 J Clin Aesthet Dermatol. 2023;16(11):43–46.
J Clin Aesthet Dermatol. 2023;16(11):43–46.
by Mariem Rekik, MD; Fatma Hammami, PhD; Ines Saguem, PhD; Khadija Sellami, PhD; Abderrahmen Masmoudi, Prof; Mariem Amouri, Prof; Madiha Mseddi, Prof; Tahya Sellami, Prof; Emna Bahloul, PhD; and Hamida Turki, Prof
Drs. Rekik, Hammami, Bahloul, Sellami, Masmoudi, Amouri, Mseddi, and Turki are with the Dermatology Department at Hedi Chaker Hospital University in Sfax, Tunisia. Drs. Saguem and Sellami are with the Pathology Department at Habib Bourguiba University Hospital in Sfax, Tunisia.
ABSTRACT: Background. Basaloid follicular hamartoma is an uncommun benign neoplasm of the hair follicule. The linear form of basaloid follicular hamartoma can be associated with basal cell carcinoma.
Objective. We report a case of a patient with multiple basal cell carcinomas developing on a congenital lesion allowing the diagnosis of basaloid follicular hamartoma on histopathology.
Methods. Each lesion was evaluated by two dermatologists. All biopsy specimens were routinely stained with hematoxylin-eosin.
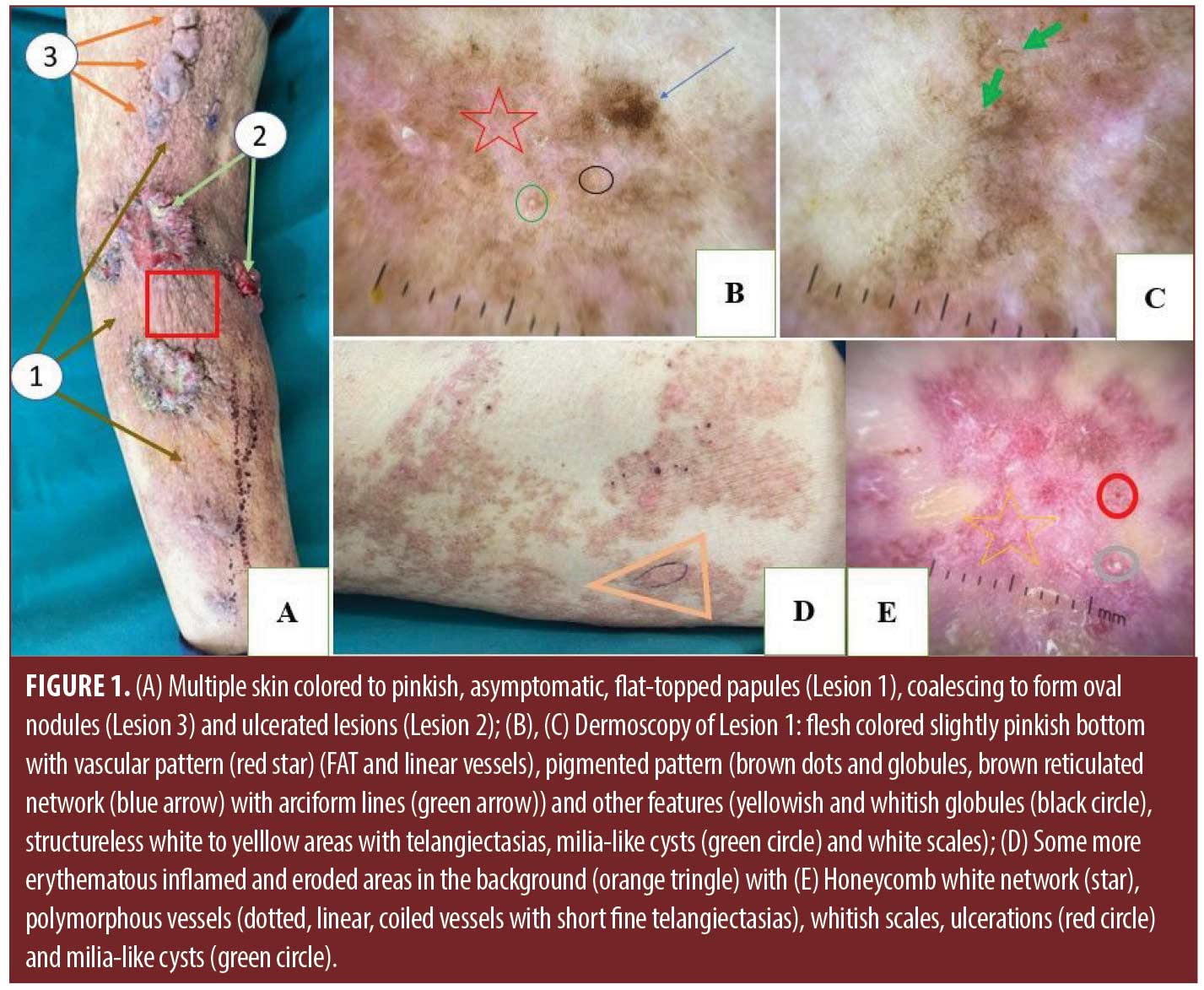
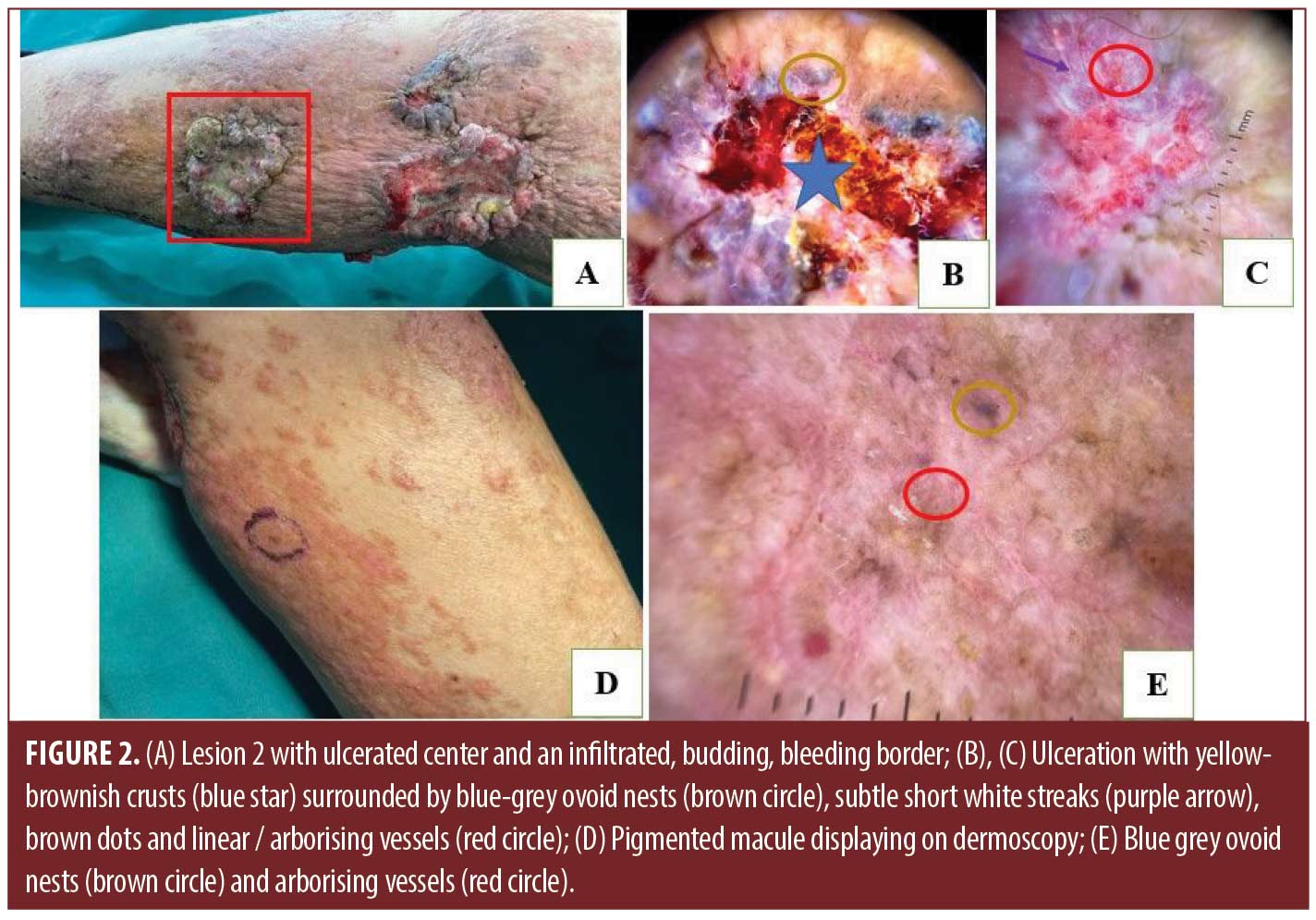
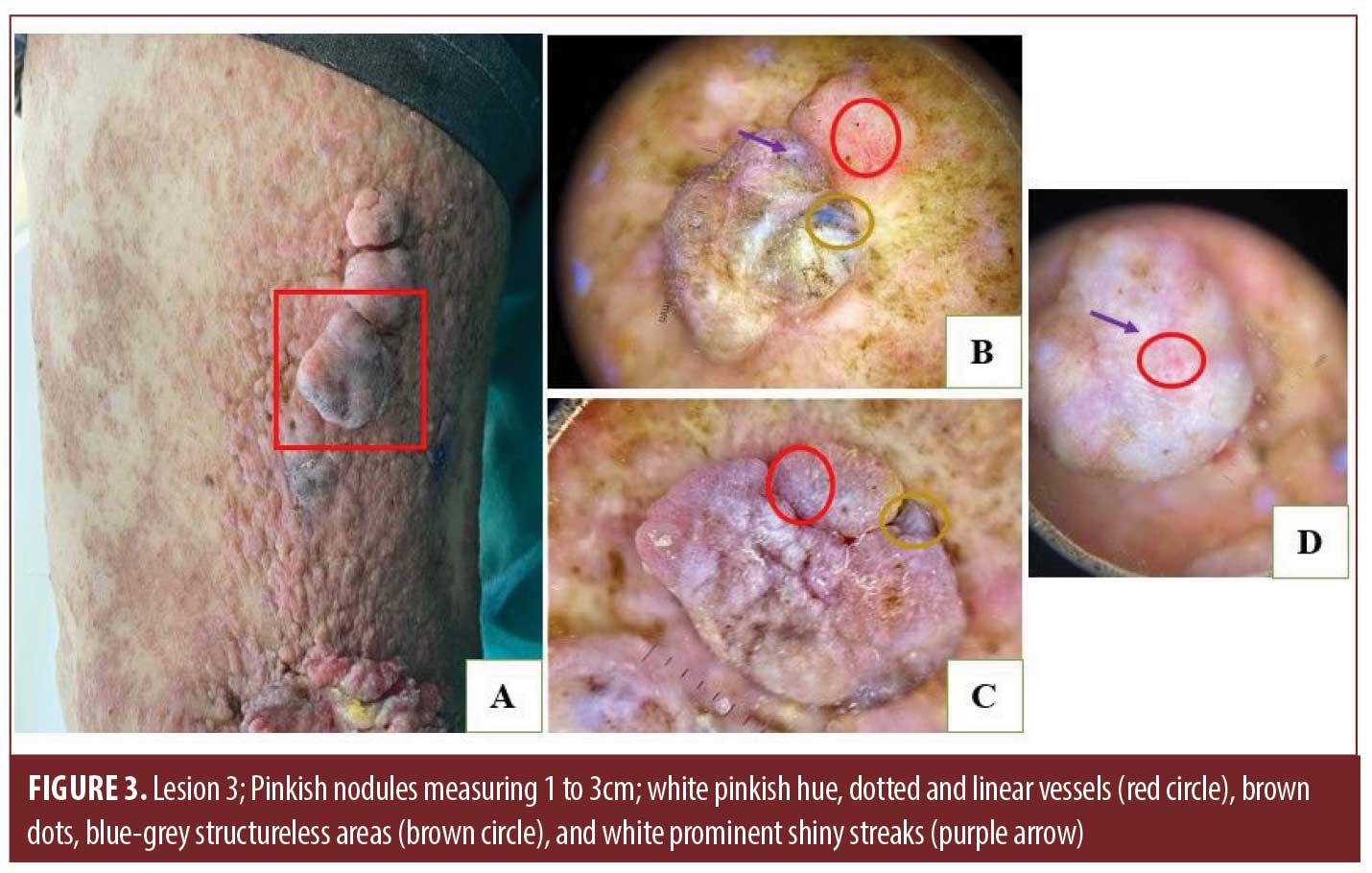
Results. A 76 year-old-man consulted our dermatology departement for erythematous papules spread over the left lower limb. The lesion had been evolving since birth with flesh-colored to pinkish papules following Blaschko’s lines from the root of the thigh to the foot. Three months before consultation, the papules increased in size leading to nodules with sometimes an ulcerated center. Dermoscopy under polarized mode displayed for ulcerated lesions (A) yellow-brownish crusts and ulceration surrounded by blue-grey ovoid nests, subtle short white streaks, brown dots and linear/arborising vessels. For nodular lesions (B), dermoscopic features are white pinkish hue, dotted and linear vessels, brown dots, blue-grey structureless areas and white prominent shiny streaks. There were some more erythematous inflamed and eroded areas in the background with a reversed honeycomb white network on dermoscopy (C), polymorphous vessels, whitish scales, ulcerations and milia-like cysts. The background lesion showed varied dermoscopic structures on a flesh colored slightly pinkish bottom (D). Histolopathology concluded for lesions A to an infiltrating and nodular basal cell carcinoma, (B) and (C) to fibroepithelioma of Pinkus and (D) to basaloid follicular hamartoma.
Conclusion. Several case reports have documented dermoscopic features of a solitary basaloid follicular hamartoma. However, further studies are required to specify any reproducible features.
Keywords: Basal cell carcinoma, Blashcko’s lines, basaloid follicular hamartoma, Fibroepithelioma of Pinkus
Basaloid follicular hamartoma (BFH) is an uncommon benign neoplasm of the hair follicle described in 1952.1–3 It has different clinical presentations. This disorder can be familial, congenital, or acquired.2 Even though it is a benign tumor, lesions can be cosmetically unacceptable and can be associated with numerous disorders such as basal cell carcinomas (BCC).3 We report a case of a patient with multiple BCC developing on a congenital BFH.
Case report
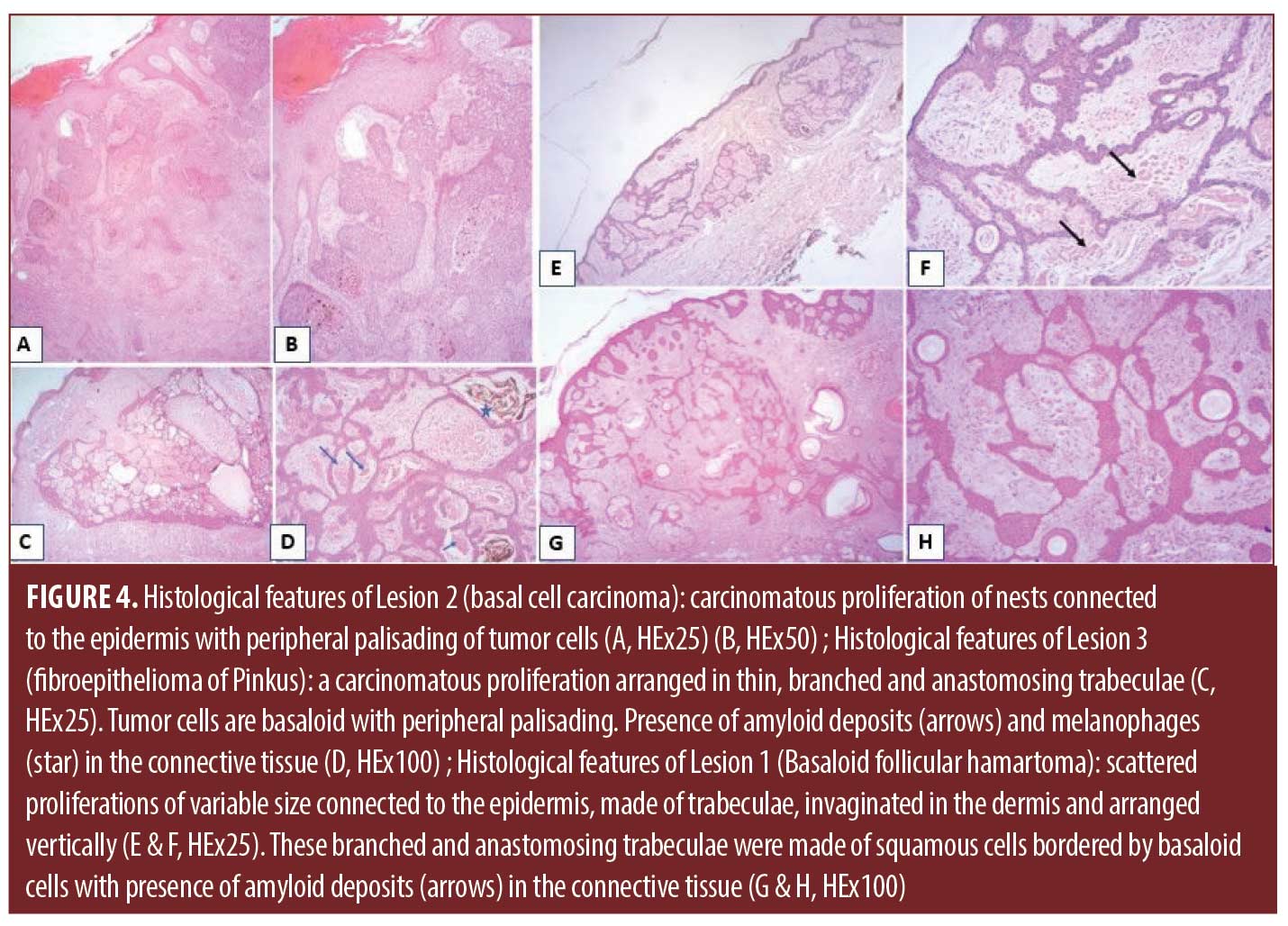
A 76-year-old man consulted our dermatology department for multiple cutaneous nodules with recent rapid increase in size over the last three months. Physical examination revealed erythematous flesh-colored to pinkish papules spread over the left lower limb, following Blaschko’s lines from the root of the thigh to the foot (Figure 1). This lesion (Lesion 1) has been evolving since birth. On top of this lesion, there were four nodules having an ulcerated center and an infiltrated, budding, bleeding border were seen around the popliteal fossa (Lesion 2) (Figure 2) with three skin-colored to pinkish, asymptomatic, flat-topped, oval nodules (Figure 3) on the posterior aspect of the thigh (Lesion 3). There was no family history of such lesions and the rest of the cutaneous and systemic examination was unremarkable. Dermoscopy under polarized mode displayed for ulcerated lesions (Lesion 2): yellow-brownish crusts and ulceration surrounded by blue-grey ovoid nests, subtle short white streaks, brown dots and linear / arborising vessels (Figure 2). A pigmented macule displayed on dermoscopy blue-grey ovoid nests and arborinzing vessels (Figure 2). For nodular lesions (Lesion 3), dermoscopic features were white pinkish hue, dotted and linear vessels, brown dots, blue-grey structureless areas and white prominent shiny streaks (Figure 3). There were some more erythematous inflamed and eroded areas in the background with a reversed honeycomb white network on dermoscopy (Figure 1), polymorphous vessels (dotted, linear, coiled vessels with short fine telangiectasias (SFT)), whitish scales, ulcerations and milia-like cysts. The Lesion 1 showed varied dermoscopic structures on a flesh colored slightly pinkish bottom: vascular pattern (SFT and linear vessels), pigmented pattern (brown dots and globules, brown reticulated network with arciform lines) and other features (yellowish globules, structureless white to yellow areas, milia-like cysts and white scales) (Figure 1). One of the ulcerated nodules as well as the pigmented macule were biopsied and diagnosed as BCC. The patient underwent a wide excision of all the nodules with some of the background lesion. Histological examination of the ulcerated nodules (Lesion 2) showed a carcinomatous proliferation of nests connected to the epidermis and surrounded by retraction artifacts. Tumor cells were small and basal with high nuclear to cytoplasmic ratio and peripheral palisading (Figure 4). All the ulcerated nodules were diagnosed as infiltrating and nodular BCCs. The examination of the oval nodules on the posterior aspect of the thigh (Lesion 3) and of the erythematous and eroded areas revealed a connected proliferation to the epidermis, made of thin, branched and anastomosing trabeculae of basaloid cells with a palisading arrangement at the periphery, slight nuclear atypia and rare mitotic figures. The connective tissue, often cellular, contained amyloid deposits and melanophages (Figure 4). The Lesion 3 as well as the inflamed areas were diagnosed as fibroepithelioma of Pinkus (FeP). Regarding the background lesion (Lesion 1), it was formed by scattered proliferations of variable size connected to the epidermis, made of trabeculae, invaginated in the dermis and arranged vertically. These branched and anastomosing trabeculae were made of squamous cells bordered by basaloid cells. These cells showed neither atypia nor mitosis. They were associated with horny cysts and sebaceous glands. These trabeculae were separated by a vascularized connective tissue tissue with amyloid deposits (Figure 4). The diagnosis of BFH was retained. Given the extent of this hamartoma, monitoring was recommended.
Discussion
Basaloid follicular hamartoma is a rare benign follicular tumor with different clinical forms. It can be inherited or sporadic, congenital or acquired, localized or generalized.3 The linear form of BFH often presents at birth4,5 as in our patient, or develops in early childhood.6 Occurrence at puberty or at a later age has been reported.2,7 Clinical examination can show multiple skin-colored to pigmented follicular papules, nodules or plaques, with or without associated milia and/or comedones8 in a band-like configuration along the Blaschko’s lines7 as shown remarkably in our case, thus reflecting a cutaneous mosaicism.3 To date, less than 30 cases of linear and unilateral BFHs have been reported.2,9 Generally, BFH is isolated although other disorders can be associated. BCCs may develop in different clinical variants of hamartoma.3,10 They tend to arise de novo. We found ten cases of BFH related to BCC in a literature search. Out of these 10 cases, eight were of localized linear variant of BFH.11–13 Rapid change in size or appearance of BFH lesions may indicate BCC development.8 Del Barrio-Diaz et al11 stated that local inflammation can predict clinically malignant transformation in BFH. This fact is confirmed in our patient since inflammed areas showed FeP proliferation in histopathology. FeP is an uncommon, rare and slow growing variant of BCC with low risk of destruction. Mutations in the PTCH gene could be involved in its pathogenesis.14 There are some reports of FeP-like proliferations, or proliferations that resemble trichoepitheliomas developing on lesions of BFHs.5 However, to our knowledge, no cases of FeP associated with BFH have been described previously. Dermoscopy is very helpful for the evaluation of tumours arising on BFH. Dermoscopic features of different variant CBC are well defined currently. Vascular polymorphism overlying a homogenous white-pinkish coloration and the presence of peculiar white septal lines are the hallmark dermoscopic features of FeP. The white network represent an additional dermatoscopic feature that may be more specific for FeP. Dermoscopy may also be helpful for the prediction of malignant transformation in BFH by detecting blue-grey ovoid nests, white streaks, white network, erosions and polymorphous vessels as in our patient. Dermoscopic characterization of BFH with similar clinical and morphological attributes to our case is not available in the literature to enable comparison or assertion of our findings. Reported findings include bluish structureless areas,15 white, pink, and grey areas, lesion with globular pattern, brown globules,11 white globules with a follicular unit in the center,10 well defined rounded structures that contained brown-grey linear, arciform structures, comedo-like openings and milia-like cysts.9 Others reports found irregularly branched crown vessels and structureless areas with telangiectasias.9
The definite diagnosis of BFH is made by histological examination. BFH has histologic similarities with BCC especially the infundibulocystic form.12 Characteristic histological features of BFH include the presence of an epithelial proliferation connected to the epidermis, arising from hair follicles, and arranged vertically in the superficial and middle dermis, embedded in a fibrous stroma. This proliferation is composed of branching and anastomosing cords and thin strands of small squamoid and basaloid cells.2
Conclusion
We have reported a unique case of BCC and FeP arising on BFH. Several case reports have documented dermoscopic features of solitary BFH. However, further studies are required to specify any reproducible features. The premalignant potential of BFH is currently uncertain. Prophylactic surgery is not indicated, especially in multiple forms. Follow-up is nevertheless recommended.
References
- Segars K, Cooper H, Hogan DJ, et al. Basaloid Follicular Hamartoma. J Clin Aesthet Dermatol. mars 2018;11(3):39–41.
- López Jiménez EC, Grau C, Islas Norris D, et al. Linear Unilateral Basaloid Follicular Hamartoma Following Blaschko’s Lines: Two Case Reports and Review of the Literature. Pediatr Dermatol. juill 2017;34(4):e196–200.
- Hazemann G, Michel C, Mahé A, et al. Hamartome folliculaire basaloïde : étude anatomoclinique. Annales de Dermatologie et de Vénéréologie. March 2019;146(3):181–191.
- Lee MW, Choi JH, Moon KC, et al. Linear basaloid follicular hamartoma on the Blaschko’s line of the face. Clin Exp Dermatol. janv 2005;30(1):30–34.
- Kaiser A, Spence RJ, Parwani A, et al. Basaloid follicular hamartoma with trichoblastomatous proliferations. J Cutan Med Surg. Cct 2003;7(5):395–398.
- Kim TH, Oh SJ, Kim YC, et al. Segmentally arranged hyperpigmented basaloid follicular hamartoma. Ann Dermatol. avr 2015;27(2):218–220.
- ElBehairy S, Elbendary A, Moussa Z. Image Gallery: Linear unilateral basaloid follicular hamartoma: a unique presentation. Br J Dermatol. mars 2016;174(3):e11.
- Jain S, Khopkar U, Sakhiya J. Localized unilateral basaloid follicular hamartoma along Blaschko’s lines on face. Indian J Dermatol Venereol Leprol. févr 2019;85(1):60–64.
- Muhammed N, Dongre AM, Khopkar US. Clinicopathological and Dermoscopic Features in a Case of Linear and Unilateral Basaloid Follicular Hamartoma. Indian Dermatol Online J. Déc 2019;10(6):710–713.
- Adya KA, Inamadar AC, Palit A, et al. Dermoscopy of Linear Basaloid Follicular Hamartoma. Indian Dermatol Online J. Oct 2019;10(5):610–612.
- Barrio-Diaz PD, Meza-Romero R, González S, et al. Cutaneous inflammation as a marker of malignant transformation in a patient with linear unilateral basaloid follicular hamartoma. IJDVL. 1 mai 2019;85:287.
- Jih DM, Shapiro M, James WD, et al. Familial basaloid follicular hamartoma: lesional characterization and review of the literature. Am J Dermatopathol. avr 2003;25(2):130–137.
- Jiménez-Acosta FJ, Redondo E, Baez O, et al. Linear unilateral basaloid follicular hamartoma. J Am Acad Dermatol. août 1992;27(2 Pt 2):316–319.
- Lupu M, Clatici VG, Barinova E, et al. Fibroepithelioma of Pinkus: Dermoscopic and reflectance confocal microscopic patterns. Dermatol Ther. mars 2021;34(2):e14831.
- Choi E, Liau M, Huang J, et al. Basaloid follicular hamartoma: clinical, dermoscopic, and histopathological characteristics of case. Dermatol Online J. 15 mai 2017;23(5):13030/qt3xn054wf.