 J Clin Aesthet Dermatol. 2020;13(9):49–51
J Clin Aesthet Dermatol. 2020;13(9):49–51
by Gabriella Vasile, DO; Mojgan Hosseinipour, DO; Cindy Hoffman, DO; and Charles Gropper, MD
Dr. Vasile is a Dermatology resident at Larkin Community Hospital of Palm Springs Dermatology in Hialeah, Florida. Dr. Hosseinipour is a Dermatology resident at St. Barnabas Hospital in Bronx, New York. Dr. Gropper is a Dermatologist at St. Barnabas Hospital in Bronx, New York.
FUNDING: No funding was provided for this study.
DISCLOSURES: The authors have no conflicts of interest relevant to the content of this article.
ABSTRACT: Corticosteroid injections are an effective treatment for many medical conditions. However, clinicians must be aware of potential side effects of this treatment modality so that proper patient counseling can take place. Patients with pigmentary alteration after intra-articular or intralesional corticosteroid injections have rarely been reported in literature. We present an adult male patient with linear depigmentation after an intralesional corticosteroid injection for a Morton’s neuroma.
Keywords: Depigmentation, corticosteroid injection, Morton’s neuroma, intralesional injection, lymphatic depigmentation, linear depigmentation, corticosteroid side effect
Extra-articular corticosteroid injections are commonly used to treat many dermatologic, orthopedic, and rheumatologic disorders, including keloids, hypertrophic scarring, acne, psoriasis, trigxger finger, Morton’s neuroma, and arthritis, and can be used to decrease inflammation of tendons and ligaments.1 Hypopigmentation or depigmentation of the skin, especially that in a linear fashion, has rarely been reported in literature as a possible side effect of corticosteroid injection, making this a unique entity. We present a case of linear depigmentation in a 55-year-old male following an intralesional corticosteroid injection for a Morton’s neuroma.
Case Report
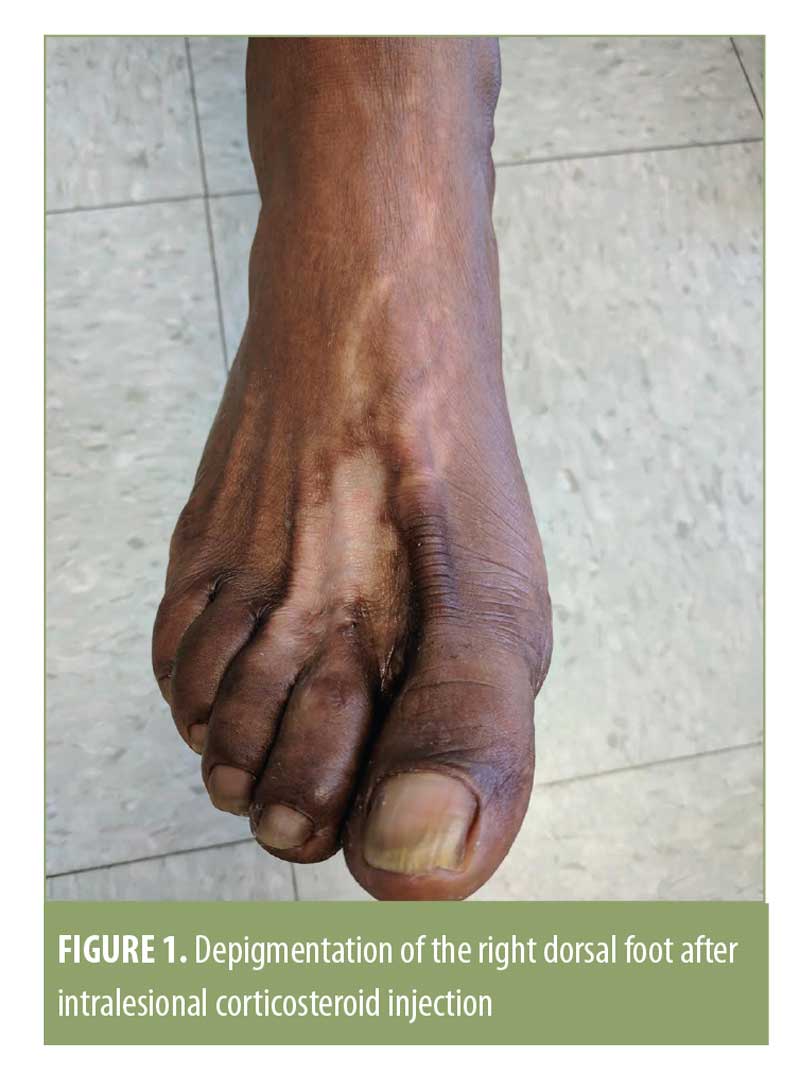
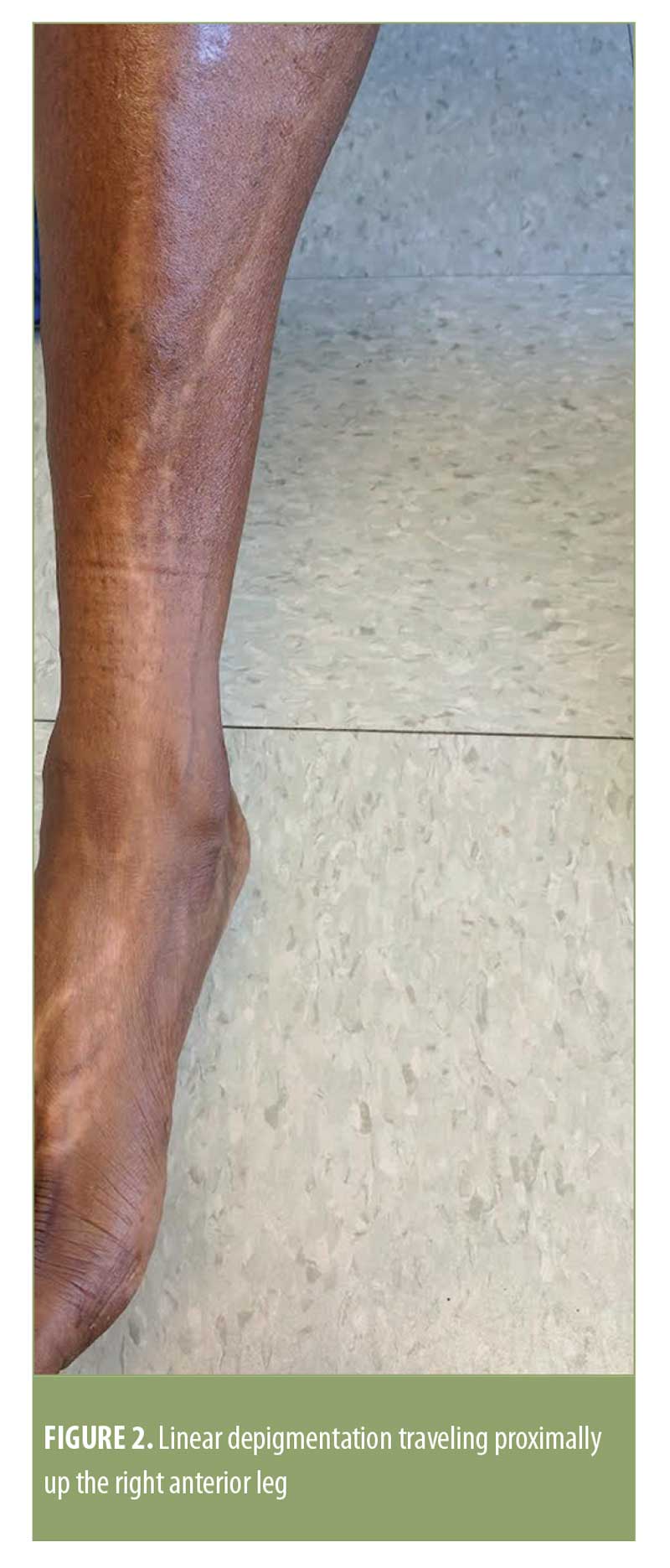
A 55-year-old African American male presented to our dermatology clinic with pigmentary alteration of the right lower extremity. The patient did not report any pertinent medical or surgical history, as well as any allergies or current medications. The patient’s physical exam was notable for a depigmented patch on the right dorsal foot with scattered surrounding depigmented macules and linear depigmentation extending proximally up the right anterior leg (Figures 1 and 2). The patient received an intralesional corticosteroid injection for a Morton’s neuroma four months prior to presentation. Wood’s lamp examination confirmed depigmentation. The patient was seen in the office four weeks later, with mild improvement of the depigmentation.
Discussion
Morton’s neuroma, also known as interdigital neuralgia, is a degenerative neuropathy affecting plantar digital nerves and is a common entity seen in middle-aged individuals.2 Because Morton’s
neuroma can be extremely painful and debilitating for patients, treatment is usually warranted. Intralesional injections of corticosteroids, anesthetics, and alcohol have been used to treat Morton’s neuroma not responsive to conservative measures. To avoid the complications of surgery, intrales
ional injections of triamcinolone are most commonly used.3,4
Intralesional corticosteroids tend to have a longer duration of action compared to topical or systemic corticosteroids and are therefore the preferred treatment modality for chronic conditions.5 Because intralesional corticosteroid injections are directed towards a localized area in the body, some of the major side effects caused by systemic corticosteroids, such as immunosuppression, allergic reactions, change in vision, hypertension, and adrenal suppression, can be avoided.6 However, localized corticosteroid injection has been shown to cause tendon rupture, cellulitis, osteomyelitis, atrophy, and hypopigmentation or depigmentation.1,7
The exact mechanism of depigmentation or hypopigmentation after an intralesional or intra-articular corticosteroid injection is unknown, but several theories exist.8 One thought is that the spread of corticosteroids after injection can lead to cutaneous atrophy and linear loss of pigment.9 The corticosteroid might travel via the lymphatics or vasculature, leading to linear depigmentation, as hypothesized by Gaglio de Grecco et al.10 It is also hypothesized that corticosteroids might lead to a decrease in the number of melanocytes or alter melanocyte function via cytokine or prostaglandin inhibition.11 In one case, a biopsy was performed at a site of linear depigmentation and the results showed normal skin with a normal number of melanocytes.12 Dhawan et al5 reported a case of linear leucoderma after intralesional triamcinolone injection for hypertrophic lichen planus in which a punch biopsy was performed on a depigmented area. The results of this biopsy on hematoxylin and eosin (H+E) stain also showed a normal number of melanocytes with decreased production of melanin.
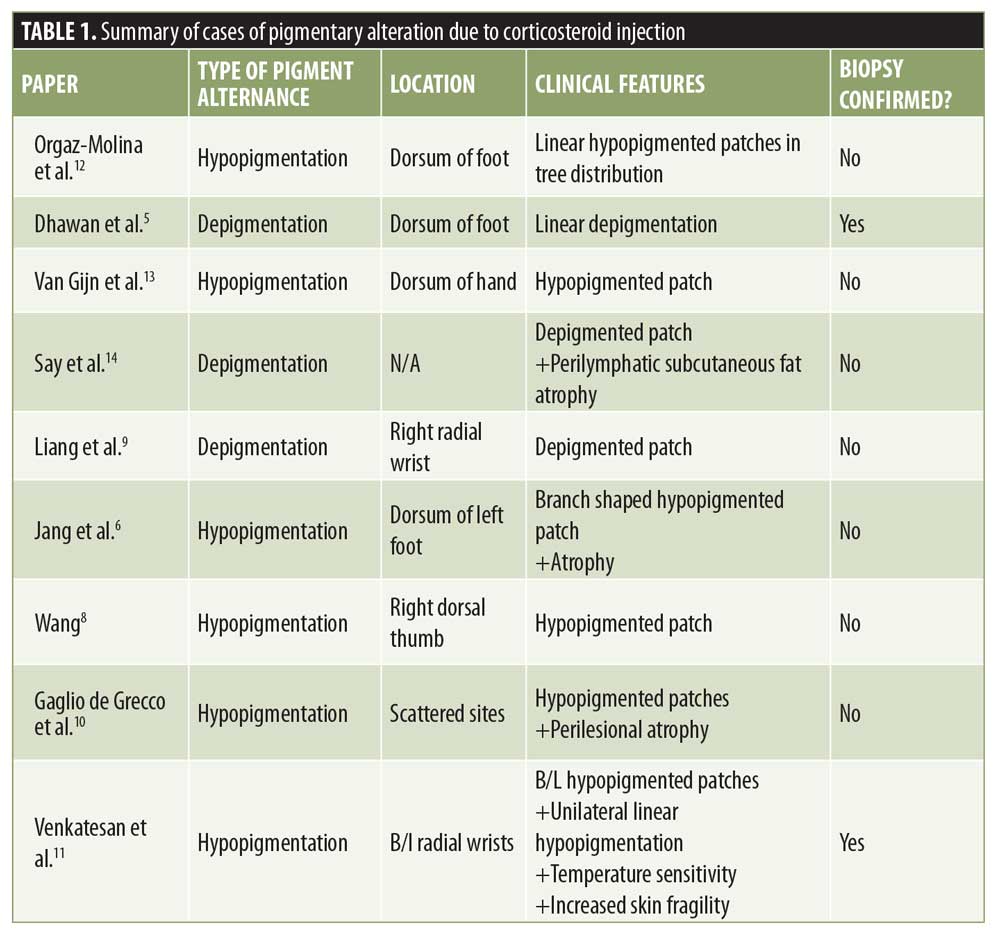
In our patient, both local and linear depigmentation were observed, versus hypopigmentation reported more commonly in other cases. Table 1 summarizes reported cases of pigmentary alteration secondary to local corticosteroid injection along with associated cutaneous findings. Differential diagnosis included linear leucoderma or segmental vitiligo, post-inflammatory hypopigmentation, tinea versicolor, and onchocerciasis. Although some cases report hypopigmentation in a linear distribution, Van Gijn13 reported a case of local hypopigmentation surrounding the site of injection. Say et al14 described a case of periocular depigmentation and fat atrophy after corticosteroid injection in a child.
Depigmentation following intralesional corticosteroid injections normally improves or resolves within one year.12 Therefore, treatment is usually not recommended. Several cases have been reported in which spontaneous repigmentation occurred without any treatment.9 Jang et al6 presented a case in which the patient did not have any significant improvement in pigmentation after 13 months. A majority of patients will see improvement in hypopigmentation; therefore, patient counseling and reassurance are important.
Cases of depigmentation of the skin following a corticosteroid injection are rare. Although there are many commonly seen adverse reactions to corticosteroid injections, it is important that clinicians are aware of this unusual side effect, which can be a cause of patient concern, especially in patients with darker skin types.5 Although this is a benign entity, the question exists whether or not there is an increased risk of depigmentation in patients of certain skin types or with higher concentrations of corticosteroid per injection. We report a case of depigmentation that likely spread in a vascular or lymphatic manner 3 to 4 months after an extra-articular steroid injection for a Morton’s neuroma. Due to the severity of side effects of such corticosteroid injections, clinicians must weigh the benefits versus risks before relying on this treatment modality. More studies are needed to understand the exact mechanism in which the hypopigmentation or depigmentation occurs and whether or not using lower doses of corticosteroid can prevent this side effect.
References
- Brinks A, Koes BW, Volkers A, et al. Adverse effects of extra-articular corticosteroid injections: a systemic review. BMC Musculoskelet. 2010;11:206.
- Valisena S, Petri GJ, Ferrero A. Treatment of morton’s neuroma: a systemic review. J Foot Ankle Surg. 2018; 24(4):271–281.
- Hughes RJ, Ali K, Jones K et al. Treatment of morton’s neuroma with alcohol injection under sonographic guidance: follow-up of 101 cases. AJR. 2007;188:1535–1539.
- Lizano-Diez X, Gines-Cespedosa A, Alentorn-Geli E et al. Corticosteroid injection for the treatment of morton’s neuroma: a prospective, double-blinded, randomized, placebo-controlled trial. Foot Ankle Int. 2017;39(9):944–951.
- Dhawan AK, Bisherwal K, Grover C et al. Linear leucoderma following intralesional steroid: a report of three cases. J Cutan Aesthet Surg. 2015;8:117–119.
- Jang WS, Park J, Yoo KH et al. Branch shaped cutaneous hypopigmentation and atrophy after intralesional triamcinolone injection. Ann Dermatol. 2011;23(1):111–114.
- Cohen PR. Cephalexin-associated Achilles Tendonitis: case report and review of drug-induced tendinopathy. Cureus. 2018;10(12):3783.
- Wang X. Hypopigmentation after local corticosteroid injection for de quervain tenosynovitis. Int J Res Dermatol. 2017;1:31–33.
- Liang J, McElroy K. Hypopigmentation after triamcinolone injection for de quervain tenosynovitis. Am J Phys Med Rehabil. 2013;13:639.
- Gaglio de Grecco MS, Cutillas-Marco E, Gimenez-Cortes ME et al. A rare complication from a common procedure. J Am Acad Dermat. 2011;64(2):AB145.
- Venkatesan P, Fangman WL: Linear hypopigmentation and cutaneous atrophy following intra-articular steroid injections for de quervain’s tendonitis. J Drugs Dermatol. 2009;8:492–493.
- Orgaz-Molina J, Naranjo-Sintes R, Arias-Santiago S. Linear hypopigmentation following vein path. J Am Acad Dermat. 2012;66(4):AB179.
- Van Gijn DR, Dunne JA, Fleming ANM. Hypopigmentation of the dorsum of the hand following steroid injection for trigger finger. J Plast Reconstr Aesthet Surg. 2017;11:26–27.
- Say EA, Shields CL, Biancotto C et al. Perilymphatic subcutaneous fat atrophy and cutaneous depigmentation after periocular triamcinolone acetonide injection in a child. J AAPOS. 2011;(15(1):107–108.

