology Clinic of Hospital Maggiore at the University of Trieste in Trieste, Italy. Dr. Dianzani is with the Plastic and Reconstructive Surgery Department at Campus Biomedico University in Rome, Italy.
FUNDING: No funding was provided for this article
DISCLOSURES: The authors report no conflicts of interest relevant to the content of this article.
ABSTRACT: Background. Acne is defined as a chronic inflammatory disease of the pilosebaceous units, mainly affecting the face of young adults, but the chest and back can be involved as well. Oral antibiotics, topical retinoids, azelaic acid, benzoyl peroxide, and isotretinoin represent the most common treatment used for the treatment of acne, but several adverse effects and a lack of durable remission, with poor adherence by the patients, have been reported thus far. Lasers have been shown to be effective and safe to treat acne; intense pulsed light (IPL) demonstrates high efficacy rates, minimal discomfort, rapid recovery times, and excellent cosmetic and therapeutic outcomes.
Objective. In this prospective study, we assessed the efficacy, safety, and reproducibility of a novel IPL protocol as a monotherapy in the treatment of acne of the chest and back.
Methods. We included patients (N=50) aged 14 to 30 who presented with moderate papulopustular acne sited on the chest and back (Cook’s Acne Grading Scale method 4–6, Pillsbury Scale III–IV). We performed four IPL sessions at two-week intervals on each patient.
Results: An excellent outcome was achieved in 50 percent of the patients and a good outcome in the 35 percent of the patients. Patients experienced light erythema and mild burning as the most common side effects, which spontaneously resolved within 24 to 96 hours.
Conclusion. Consistent with previous reports, our study demonstrated IPL to be a safe and effective treatment for severe cases of acne on the chest and back, providing excellent aesthetic and therapeutic results in 85 percent of treated patients.
Keywords: Papulopustular acne vulgaris, acne, chest, back, intense pulsed light, IPL
Acne vulgaris (AV) is an inflammatory disorder of the sebaceous glands of some areas (e.g., face, trunk, buttocks) that onsets most frequently during adolescence and is clinically characterized by comedones (comedonal acne), papulopustules (papulopustular acne) or nodules and cysts (nodulocystic acne or acne conglobata).1 All forms can result in punctiform, depressed or hypertrophic scars, with considerable psycho-emotional stress on the patient. Acne affects up to 85 percent of young people, with an average age between 14 and 19 years in males and between 10 and 17 years in females.2, 3 Although AV has long been considered a disease of puberty, it has been increasingly observed in pre- and post-adolescents as well.4 A lower incidence in individuals of Asian and African descent has been described.5 The etiopathogenesis of acne is multifactorial and it involves the role of androgens, keratinization, the infection of Cutibacterium acnes, and family history.5
Even if AV is not a devastating or life-threatening condition, it is significantly associated with social impairment, diminished quality of life, depression, anxiety, anger, and poor self-esteem.6 Given the negative psychological impact of AV, early initiation of effective therapy is recommended, especially in the inflammatory variety of AV. The aim of AV treatment is to reduce and control the progression of acne lesions, reduce the risk of acne development and reduce the duration of the disease.7 The choice of therapy depends on several factors, such as the age of patients, site, type and severity of acne, side effects, costs, and treatment availability. Combined treatments also can lead to excellent results in complex cases.
The most frequent combination therapies are based on the combination of oral antibiotic therapy, chemical peels, and the recourse to camouflage with variable grades of resolution and/or satisfaction. Oral antibiotics, topical retinoids, azelaic acid, benzoyl peroxide, and isotretinoin represent the most common treatments used to treat patients with acne, though adverse effects and a lack of durable remission, with a subsequent poor treatment adherence, have been reported.8–11 Some therapies for AV can cause skin inflammation, burning, or itching, leading to treatment interruption by patients.12
Lasers have been demonstrated to be a viable alternative for these acne treatments. The 1064-nm Nd:YAG laser and intense pulsed light (IPL) have been investigated in the past few years and both therapies demonstrate excellent cosmetic and therapeutic outcomes. Based on the variability in frequency and power usage of these technologies, IPL is a useful laser in the treatment of acne, since its flexibility can achieve notable improvements within the context of the variable inflammatory and non-inflammatory clinical presentation of acne.13–15
In this prospective study, we assessed the efficacy, safety, and reproducibility of a novel IPL protocol as a monotherapy in the treatment of acne of the chest and back.
Methods
Fifty patients ranging from 18 to 40 years of age (mean age 23.8 years old) with Fitzpatrick Skin Types II to III and moderate papulopustular acne on chest and back were retrospectively enrolled from our private practice centers. Written informed consent for participation in this study was obtained from all patients prior to enrollment. Patients were enrolled according to the Cook’s Acne Grading Scale method (inclusion criterion: Cook’s grading 4–6) and according to the Pillsbury Scale (inclusion criterion: Pillsbury Scale III–IV).
Thirty-two of 50 patients (64%) presented with a history of conventional topical and systemic acne treatments with antibiotics and isotretinoin without achieving a remarkable improvement. Each patient signed an informed consent before starting treatment. Exclusion criteria included a history of systemic retinoid use within six months prior to treatment, history of antibiotics within one month of treatment and use of topical antiacne treatment within three weeks prior to enrollment, along with a history of photodermatosis or photosensitizing reactions or any ongoing condition that could interfere with the evaluations. Pregnant and/or breastfeeding patients were also excluded. During the study, patients did not undergo any other systemic, topical, or another light-based acne treatment.
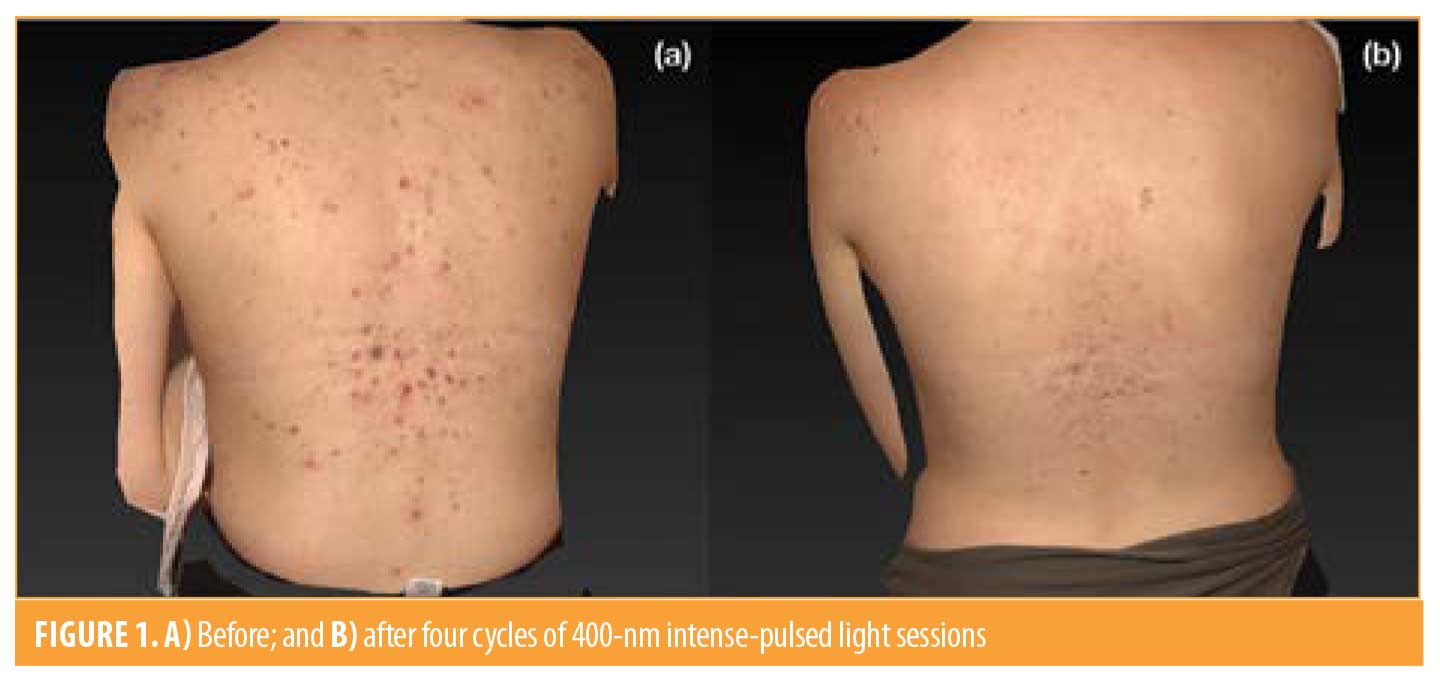
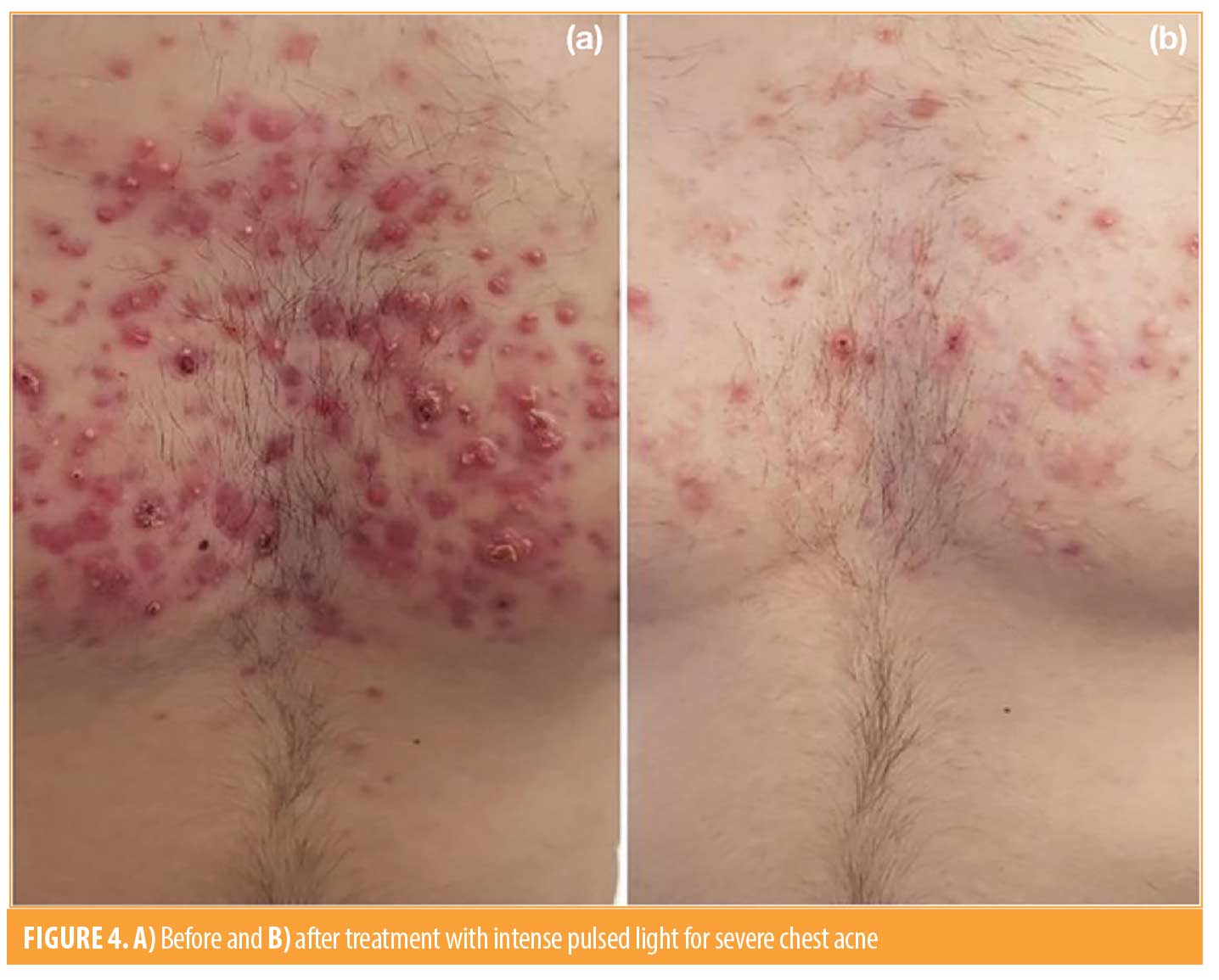
We used an IPL hand piece (Luxea Lazur hand piece, DEKA M.E.L.A. S.r.l., Calenzano, Italy) adjusted with the following parameters: cut-off wavelength, 400nm; fluence, 8–9J/cm2; single-pulse mode of 30ms duration; cooling of the hand piece and interposition of gel between skin and hand piece was used to avoid heating and skin burn; each area was treated only once per session. The protocol used was four sessions, each after a two-week interval. After each session, sunscreen and gentle cleansing were prescribed.
Patients subsequently underwent a clinical evaluation of the results based on clinical pictures (Cook and Pillsbury scales) before and after each session, and patient self-perception was evaluated. Patients came to follow-up every two-weeks for five weeks and were globally evaluated and subsequently classified via photographic records into five categories: G-I=Excellent Outcome (90% reduction of papules and pustules); G-II=Marked Improvement (89-60% reduction of inflammatory lesions); G-III=Partial Response (59–30% reduction); G-IV=Poor Response (<30% reduction); and G-V=No response (no changes or worsening in number of inflammatory acne lesions). Any side effects, such as erythema, hyperpigmentation, or scarring were also evaluated before each new session and, if present, they were recorded. Patient subjective responses were obtained at each visit using questionnaires that ranked degree of satisfaction from 0 (very unsatisfied) to 10 (highly satisfied).


Results
After the first session, Excellent Outcome (G-I) was achieved in 13/50 patients (26%) and 25/50 patients (50%) achieved category G-II. By the fifth session, an Excellent Outcome was achieved by the 50 percent of the patients (25/50) and a Marked Improvement was achieved by the 35 percent of the patients (18/50). No statistical difference was observed among age or sex of patients. Four patients (8%) demonstrated a partial response with a reduction of the inflammatory component without any improvement of the papulopustular lesions. Two patients (4%) showed no response since their clinical presentation remained substantially stable. Interestingly, one patient (2%) presented at the final follow-up visit with a worsening of her clinical conditions. Ninety-six percent (48/50) of treated patients improved at the end of the fourth session without side effects. Considering this, IPL seems to be faster in achieving results when compared to a conventional systemic and antibiotic therapy alone.
The most frequently reported side effects were erythema and burning which resolved within 96 hours of treatment. Pain, on the other hand, was reported in most cases as mild or moderate within three minutes after the end of the session.
Patients satisfaction scores increased from 0 at baseline to 3.5 after two sessions and 7.3 at one month after final treatment sessions. Our results have been summarized in Table 1.
Discussion
Acne vulgaris represents a common inflammatory condition of the pilosebaceous areas, especially in adolescents and young adults. The tendency of the pathology to relapse, cause hyperpigmentation or scarring can cause considerable psychological stress; for this reason, in addition to topical or systemic therapies, many treatments have been studied in recent years, especially to cope with cases that do not respond to common therapies.
According to the literature, a great interest has been shown in the investigations of lasers as new therapeutic tools in the treatment of acne. From 1,064 Nd:YAG lasers to blue or blue-red lights devices, from infrared (IR) lasers to PDT and IPL; clinicians all over the world assessed several comparative studies in the aim to achieve the most effective, safe and economically sustainable treatment in such a challenging dermatological condition. While blue light has also shown an important anti-inflammatory effect on keratinocytes,14–16 infrared (IR) lasers (1320, 1450, 1540 nm) and photodynamic therapy (PDT) are able to cause direct phototoxic damage to sebaceous glands, reducing the density of the glands and their sebum production.10
To date, twenty-six comparative studies regarding the efficacy of IPL in the treatment of acne have been published, highlighting the effectiveness and the safety of these devices in both inflammatory and non-inflammatory component of clinical presentations of acne vulgaris. Mohammed et al17 tested 1,064-nm Nd:YAG laser and IPL simultaneously on 74 patients, treating one cheek of each patient with IPL and the other cheek with 1,064-nm Nd:YAG laser. Their results showed a 70.2-percent reduction of the inflammatory acne lesions achieved by the 1,064-nm Nd:YAG versus 67.1 percent IPL treated side (p<0.05 for each), and a 19.3 percent reduction of non-inflammatory acne lesions obtained with the 1,064-nm Nd:YAG versus 18.3 percent IPL treated side (p>0.05 for each).
In addition, IPL might damage blood vessels supplying sebaceous glands, thus reducing sebaceous gland size and/or function.15–18 In our study, we observed a reduction in oiliness of the skin of our patients with improvement in skin tone and texture.
IPL also corrects the dilatation of vessels, resulting in reduction of erythema in inflammatory acne.19,20 In our study, our patients demonstrated a significant reduction of erythema after two sessions of treatment.
IPL, moreover, has been shown in in-vitro studies to induce collagen and elastic fiber synthesis in the dermis.21 This action reduces scar formation and our results confirm this evidence as the acne lesions in our study healed without scar formation.
Conclusion
Based on the possibility of using different combinations of wavelength, pulse duration, delay and fluency, IPL represents a good tool in the treatment of acne, since its flexibility could achieve important improvements within the context of the variable inflammatory and non-inflammatory clinical presentation of acne. The antibacterial and anti-inflammatory effects of IPL result in a reduction of lesion count and prevention on the formation of new lesions.
Consistent with previous reports, our study demonstrated IPL to be a safe and effective treatment for severe cases of acne on the chest and back, providing excellent aesthetic and therapeutic results in 85 percent of treated patients, whereas only 10 percent of the patients saw no improvement and the remnant five percent showed a slight worsening.
References
- Thiboutot DM, Strauss JS (2013) Diseases of The Sebaceous Glands. In : Freedberg IM, et.al. Fitzpatrick`s Dermatology in General Medicine.12th.ed. New York : McGraw-Hill Inc 672-686.
- Bhate K, Williams HC. Epidemiology of acne vulgaris. Br J Dermatol 2013 Mar;168(3): 474–485.
- Tan JK, Bhate K. A global perspective on the epidemiology of acne. Br J Dermatol. 2015 Jul;172 Suppl 1:3–12.
- Goldberg JL, Dabade TS, Davis SA, Feldman SR, Krowchuk DP, Fleischer AB. Changing age of acne vulgaris visits: another sign of earlier puberty? Pediatr Dermatol. 2011 Nov-Dec;28(6):645-8.
- Kurokawa I, et al. 2009. New developments in our understanding of acne pathogenesis and treatment. Exp. Dermatol. 18:821–832.
- Dunn LK, O’Neill JL, Feldman SR. Acne in adolescents: quality of life, self-esteem, mood, and psychological disorders. Dermatol Online J. 2011 Jan 15;17(1):1.
- Fox L, Csongradi C, Aucamp M, du Plessis J, Gerber M.Treatment Modalities for Acne. Molecules 2016;21(8):1063.
- Zaenglein AL, Pathy AL, Schlosser BJ, Alikhan A, Baldwin HE, Berson DS, et al. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol 2016;74(5):945-73.e33.
- Katsambas A, Papakonstantinou A. Acne: systemic treatment. Clin Dermatol. 2004 Sep-Oct;22(5):412-8.
- Thiboutot D, Gollnick H, Bettoli V, Dreno B, Kang S, Leyden JJ, et al. Global Alliance to Improve Outcomes in Acne. New insights into the management of acne: An update from the Global Alliance to Improve Outcomes in Acne Group. J Am Acad Dermatol. 2009;60(Suppl):S1–50.
- Thiboutot D, Dréno B, Sanders V, Rueda MJ, Gollnick H. Changes in the management of acne: 2009-2019. J Am Acad Dermatol. 2020 May;82(5):1268-1269.
- Barbaric J, Abbott R, Posadzki P, Car M, Gunn LH, Layton AM, Majeed A, Car J. Light therapies for acne. Cochrane Database Syst Rev. 2016 Sep 27;9(9):CD007917.
- Elman M, Lebzelter J. Light therapy in the treatment of acne vulgaris. Dermatol Surg. 2004;30:139–46.
- Mohanan S, Parveen B, Annie Malathy P, Gomathi N. Use of intense pulse light for acne vulgaris in Indian skin–a case series. Int J Dermatol. 2012 Apr;51(4):473-6.
- Patidar MV, Deshmukh AR, Khedkar MY. Efficacy of Intense Pulsed Light Therapy in the Treatment of Facial Acne Vulgaris. Indian J Dermatol. 2016 Sep-Oct;61(5):545-9.
- Shnitkind E, Yaping E, Geen S, Shalita AR, Lee WL. Anti-inflammatory properties of narrow-band blue light. J Drugs Dermatol. 2006;5:605–10.
- Mohamed EE, Tawfik K, Elsaie M. Intense Pulsed Light Versus 1,064 Long-Pulsed Neodymium: Yttrium-Aluminum-Garnet Laser in the Treatment of Facial Acne Vulgaris. J Clin Diagn Res. 2016 Jul;10(7):WC01-3.
- Pei S, Inamadar AC, Adya KA, Tsoukas MM. Light-based therapies in acne treatment Indian Dermatol Online J. May-Jun 2015;6(3):145-57. doi: 10.4103/2229-5178.156379.
- Liu J, Liu J, Ren Y, Li B, Lu S. Comparative efficacy of intense pulsed light for different erythema associated with rosacea. J Cosmet Laser Ther. 2014 Dec;16(6):324-7.
- Chen S, et al. Efficacy and safety of intense pulsed light in the treatment of inflammatory acne vulgaris with a novel filter. J Cosmet Laser Ther. 2019.
- Cuerda-Galindo E, Díaz-Gil G, Palomar-Gallego MA, Linares-GarcíaValdecasas R. Intense pulsed light induces synthesis of dermal extracellular proteins in vitro. Lasers Med Sci. 2015 Sep;30(7):1931-9.

