
J Clin Aesthet Dermatol. 2021;14(2):42–43.
by Noureddine Litaiem, MD; Olfa Charfi, MD; Takwa Bacha, MD; and Faten Zeglaoui, MD, PhD
All authors are with the Department of Dermatology at Charles Nicolle Hospital in Tunis, Tunisia.
FUNDING: No funding was provided for this article.
DISCLOSURES: The authors report no conflicts of interest relevant to the content of this article.
ABSTRACT: Alopecia areata (AA) is an autoimmune disease that affects the hair follicles and leads to nonscarring alopecia. Nails changes are a common manifestation in AA, with an average prevalence of 30 percent. Both nail changes and hair loss in AA are associated with lymphocytic inflammation and are thought to be a result of a loss of immune privilege in both hair follicle and nail apparatus. Koilonychia, or “spoon nails,” is a nail dystrophy where the nail plate is depressed centrally and everted laterally. Causes of nail spooning are various, but koilonychia is usually associated with iron deficiency and inflammatory dermatoses, such as psoriasis and lichen planus. Koilonychia is very rarely reported in association with AA in the English literature and its prognostic significance is still unknown. We report a case of a 25-year-old female patient who presented with AA focalis and koilonychia that regressed almost completely after oral corticosteroids, with an accompanying discussion of the pathogenesis and prognostic value of koilonychia.
KEYWORDS: Alopecia areata, koilonychia, nail changes
Alopecia areata (AA) is an autoimmune disease that affects the hair follicles leading to nonscarring alopecia. It affects approximately 0.1 to 0.2 percent of the general population. Nails changes are a common manifestation in AA, with an average prevalence of 30 percent.1 Nails can be affected before or after hair loss. The most frequent nail abnormalities are pitting and trachyonychia.1 However, there are many other reported changes, such as Beau’s lines and onycholysis. Nail changes in patients with AA are associated with a poor prognosis.2
Koilonychia, or “spoon nails,” is a nail dystrophy wherein the nail plate is depressed centrally and everted laterally. Causes of nail spooning are various, but koilonychia is usually associated with iron deficiency and inflammatory dermatosis, such as psoriasis and lichen planus.3 To the best of our knowledge, koilonychia has never been reported in association with AA in the English literature.4,5
Case Presentation
A 25-year-old female patient presented with a four-month history of hair loss affecting mainly the frontal region. Hair loss was associated with dystrophy of all fingernails and toenails. There was no family history of nail changes, hemochromatosis, or hemoglobinopathy. She reported no poor nutrition, alcohol abuse, joint pain, or signs of gastrointestinal reflux.
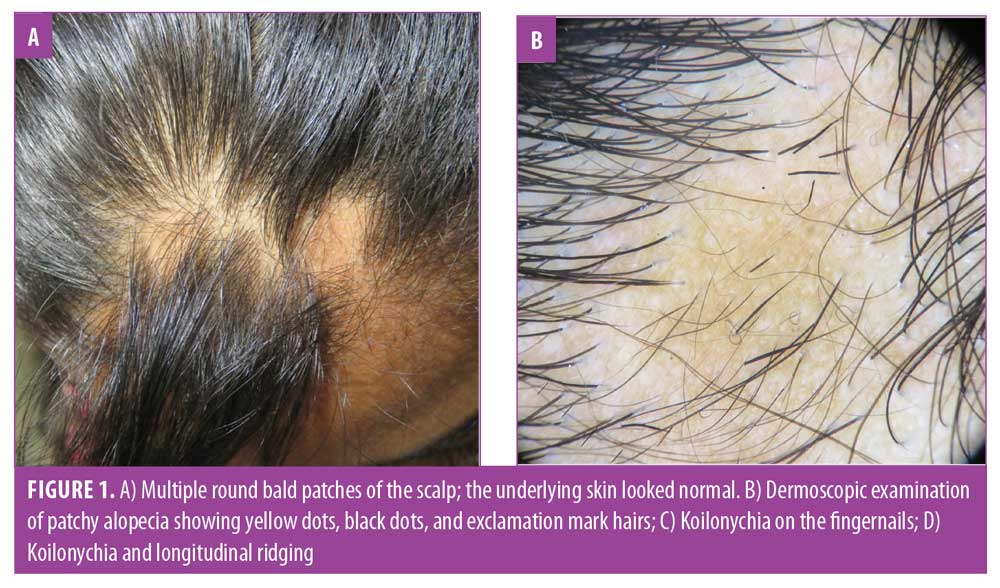
Clinical examination showed multiple round bald patches of the scalp; however, the underlying skin looked normal (Figure 1A). Meanwhile, there was no hair loss in the eyebrows, the eyelashes, or the rest of the body. Dermoscopic examination of patchy alopecia revealed yellow dots, black dots, and exclamation mark hairs (Figure 1B). All nails were dystrophic, showing koilonychia (Figures 1C and 1D). Excessive longitudinal ridging (i.e., onychorrhexis) was present, especially on the toenails (Figure 1D). The patient was concerned with the cosmetically disfiguring aspect of the nails but reported no pain or discomfort. Her physical examination was otherwise unremarkable. There was no atrophic glossitis or erythematosquamous lesions. Blood tests did not suggest anemia, and her iron, ferritin, and thyroid-stimulating hormone levels were within normal range. The diagnosis of koilonychia associated with AA focalis was made.

The patient was treated by both topical and oral corticosteroids (oral prednisolone 0.5 mg/kg/month for three months). After one month of therapy, new hair had emerged in the scalp simultaneously with a fast improvement of the nail aspect (Figure 2). After three months of follow-up, there was total hair regrowth and a progressive normalization of the nail plate.

Discussion
AA is the most common cause of inflammation-mediated nonscarring alopecia. The disease may be limited to round or oval patches of alopecia (AA focalis) or it could involve the entire scalp (AA totalis) or even the entire body (AA universalis).
Nail changes are often overlooked on physical examination.5 They could, however, be associated with significant cosmetic disfigurement or pain or may hinder normal daily activities.2,5
The most frequent nail changes associated with AA are pitting and trachyonychia.2,5 Other reported changes included onychorrhexis, Beau’s lines, onycholysis, punctate leukonychia, and red-spotted lunula.2,4 In our patient’s case, nail changes associated with AA were koilonychia and onychorrhexis. Koilonychia could be associated with several diseases, including iron deficiency, inflammatory skin diseases (e.g., lichen planus, psoriasis), onychomycosis, anemia, Plummer-Vinson syndrome, connective tissue diseases, dysthyroidism, poor nutrition, and familial koilonychia.3 Each of these conditions were ruled out in the present case. Koilonychia was associated with onychorrhexis and almost resolved simultaneously with alopecia. Therefore, the diagnosis of koilonychia associated with AA was made.
The pathogenesis of koilonychia is poorly understood and could be related to nail inflammation resulting in a relative depression of the distal matrix relative to the proximal matrix.3 Both nail changes and hair loss in AA are associated with lymphocytic inflammation and are considered to be a result of a loss of immune privilege in both the hair follicle and nail apparatuses.6,7 It is possible that koilonychia, in this case, was a consequence of a lymphocytic inflammation of the nail matrix leading to the observed spoon-shaped abnormality.
To date, there is no internationally standardized therapy regimen for AA-related nail changes.3,4 Topical, intralesional, and systemic corticosteroids were used with variable degrees of efficacy.5 Recently, Janus kinase inhibitors were used with encouraging results.8 In our case, koilonychia was associated with a limited form of AA and regressed almost completely and rapidly with oral corticosteroids.
While trachyonychia and red spots on the lunula have been reported as predictors for severe forms of AA,2 koilonychia may be considered a transient sign and may be associated with less severe forms of the disease.
References
- Kasumagic-Halilovic E, Prohic A. Nail changes in Alopecia Areata: Frequency and clinical presentation. J Eur Acad Dermatol Venereol. 2009;23(2):240–241.
- Roest YBM, van Middendorp HT, Evers AWM, et al. Nail involvement in alopecia areata: a questionnaire-based survey on clinical signs, impact on quality of life and review of the literature. Acta Derm Venereol. 2018;98(2):212–217.
- Walker J, Baran R, Velez N, Jellinek N. Koilonychia: an update on pathophysiology, differential diagnosis and clinical relevance. J Eur Acad Dermatol Venereol. 2016;30(11):1985–1991.
- Park JW, Kim SW, Wang HY. Nail abnormalities in alopecia areata. Korean J Dermatol. 2003;41(2):152–157.
- Chelidze K, Lipner SR. Nail changes in alopecia areata: an update and review. Int J Dermatol. 2018;57(7):776–783.
- Tosti A, Fanti PA, Morelli R, et al. Trachyonychia associated with alopecia areata: a clinical and pathologic study. J Am Acad Dermatol. 1991;25(2 Pt 1):266–270.
- Ito T, Ito N, Saathoff M, et al. Immunology of the human nail apparatus: the nail matrix is a site of relative immune privilege. J Invest Dermatol. 2005;125(6):1139–1148.
- Dhayalan A, King BA. Tofacitinib citrate for the treatment of nail dystrophy associated with alopecia universalis. JAMA Dermatol. 2016;152(4):492–493

