J Clin Aesthet Dermatol. 2023;16(11):36–41.
J Clin Aesthet Dermatol. 2023;16(11):36–41.
by Ibrahim Fouda, MD; Asmaa Saad Shatta, MBBCH; and Zakaria Mahran Obaid, MD
Dr. Shatta is with Damietta Dermatology, Leprosy Hospital, and the Egyptian Ministry of Health and Population in Damietta, Egypt. Drs. Obaid and Fouda are with the Dermatology and Venereology and Andrology Department in the Damietta Faculty of Medicine at Al-Azhar University in Cairo, Egypt.
FUNDING: No funding was provided for this article.
DISCLOSURES: The authors report no conflicts of interest relevant to the content of this article.
ABSTRACT: Background. Acanthosis nigricans (AN) is a common chronic skin disorder clinically presenting as velvety, hyperpigmented lesions that can affect any part of the body, including the face.
Objective. We sought to evaluate and compare the efficacy and safety of fractional CO₂ laser and TCA 20% peel in the treatment of pseudo-acanthosis nigricans.
Methods. The current study adopted an experimental, comparative split-neck design. It included a total of 20 patients with bilateral pseudo-acanthosis nigricans of the neck. Each patient was subjected to four sessions, spaced three weeks apart, involving fractional CO₂ laser therapy on the right side and TCA 20% application on the left side. The evaluation of cases involved the utilization of the ANASI score and the assessment conducted by two dermatologists blinded to the treatment, both prior to and three months following the treatment.
Results. Regarding Clinical improvement, 20% of the Fractional CO₂ laser side had excellent improvement, and 45 percent had marked improvement. In contrast, the TCA 20% peel side had 2 percent marked improvement, 50 percent moderate improvement, and 40 percent mild improvement. In terms of response to therapy sessions, there was a statistically significant difference between the studied treatment sides (p<0.001). Regarding ANASI score differences between treated sides before and after treatment, a statistically significant reduction in ANASI score was observed, with a higher percentage of reduction in the Fractional CO₂ laser side compared to the TCA 20% peel side.
Limitations. The primary limitations are the small sample size and short follow-up period. Conclusion. In the treatment of pseudo-acanthosis nigricans, it appears that fractional CO₂ laser and TCA 20% are promising, effective, and well-tolerated modalities. However, the Fractional CO₂ laser was associated with a better response.
Keywords: Acanthosis Nigricans, Fractional CO₂ lasers, trichloroacetic acid, chemical peeling
Introduction
The term acanthosis nigricans (AN) was first described by Sigmund Pollitzer (1859-1937), Victor Janowsky (1847-1925), and Paul Gerson Unna (1850-1929) from Hamburg Germany in Unna’s eminent International Atlas of Rare Skin Diseases published in 1890.1
AN is a cutaneous disorder with multiple etiologies that typically manifests as hyperpigmented, dark, rough patches or plaques on the neck, elbows, knees, dorsal joints of the hands and fingers (knuckles), external genitalia, and flexures. In rare cases, the face and eyelids may also be affected.2
According to Curth, AN has numerous classifications, including malignant, benign inherited, pseudo-associated with obesity, and syndromic.3 Hernandez-Perez classified AN as simple (including nevoid/obesity-related/drug-related/syndromic) and paraneoplastic.4 Schwartz outlined eight categories of AN: (1) benign, (2) obesity-associated, (3) syndromic, (4) malignant, (5) acral, (6) unilateral, (7) medication-induced, and (8) mixed-type when two varieties are present.5
The most prevalent type is pseudo-acanthosis nigricans (obesity-associated AN). Even though it can occur at any age, it is more common in adults and is frequently associated with insulin resistance.6
A significant correlation has been found between AN and BMI (Body Mass Index), waist circumference, elevated blood pressure, dyslipidemia, hyperinsulinemia, hyperglycemia, impaired glucose intolerance, and insulin resistance, as measured by the HOMA-index in different age groups. This finding suggests that patients with AN are at an increased risk of developing metabolic syndrome (METS) and Type 2 diabetes.7
The prevalence of AN is currently increasing due to the rise in obesity and diabetes among the population. In the general population, prevalence ranges from 7 percent to 74 percent, depending on factors including age, race, AN type, level of obesity, and concomitant endocrine problems.8 Dark-skinned people are more likely to exhibit this symptom, with Native Americans and African Americans most frequently affected, followed by Hispanics, Asians, and significantly fewer Caucasians.9
Pathogenesis of AN is not fully understood. However, it is known that extensive AN with an early onset in childhood can be caused by mutations in the insulin receptor gene that result in insulin resistance. Additionally, severe AN phenotypes are associated with genetic mutations in the phosphatase and tensin homolog (PTEN), FGFR2, and FGFR3 genes 10.
In paraneoplastic AN, cancer cells in tumors and metastatic deposits secrete cytokines such as transforming growth factor-a (TGF-a), which can bind to EGFR in skin cells and cause hyperkeratosis and papillomatosis leading to AN.11
Drug-induced acanthosis nigricans is a rare subtype of acanthosis nigricans, which may be a side effect of numerous drugs, with nicotinic acid and insulin being the most likely drugs to induce AN.12
In general, the available treatments for AN are not entirely sufficient. There is a scarcity of well-controlled comparative studies that include long-term follow-up. Topical retinoids, such as tretinoin, tazarotene, and adapalene, exhibit a degree of efficacy. The efficacy of oral retinoids, including acitretin and isotretinoin, has been documented in the treatment of extensive disease. Additional topical agents, such as vitamin D analogs, ammonium lactate, trichloroacetic acid, triple-combination depigmentation cream, urea, and salicylic acid, have been suggested for use in treating the condition. However, further research is needed to confirm their effectiveness.13,14
Fractional CO₂ lasers incorporate the technique of fractionated photo-thermolysis, creating columns of micro-thermal zones in the skin. The adjacent unaffected follicular stem cells and surviving fibroblasts contribute to the rapid regeneration of the epidermis and collagen remodeling collagen in the afflicted skin, respectively.15
By removing just a few layers of skin with little thermal injury, a fractional laser for acanthosis Nigricans can enhance both pigmentary and textural alterations, causing a dermal wound and the production of new collagen.16
Trichloroacetic acid (TCA) is frequently utilized for the treatment of lentigo, acne vulgaris, fine wrinkles, scars, seborrheic and actinic keratosis, and hyperpigmentation.17,18.
Methods
The current study adopted an experimental, comparative split-neck study. A total of 20 patients with bilateral pseudo acanthosis nigricans of the neck were recruited from the Dermatology outpatient clinic at Al-Azhar University Hospital in Damietta. This study was conducted to compare the efficacy and safety of fractional CO₂ laser and TCA 20% peel in the treatment of AN. The right side of the neck was treated with fractional CO₂ laser, while the left side was treated with TCA 20% during four sessions separated by three weeks. The study was approved by an Ethics Committee of Damietta Faculty of Medicine IRB (00012367), Al-Azhar University, Egypt. All patients provided written informed consent.
Patient selection. The study included adult patients with Pseudo AN of varying degrees of severity. Patients with keloidal tendency, pregnant and lactating females, patients with systemic diseases such as connective tissue disease, skin infection, or any other disease that could affect the wound healing process, patients receiving immunosuppressive drugs, and patients who were sensitive to TCA were excluded from the study.
Patient evaluation. All patients provided a comprehensive medical history, including their names, ages, onset and duration, risk factors, potential causes, and propensity for scarring or keloid formation. General and dermatological examinations were performed to determine the severity of the disease, the skin type, and any associated skin diseases.
The right side was treated with a fractional laser, while the left side was treated with TCA 20%, and a total of four sessions were performed every three weeks.
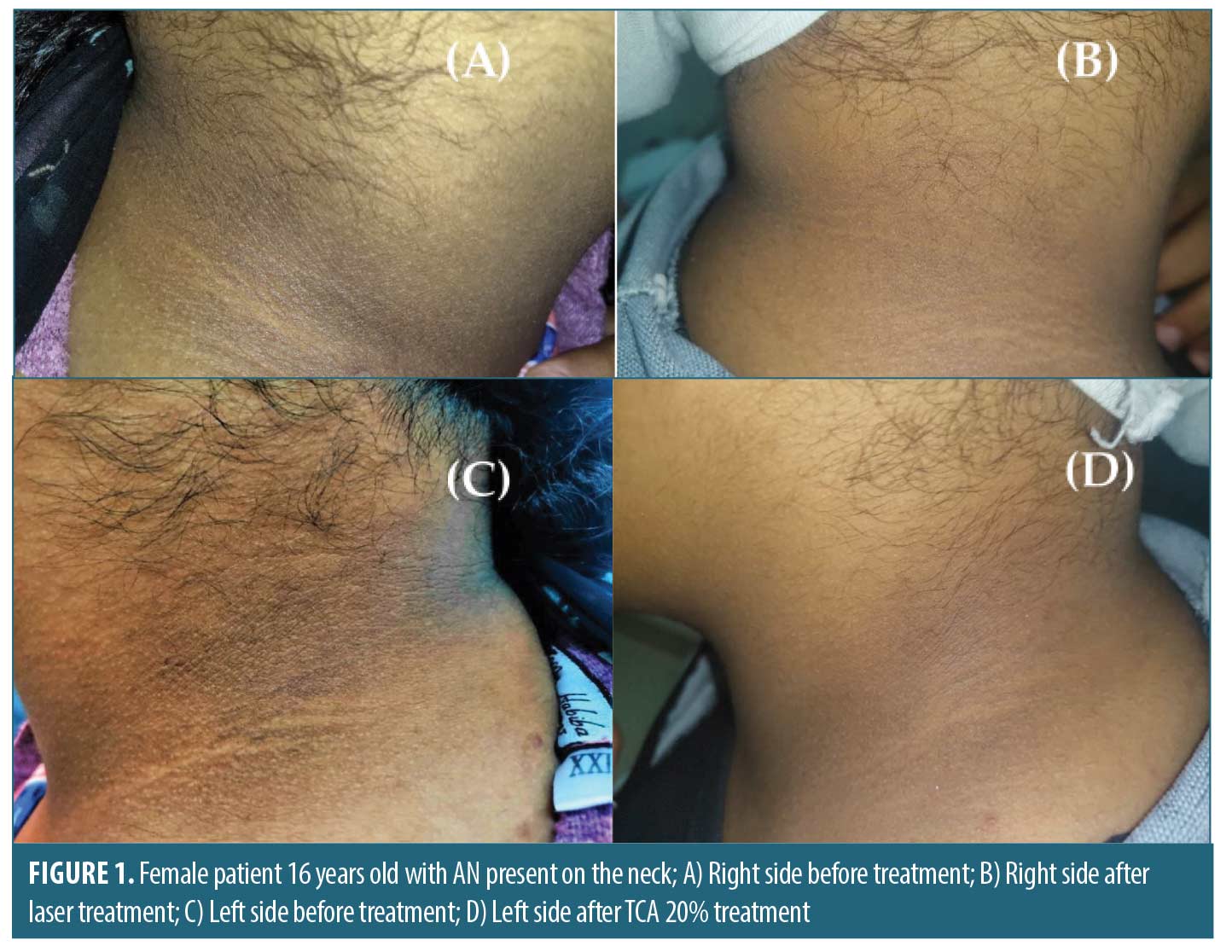
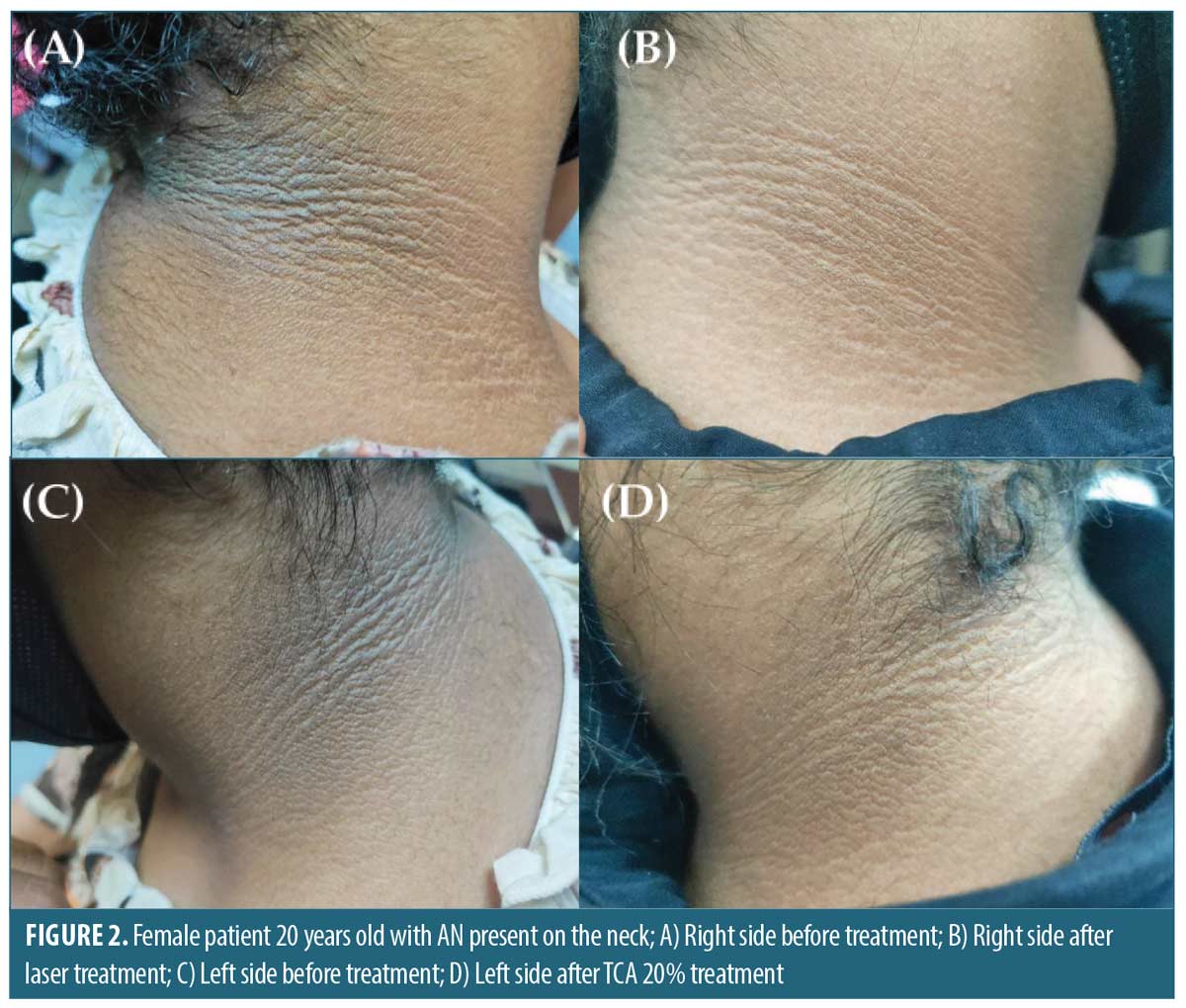
Disease severity was evaluated before and after treatment by two blinded dermatologists using a percentage of improvement (0=no improvement, mild=1%–25% improvement, moderate=26%–50% improvement, marked= 51%–75% improvement, and excellent=76%–100% improvement) and using ANASI score system. (Figure 1)
Digital photography was taken before, after the completion of the sessions, and at the conclusion of the sessions.
Treatment protocol. Laser side. A topical anesthetic cream (lidocaine 5%) was applied on the RT side of the neck for 60 minutes. A fractional CO₂ laser (DEKA Smartxide DOT C60) was used. The used laser parameters included power (10 w), dwell time (300 μs), spacing (300 μm), and double stacking with a single pass on the affected areas without overlapping.
Peeling side. The LT side of the neck was cleaned with alcohol-soaked gauze, and then TCA 20% peel was applied until white frosting formed.
Postoperative care. All patients were advised to apply a topical antibiotic with steroid cream and emollient twice daily for one week after the session and to avoid sun exposure.
Statistical analysis and data interpretation. Data were fed into the computer and analyzed using the IBM SPSS Statistics for Windows (Version 22.0., 2014, Armonk, NY: IBM Corp). Qualitative data were described using numbers and percentages. Quantitative data were described using median (minimum and maximum), mean, and standard deviation for parametric data after testing normality using the Kolmogrov-Smirnov test. The significance of the obtained results was judged at the (0.05) level.
Data analysis. Qualitative data. Chi-square and Monte Carlo tests were used to compare two or more groups, whereas the Friedman test was used to compare follow-up readings within the same injection side.
Results
The mean age of the patients studied was 22 years, with a range of 14 to 33 years (17 females and 3 males. Eight (40%) had mild disease, nine patients (45%) had moderate disease, and three cases (15%) had severe disease. The median duration of the disease was 4.5 years, ranging from 2 to 10 years. The mean ANASI score was 22, ranging from 12 to 40. In terms of skin type distribution, 10 percent of the cases studied were Skin Type V, 70 percent were Skin Type IV, and 20 percent were Skin Type III. In addition, 5 percent of the studied cases had an associated systemic disease, diabetes mellitus, and 5 percent had a positive family history of AN (Table 1).
In terms of clinical response, 20% of the Fractional CO₂ laser side showed excellent improvement, 45 percent showed marked improvement, and 35 percent showed moderate improvement. In contrast, 50 percent of the TCA 20% peel side showed moderate improvement, 40 percent showed mild improvement, and 2 percent showed marked improvement (Table 2).
Regarding Regarding ANASI score differences between treated sides before and after treatment, a statistically significant reduction in ANASI score was observed, with a greater percentage of reduction in the Fractional CO₂ laser side compared to the TCA 20% peel side (Table 3).
In terms of pain and erythema, the fractional CO₂ laser side had a statistically significant higher incidence of adverse effects than the TCA 20% peel side. However, there was no statistically significant difference between the two sides in terms of hyperpigmentation (Table 4).
Discussion
AN is a therapeutic challenge due to the absence of a standard treatment. Improvement of the skin lesions is often the patient’s primary concern. Changes in lifestyle, topical retinoids, depigmenting agents, and oral insulin sensitizers like metformin require long-term therapy with variable compliance and efficacy.19
Due to its capacity for superficial skin surface ablation with trans-epidermal melanin elimination, the fractional ablative carbon dioxide (CO₂) laser has emerged as a potential treatment.16 Furthermore, it has been demonstrated that chemical peels such as TCA, which exfoliate the epidermis and remove excess keratin and melanin, are effective in the treatment of AN.9
Wijnberg et al20 evaluated the use of fractional CO₂ laser in the treatment of AN in a 48-year-old male who had AN since puberty. After a one-year follow-up period, the resurfaced area showed complete healing with significant improvement, and there were no signs of recurrence.
In another study, Campos et al21 treated a 9-year-old child presenting with unilateral acanthosis nigricans. The treatment consisted of two cycles of pulsed CO₂ laser treatment , with a 2-month gap between sessions. They concluded that the patient’s final cosmetic outcome was relatively satisfactory.
Similarly, Leerapongnan et al22 compared fractional 1550-nm erbium fiber laser (three sessions) to topical tretinoin 0.05 for 12 weeks in 18 patients with AN on the neck. There was a more significant improvement in skin roughness and hyperpigmentation on the laser side, with no reported adverse effects. They determined that fractional erbium laser could be a viable alternative treatment for AN.
Elmasry et al. conducted another randomized-controlled split neck study on 23 patients suffering from AN. Each patient’s side of the neck was randomly assigned to fractional CO₂ laser versus Qs Nd: YAG and KTP laser treatments every four weeks for four months, followed by four monthly assessments. Both fractional CO₂ and Q-switched lasers were found to be safe and effective methods of treating AN.23
In the present study, there was a statistically significant difference in disease response to treatment between the fractional CO₂ laser and TCA 20% peel groups (p=0.001). Twenty percent showed excellent improvement, 45 percent showed marked improvement, and 35 percent showed moderate improvement on the fractional CO₂ laser side, compared to 50 percent moderate improvement and 40 percent mild improvement on the TCA 20% peel side.
Eldeep et al. revealed that both modalities (fractional CO₂ laser and TCA 20% peel) were influential in the treatment of pseudo-AN. However, the therapeutic response was significantly higher in the fractional CO₂ laser group than in the TCA 20% peel group (p<0.01). In addition, marked excellent response (51%–100% clearance of AN lesions) was achieved in 85 percent of the patients in the fractional laser group versus 10 percent of the patients in the TCA group.24
In contrast to Eldeep et al., our study was a split-neck comparative study, so each subject served as his or her own control. Because all interventions are measured on the same participants, this design minimizes the risk of confounding. Moreover, fewer patients are required than in parallel-group studies.
In contrast to our findings, Zaki et al., who compared the use of fractional CO₂ laser versus 70% glycolic acid peel in the treatment of pseudo-acanthosis nigricans. Their study concluded that glycolic acid peeling and fractional CO₂ laser are both effective in treating pseudoacanthosis nigricans. Glycolic acid peels 70% demonstrated superior results to fractional CO₂ laser due to accelerated exfoliation induced by the peel.25
The removal of excess keratin and melanin from the epidermis, as well as epidermal sloughing, is the precise mechanism by which TCA chemical peeling treats AN. TCA concentration affects the extent to which the epidermis undergoes coagulative necrosis.
In a pilot study by Zayed et al., which included six females with AN, the patients received four peeling sessions using TCA 15%. All patients showed improvement regarding hyperpigmentation, thickening, and overall appearance.26
These results were similar to those reported by Rajegowda et al., who investigated TCA 15% peels (four sessions) compared to topical retinoids in 21 patients with AN. At the end of the treatment period, 47.62 percent (n=10) of patients were in the topical retinoids group. Additionally, 85 percent (n=17) of patients in the TCA 15% peels group showed moderate improvement. Moreover, 23.81 percent (n=5) in the topical retinoids group, whereas 5 percent (n=1) in TCA 15% peels group showed good improvement (p=0.0395). They also reported better response with topical retinoids compared to TCA peels. However, TCA was more tolerated with less erythema and burning sensation.27
A statistically significant reduction in ANASI scores was observed for both the fractional CO₂ laser side and the TCA 20% peel side, with the fractional CO₂ peel side exhibiting a higher reduction percentage.
Likewise, Abu Oun and her colleagues studied 20 Egyptian patients with neck-AN, administering fractional CO₂ laser on the right half of the neck and retinoic acid peel to the left half. After therapy, there was a highly significant decrease in the score on both halves, whereas there was no difference between the two halves prior to therapy. Nevertheless, there was a highly significant difference between the two halves after therapy, with the laser-treated half producing superior results than the peeling-treated half.28
Contrary to the findings of Zaky et al., the mean decrease in ANASI on the glycolic acid peel 70% side was 10.05 (± 6.01), representing a 43 percent decrease, while that on the fractional CO₂ laser side was 4.40 (± 6.63) representing 19 percent decrease. There was a statistical difference between the two sides (P=0.008).25
In terms of side effects, the current study found that the side treated with fractional CO₂ laser had a statistically significant higher incidence of pain and erythema than the side treated with TCA (20%). Post-inflammatory hyperpigmentation was tolerable and did not require treatment cessation, and there was no statistically significant difference between the two sides.
After TCA application to the neck, 10 percent of patients in the current study exhibited post-inflammatory symptoms. This finding is due to the unavoidable friction at this site and the lack of postoperative care. In post-inflammatory hyperpigmentation (PIH) cases, TCA peeling sessions were continued until the hyperpigmentation was entirely resolved.
Conclusion
Both fractional CO₂ laser and TCA (20%) appear effective, well-tolerated, and promising treatment options for AN. TCA is a simple, effective method with faster good results, whereas fractional CO₂ lasers provide better long lasting skin tone and texture improvement. The treatment of the underlying cause, particularly obesity, is also crucial.
Limitations. Despite the promising outcomes of the current study, the small sample size was considered the main limitation. Short follow-up time is another disadvantage. Since AN is a chronic condition, we recommend continuing treatment with maintenance sessions to sustain positive outcomes and reduce the risk of relapse.
References
- Pollitzer S and Janovsky V. Acanthosis nigricans. In: Morris MA, Unna PG, Duhring LA, Leloir H-C-C, eds. International Atlas of Rare Skin Diseases.Voss, Hamburg und Leipzig; Lewis, London; Masson, Paris 1890, Band 4.
- Karadağ AS, You Y, Danarti R, et al. Acanthosis nigricans and the metabolic syndrome. Clin Dermatol. 2018 Jan-Feb;36(1):48–53.
- Curth HO. Classification of acanthosis nigricans. Int J Dermatol. 1976;15(8):592–593.
- Hernández-Pérez E. On the classification of Acanthosis Nigricans. Int J Dermatol. 1984;23(9):605–606
- Schwartz RA. Acanthosis nigricans. J Am Acad Dermatol. 1994;31(1):1–19.
- Das A, Datta D, Kassir M, et al. Acanthosis nigricans: A review. J Cosmet Dermatol. 2020 Aug;19(8):1857–1865.
- Karadağ AS, You Y, Danarti R, et al. Acanthosis nigricans and the metabolic syndrome. Clin Dermatol. 2018 Jan-Feb;36(1):48–53.
- Phiske, MM. An approach to acanthosis nigricans. Indian Dermatol Online J. 2014;5:239–249
- Baldissera RL, Yang EJ, Schmitt JV, et al . Trichloroacetic acid peels for the treatment of acanthosis nigricans. J Am Acad Dermatol. 2022 Jan;86(1):203–204.
- Rafalson L, Pham TH, Willi SM, et al. The association between acanthosis nigricans and dysglycemia in an ethnically diverse group of eighth grade students. Obesity (Silver Spring). 2013 Mar;21(3):E328–333.
- Mir A, Wu T, and Orlow SJ. Cutaneous features of Crouzon syndrome with acanthosis nigricans. JAMA Dermatol. 2013;149:737–741.
- James WD, Elston DM, Treat JR, et al. eds. Endocrine diseases. In: Andrew’s Diseases of the Skin: Clinical Dermatology (13th ed). Canada: Elsevier Inc.; 2020:502
- Mourad AI, Haber RM. Drug-induced acanthosis nigricans: A systematic review and new classification. Dermatol Ther. 2021 Mar;34(2):e14794
- Ng HY. Acanthosis nigricans in obese adolescents: prevalence, impact, and management challenges. Adolesc Health Med Ther. 2017;8:1–10
- Helou J, Korkomaz J, Stephan F, et al. Searching predictive factors of efficacy and safety in a fractional CO2 laser. Dermatol Ther. 2020 Nov;33(6):e13985.
- Patel NU, Roach C, Alinia H, et al. Current treatment options for acanthosis nigricans. Clin Cosmet Investig Dermatol. 2018 Aug 7;11:407–413.
- Fanous N, Zari S. Universal Trichloroacetic Acid Peel Technique for Light and Dark Skin. JAMA Facial Plast Surg. 2017 May 1;19(3):212–219.
- O’Connor AA, Lowe PM, Shumack S, et al. Chemical peels: A review of current practice. Australas J Dermatol. 2018 Aug;59(3):171–181.
- Ng HY. Acanthosis nigricans in obese adolescents: prevalence, impact, and management challenges. Adolesc Health Med Ther. 2016 Dec 16;8:1–10.
- Wijnberg D, Deutman H, Steijlen P, et al. CO2 laser treatment of benign juvenile acanthosis nigricans. E J Plastic Surg. 23, 238–240.
- Campos MA, Varela P, Baptista A, et al. Unilateral nevoid acanthosis nigricans treated with CO2 laser. BMJ Case Rep. 25:2016
- Leerapongnan P, Jurairattanaporn N, Kanokrungsee S, et al. Comparison of the effectiveness of fractional 1550-nm erbium fiber laser and 0.05% tretinoin cream in the treatment of acanthosis nigricans: a prospective, randomized, controlled trial. Lasers Med Sci. 2020;35(5):1153–1158
- Elmasry MF, Khalil MMF, Badawi A, et al. Efficacy of Fractional Carbon Dioxide (CO2) Laser versus Q-Switched Neodymium-Doped Yttrium Aluminum Garnet (Nd:YAG) and Potassium-Titanyl-Phosphate (KTP) Lasers in the Treatment of Acanthosis Nigricans. Clin Cosmet Investig Dermatol. 2023 Mar 23;16:705–715.
- Eldeeb F, Wahid RM, Alakad R. Fractional carbon dioxide laser versus trichloroacetic acid peel in the treatment of pseudo-acanthosis nigricans. J Cosmet Dermatol. 2022 Jan;21(1):247–253.
- Zaki NS, Hilal RF, Essam RM. Comparative study using fractional carbon dioxide laser versus glycolic acid peel in treatment of pseudo-acanthosis nigricans. Lasers Med Sci. 2018 Sep;33(7):1485–1491.
- Zayed A, Sobhi RM, Abdel Halim DM. Using trichloroacetic acid in the treatment of acanthosis nigricans: a pilot study. J Dermatolog Treat. 2014 Jun;25(3):223–225.
- Rajegowda HM, Kalegowda D, Madegowda SB, et al. To compare the efficacy and safety of trichloroacetic acid peel with topical tretinoin in the treatment of acanthosis nigricans: A randomized controlled study. J Pak Assoc Dermatol. 2019Oct.6;29(2):170–175.
- Abu Oun AA, Ahmed NA, Hafiz HSA. Comparative study between fractional carbon dioxide laser versus retinoic acid chemical peel in the treatment of acanthosis nigricans. J Cosmet Dermatol. 2022 Mar;21(3):1023–1030.