 J Clin Aesthet Dermatol. 2021;14(4):36–37.
J Clin Aesthet Dermatol. 2021;14(4):36–37.
by Nima Milani-Nejad, MD, PhD; Polina Rzepka, MD; Matthew J. Zirwas, MD; and Jessica Kaffenberger, MD
Drs. Milani-Nejad, Rzepka, and Zirwas are with the Division of Dermatology in the Department of Internal Medicine at The Ohio State University Wexner Medical Center in Columbus, Ohio. Dr. Kaffenberger is with The Ohio University College of Medicine in Columbus, Ohio.
FUNDING: No funding was provided for this article.
DISCLOSURES: Dr. Kaffenberger is a principal investigator for Amgen, Boehringer Ingelheim, Celgene, Corrona, Eli Lily, Janssen, Novartis, and Regeneron; and is a consultant with Boehringer Ingelheim. The other authors report no conflicts of interest relevant to the content of this article.
ABSTRACT: Bullous pemphigoid is an autoimmune condition whereby the immune system forms antibodies that target the skin, resulting in the formation of blisters in a generalized and symmetric pattern. Localized bullous pemphigoid can occur in special circumstances. Here, we describe two patients that developed localized bullous pemphigoid in one lower extremity following orthopedic surgery. We propose that underlying edema following orthopedic surgery is a potential trigger for localized bullous pemphigoid.
Keywords: Bullous pemphigoid, autoimmune disorder, blistering disorder, orthopedic surgery
Bullous pemphigoid (BP) typically presents in a symmetric and generalized distribution. Here, we describe two patients who presented with localized BP after orthopedic surgery.
Case Presentation
Case 1. A 68-year-old female patient with a history of generalized BP presented to our clinic with persistent blisters limited only to her left lower extremity. Previous pathological examination showed bulla with eosinophilic infiltrates with hematoxylin and eosin staining, linear immunoglobulin (Ig)G, and C3 deposition in the basement membrane with direct immunofluorescence, IgG deposition on the roof of salt split skin with indirect immunofluorescence, and elevated BP180 antibodies with enzyme-linked immunosorbent assay (ELISA), leading to a diagnosis of BP.
The patient was treated with several medications, including prednisone, mycophenolate mofetil, azathioprine, and rituximab, resulting in remission of her BP. She then underwent left ankle and foot surgeries. Subsequently, two months later, she experienced a recurrence of her BP, with large tense bullae and underlying 2+ pitting edema only on the left lower leg (Figure 1). She underwent a second course of rituximab with considerable improvement in her symptoms.

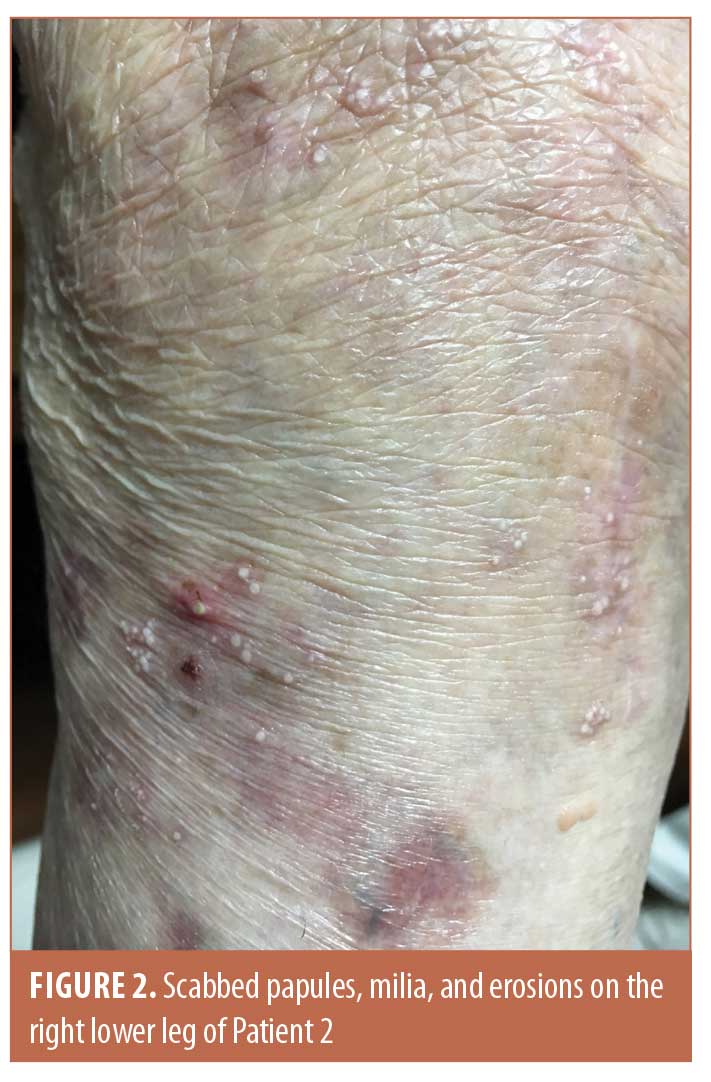
Case 2. A 75-year-old female patient with a history of right knee replacement presented with a three-year history of localized pruritic blisters on the right lower leg. By the time of our evaluation, she had scabbed papules, erosions, and milia limited to the lower right leg (Figure 2). ELISA confirmed BP180 antibody positivity. Biopsy showed subepidermal vesicular dermatitis with neutrophils and eosinophils on hematoxylin and eosin staining and linear IgG and C3 deposition in the basement membrane with direct immunofluorescence consistent with diagnosis of BP. She was treated with topical corticosteroids and oral doxycycline with resolution of her symptoms.
Discussion
The pathogenesis of BP is due to auto-antibodies targeting BP180 and BP230, two hemidesmosome components essential for the attachment of the epidermis to the underlying extracellular matrix, resulting in the formation of subepidermal blisters.1,2 Since these antigens are expressed throughout the skin, BP typically presents with a generalized and symmetric pattern.1
Localized BP has previously been described in the context of radiation, phototherapy, surgical sites, burns, and neurological hemiparesis.3 Proposed mechanisms of localized BP in this context include koebnerization, alteration of BP180 and BP230 antigens, and exposure of these antigens to the humoral mediated immunity. Neither of our patients had a history of radiation, burns, or neurologic insults to their affected extremities. Furthermore, the localized presentations in our patients were not due to koebnerization phenomenon since the blisters extended beyond the surgical sites.
One likely trigger is localized edema, a likely consequence of the orthopedic surgeries, which can explain the pathogenesis of localized BP in these cases. Studies suggest that up to seven percent of unaffected subjects have circulating BP180 and/or BP230 antibodies without any clinical manifestation.4,5 Furthermore, one study showed that such antibodies from unaffected subjects can activate immune cells in vitro.6 It is plausible that, in our patients, the edema and vascular congestion secondary to the orthopedic surgeries caused an increase in the local concentration of BP180 and/or BP230 antibodies, inflammatory mediators, and immune cells in the affected extremity, ultimately resulting in the formation of blisters limited to these sites. Interestingly, a recent report also described unilateral lower extremity BP in a patient with venous stasis,3 further highlighting the role of edema in certain cases of localized BP.
Conclusion
In summary, we describe two patients with localized presentations of BP associated with orthopedic surgery. The role of orthopedic surgery and localized edema as triggers of localized BP warrants further recognition and evaluation.
References
- Di Zenzo G, Della Torre R, Zambruno G, Borradori L. Bullous pemphigoid: from the clinic to the bench. Clin Dermatol. 2012;30(1):3–16.
- Milani-Nejad N, Zhang M, Kaffenberger J. The association between bullous pemphigoid and neurological disorders: a systematic review. Eur J Dermatol. 2017;27(5):472–481.
- Shi CR, Charrow A, Granter SR, Christakis A, Wei EX. Unilateral, localized bullous pemphigoid in a patient with chronic venous stasis. JAAD Case Rep. 2018;4(2):162–164.
- Wieland CN, Comfere NI, Gibson LE, Weaver AL, Krause PK, Murray JA. Anti-bullous pemphigoid 180 and 230 antibodies in a sample of unaffected subjects. Arch Dermatol. 2010;146(1):21–25.
- Wolz MM, Comfere NI, Gibson LE, Wieland CN. Anti-bullous pemphigoid 180 and 230 antibodies in asymptomatic subjects: five-year follow-up. J Am Acad Dermatol. 2013;68(4):686–687.
- Prussmann W, Prussmann J, Koga H, et al. Prevalence of pemphigus and pemphigoid autoantibodies in the general population. Orphanet J Rare Dis. 2015;10:63.

