 J Clin Aesthet Dermatol. 2023;16(11):47–49.
J Clin Aesthet Dermatol. 2023;16(11):47–49.
by Elizabeth Kream, MD; Neil Jairath, MD; Shirin Bajaj, MD; David Orbuch, MD, MBA;
Jordan V. Wang, MD, MBE, MBA; and Roy G. Geronemus, MD
Drs. Kream, Bajaj, Orbuch, Wang, and Geronemus are with the Laser and Skin Surgery Center of New York in New York, New York. Dr. Jairath is with the Ronald O. Perelman Department of Dermatology at New York University Langone Health in New York, New York. Additionally, Dr. Geronemus is with the Ronald O. Perelman Department of Dermatology at New York University Langone Health in New York, New York.
FUNDING: No funding was provided for this article.
DISCLOSURES: Dr. Geronemus is on the advisory board for Candela, Cynosure, and Lutronic. Dr. Wang is on the advisory board for Lutronic.
ABSTRACT: Background. Cosmetic tattoos in the periocular area, including microblading, have become increasingly popular. More patients have been seeking laser tattoo removal.
Objective. A retrospective chart review for the laser treatment of eyeliner and eyebrow tattoos and a discussion of treatment experiences can better inform physicians.
Methods. A retrospective chart review was performed over five years with patients who had eyeliner and/or eyebrow tattoos and had laser removal.
Results. Overall, 76 patients were treated. Mean age was 47 years, and 98.7 percent were women. Fitzpatrick Skin Types I-VI were represented. Of all cases, 55.3 percent included eyebrows, 43.4 percent eyelids, and 1.3 percent both. There was a mean of 2.8 treatments. Common colors included black (73.7%), black/red (7.9%), black/orange (5.3%), black/yellow (3.9%), and red (3.9%). Most cases were treated with 755nm picosecond laser or high peak-powered 532nm/1064nm picosecond laser. After initial treatment, 26.3 percent of cases involved unmasking of colors, such as red, orange, yellow, green, and blue, which were not previously visualized. There were no documented adverse events related to scarring, hypotrichosis, necrosis, and burns.
Conclusion. Laser removal of eyeliner and eyebrow tattoos can be safe and effective. There should be consideration for eye and hair protection, pain control, and pigment unmasking.
Keywords: Aesthetics, dermatology, tattoos, lasers, cosmetics
Cosmetic tattooing has become a lucrative industry, with eyeliner and eyebrow tattoos being some of the earliest adopted forms.1 Although in vogue for several decades, tattooing techniques and pigments have since evolved. Patients seeking cosmetic tattoo removal may have the traditional eyebrow or eyeliner tattoos, which were popular in the 1990s and involve metallic pigments deposited deeper into the dermis, or newer tattoos from microblading, which commonly involve the deposition of non-metallic pigments more superficially into the papillary dermis.2 While modern microblading techniques are seen as semi-permanent solutions that are meant to slowly fade over several months to years, cosmetic dissatisfaction, evolving beauty trends, and incorrect color choice or placement can prompt patients to seek laser tattoo removal. Given the myriad cosmetic tattoo techniques, ink colors and compositions, and lasers available, physicians should appreciate that each tattoo removal case is unique.
An early case of laser tattoo removal was in 1967, when Dr. Leon Goldman removed a patient’s body tattoos using an Nd:YAG and 694nm ruby laser.3 In the earlier days, tattoo removal often resulted in significant surrounding tissue destruction and scarring. However, in the 1980’s the theory of selective photothermolysis was popularized, indicating that exogenous pigment from tattoos could be selectively targeted as chromophores using specific wavelengths of light.4 For optimal tattoo pigment destruction, pulse durations must be shorter than thermal relaxation time.5 As tattoo particles are very small, rapid pulses of extremely short pulse durations, in the nanosecond to picosecond range, are necessary. These discoveries have revolutionized the field of laser tattoo removal, leading to the development of lasers with extremely short pulse durations, such as Q-switched nanosecond and picosecond lasers, to offer more precise chromophore targeting while minimizing surrounding tissue damage.
At our high-volume laser clinic, we have treated many eyeliner and eyebrow tattoos with lasers for removal. Through performing these cases and appreciating their individual nuances, our treatment approach has continued to evolve to optimize clinical outcomes. We performed a retrospective chart review of eyeliner and eyebrow tattoos treated with lasers for removal over a five-year period. We reviewed the types of cases treated, patient demographics, devices used, and treatment parameters, as well as assessed for any adverse events, with the aim that our experiences and treatment strategies can help to inform other physicians.
Methods
A retrospective chart review was performed between January 2017 and October 2022 for patients who had presented with eyeliner and/or eyebrow tattoos and had laser removal of these tattoos with adequate patient information and evaluable photographs available. Demographic, treatment, and outcomes data were reviewed.
Results
A total of 76 patients were treated. Mean age was 47 years (R: 22–75 years), and 98.7 percent (n=75) were women. Fitzpatrick Skin Types I-VI were represented. Of all cases, 55.3 percent (n=42) were eyebrow tattoos, 43.4 percent (n=33) were eyelid tattoos, and 1.3 percent (n=1) involved both the eyebrow and eyelid. There was a mean of 2.8 treatments (R: 1–12 treatments). The number of treatments performed correlated with mutual patient and physician satisfaction and optimal outcome. Colors treated included black only (73.7%; n=56), red only (3.9%; n=3), green only (1.3%; n=1), blue only (1.3%; n=1), black and red (7.9%; n=6), black and orange (5.3%; n=4), black and yellow (3.9%; n=3), black and blue (1.3%; n=1), and black and green (1.3%; n=1).
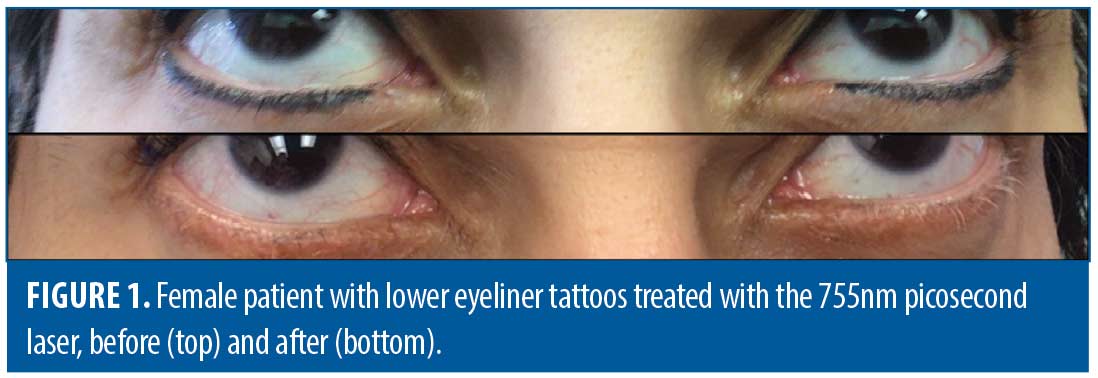
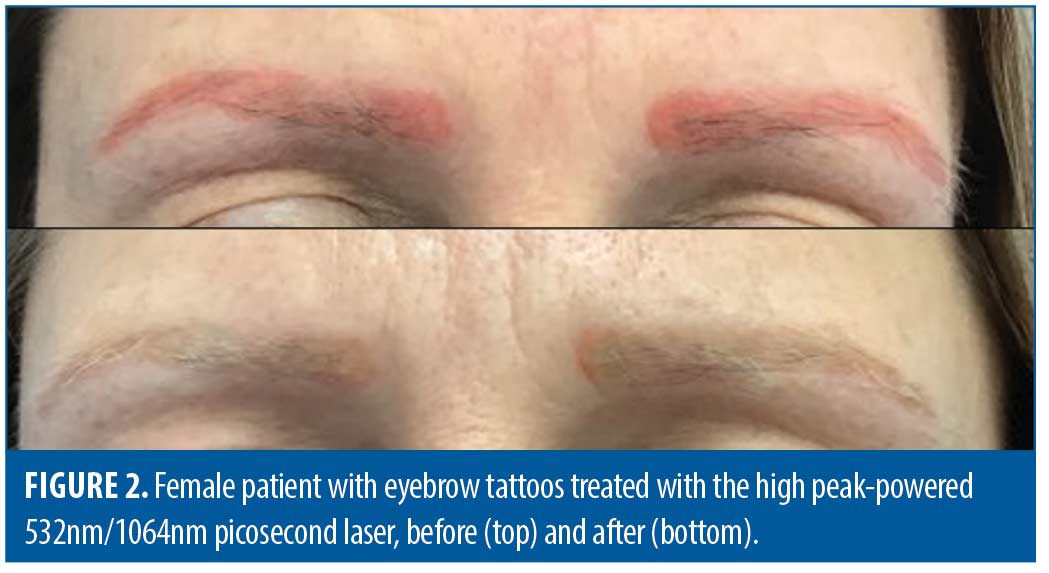
Most cases were treated with either a 755nm picosecond laser (50.0%; n=38) (PicoSure, Cynosure, Westford, MA) (Figure 1), a high peak-powered 532nm/1064nm picosecond laser (28.9%; n=22) (PicoPlus, Lutronic, South Korea) (Figure 2 and Figure 3), or a combination of these (18.4%; n=14). Singles cases (1.3%) were treated using either a fractional CO2 laser (1.3%; n=1) (CO2RE, Candela, Marlborough, MA) or Q-switched 1064nm nanosecond laser (1.3%; n=1) (Continuum Biomedical, Milpitas, CA).
Of the cases treated with the high peak-powered 532nm/1064nm picosecond laser, 61.1 percent (n=22) were treated with the 1064nm wavelength, 8.3 percent (n=3) were treated with the 532nm wavelength, and 30.6 percent (n=11) were treated with both wavelengths. For the 1064nm wavelength, spot size ranged 3-6mm, and fluence ranged 1.5-3.0J/cm2. For the 532nm wavelength, spot size ranged 3.3-5.3mm, and fluence ranged 0.7-2.0J/cm2. For the 755nm picosecond laser, spot size ranged 2.5-4mm, and fluence ranged 2.3-3.8J/cm2.
After the initial treatments, about one-fourth of cases (26.3%; n=20) involved the unmasking of other colors, such as red, orange, yellow, green, and blue, which were not previously seen upon clinical inspection. These colors continued to respond to the appropriate wavelength of laser. There were no documented adverse events related to scarring, permanent hypotrichosis, necrosis, burns, prolonged erythema, prolonged swelling, or prolonged dyspigmentation.
Discussion
Treatment of eyeliner and eyebrow tattoos pose a significant and unique challenge, especially when they are from the more recently popular microblading technique. Compared to traditional tattoos that deposit ink deeper into the dermis, eyebrow microblading employs a blade composed of multiple stacked needles that deposit ink very superficially into the papillary dermis, with the goal of creating thin discrete strokes that appear to mimic the appearance of individual hairs.2 Additionally, the ink used in microblading may not contain such hard metals as iron oxide found in traditional tattoo ink, as microblading can also include a synthetic composite mixture of organic pigments, which can be tailored to the patient’s specific skin tone.2 Each patient may therefore have their own unique combination of pigments, different in type, density, depth, and composition.
Because multiple pigments can be blended to create unique shades in microblading, challenges can arise when treatment with a particular wavelength of laser unmasks the hidden pigments comprising the tattoo. For example, dark brown to black colored tattoos treated with a 1064nm laser have commonly resulted in the appearance of residual yellow, orange, and red pigmentation at follow-up.6 This is due to the darker pigment absorbing more of this particular wavelength for destruction and subsequent clearance. It is important to note that this is not the same phenomenon as paradoxical darkening, which is often seen when treating red and other skin tone colors commonly used for lipliner tattoos. Paradoxical darkening is due to the irreversible reduction of ferric oxide or titanium dioxide to ferrous oxide (jet black) or titanium oxide (dark violet), respectively.7
In concordance with claims that newer microblading ink may not always contain heavy metals like iron oxide, we less commonly experience paradoxical darkening and more commonly witness unmasking of the underlying pigments that are mixed together to provide that patient’s personalized color. In our experience, no eyeliner or eyebrow tattoo removal cases involved paradoxical darkening; however, over one-fourth of cases involved the unmasking of other colors, such as red, orange, yellow, green, and blue. At consultation for laser tattoo removal, physicians should inquire about the type of tattoo technique used (e.g., traditional tattoo vs. microblading) and counsel patients on the adverse events of paradoxical darkening associated with traditional tattoos and pigment unmasking with microblading.
Our chart review reflects our clinical experiences as we have shifted in treatment techniques. The sole case of fractional CO₂ laser was early on (2017) involving the treatment of resistant and unmasked red pigment from microbladed eyebrows. The sole case of Q-switched 1064nm nanosecond laser was also early on (2018) involving the treatment of microbladed eyebrows in a Fitzpatrick skin type VI patient. For both types of cases, we would now instead use a newer high peak-powered 532nm/1064nm picosecond laser from the start of treatment. The option to use both wavelengths can allow for greater versatility in terms of the color to be targeted, and the higher peak power can clear pigment particles more quickly. The device is unique in that it has a fixed 450ps pulse width, flat-top multi-mode beam profile, and low lasing threshold.
Our current treatment approach involves treating dark brown and black eyeliner and eyebrow tattoos with the high peak-powered 532nm/1064nm picosecond laser (PicoPlus, Lutronic, South Korea) using the 1064nm wavelength with a spot size of 4mm and fluence around 2J/cm2 (dependent on real-time clinical endpoint) or the 755nm picosecond laser (PicoSure, Cynosure, Westford, MA) with a spot size of 3mm and fluence around 2.83J/cm2 (dependent on real-time clinical endpoint). If there is a tint of light brown to red or orange at initial presentation or if this is unmasked, as is often in the case with microbladed eyebrows, we immediately treat with the high peak-powered 532nm/1064nm picosecond laser (PicoPlus, Lutronic, South Korea) using the 532nm wavelength with a spot size of 3.3 mm and fluence around 1.2-1.6J/cm2 (dependent on real-time clinical endpoint). Fluence is titrated based upon immediate tissue response and constantly re-evaluated throughout the treatment.
The use of lasers in the periocular area mandates several safety considerations. Protecting the eye is of utmost concern. This can commonly involve opaque goggles or corneal metal eye shields, depending on the treatment performed. For eyeliner tattoos, the latter is always used. Corneal eye shields should fit snugly on the patient’s eye globe. It is important to note that thinner corneal shields may cause thermal corneal injury at higher fluences and/or longer wavelengths of lasers secondary to conduction of heat.8 There are two reported studies examining corneal eye shield safety in facial laser treatments, which demonstrated that despite a risk of corneal abrasion, metal shields do not allow light transmission, nor do they result in significant temperature rise.9 In clinical practice, we inquire about a history of recent eye surgery, as inserting corneal shields can disrupt corneal grafts, and recent Lasik surgery should prompt consulting with the operating ophthalmologist for clearance. Additionally, while rare, corneal abrasions can occur, particularly in older patients when inadequate ophthalmic lubricant is used for shield placement. Physicians should have an ophthalmologist on call and a plan in place if patients exhibit concerning signs of corneal abrasion (e.g., photophobia, pain, tearing, redness).
Periocular skin is relatively thin and has less pilosebaceous units, which can be associated with a greater risk of thermal injury.10 Additionally, since treatment of both eyebrow and eyeliner tattoos involve eyebrow and eyelash hairs in the treatment area, it is important to apply a topical gel to protect them from thermal injury, which can include clear surgical lubricant gel prior to treatment. Patients should be counseled that hairs may temporarily turn white after treatment, but brow tint can be used to camouflage this temporary response. We have had no cases of permanent hair loss with our treatments.
Prior to laser tattoo removal, we also typically use anesthesia, either topical or local depending on the treatment area, laser wavelength, and physician and patient preference. For the eyelid and eyebrows, we typically use local anesthesia to make the patients more comfortable during the laser treatment. This has changed our tattoo removal practice, where patients are more apt to return for future treatments and the laser fluence can be titrated based on clinical endpoints as opposed to being limited by patient discomfort. In our experience, local anesthesia has not negatively impacted clinical outcomes, including the effectiveness and safety of laser tattoo removal treatments.
Conclusion
With the rise of cosmetic tattoos in the periocular area, physicians should be knowledgeable on the common challenges associated with treatment, including eye safety, hair safety, pain control, laser and parameter selection, and pigment unmasking. This discussion is meant to spur future conversations and new treatment techniques.
References
- Ortiz AE, Alster TS. Rising concern over cosmetic tattoos. Dermatol Surg. 2012;38(3):424–429.
- Marwah MK, Kerure AS, Marwah GS. Microblading and the science behind it. Indian Dermatol Online J. 2021;12(1):6–11.
- Arndt KA, Noe JM, Rosen S, Beth Israel Hospital (Boston Mass.). Laser Unit., Harvard Medical School. Department of Continuing Education. Cutaneous laser therapy: Principles and methods. A Wiley medical publication. Wiley; 1983:xiii, 241 p.
- Geronemus RG. Fractional photothermolysis: current and future applications. Lasers Surg Med. 2006;38(3):169–176.
- Ho SG, Goh CL. Laser tattoo removal: A clinical update. J Cutan Aesthet Surg. 2015;8(1):9–15.
- Jimenez G, Weiss E, Spencer JM. Multiple color changes following laser therapy of cosmetic tattoos. Dermatol Surg. 2002;28(2):177–179.
- Anderson RR, Geronemus R, Kilmer SL, et al. Cosmetic tattoo ink darkening. A complication of Q-switched and pulsed-laser treatment. Arch Dermatol. 1993;129(8):1010–1014.
- Ries WR, Clymer MA, Reinisch L. Laser safety features of eye shields. Lasers Surg Med. 1996;18(3):309–315.
- Russell SW, Dinehart SM, Davis I, et al. Efficacy of corneal eye shields in protecting patients’ eyes from laser irradiation. Dermatol Surg. 1996;22(7):613–616.
- Mainster MA, Stuck BE, Brown J Jr. Assessment of alleged retinal laser injuries. Arch Ophthalmol. 2004;122(8):1210–1217.