 J Clin Aesthet Dermatol. 2022;15(7):38-42.
J Clin Aesthet Dermatol. 2022;15(7):38-42.
by Christine Munia, MD; Meire Parada, MD; and Marcus Henrique de Alvarenga Morais, MD
Drs. Munia and Parada are in private practice in Sao Paolo, Brazil. Dr. Morais is in private practice in Belo Horizonte, Brazil.
FUNDING: No funding was provided for this article.
DISCLOSURES: The authors report no conflicts of interest relevant to the content of this article.
ABSTRACT: Background. The search for nonsurgical cosmetic procedures has increased considerably in recent years. A new injection technique, using vector direction, has shown good results in improving facial aesthetics but to date has only been performed with hyaluronic acid which can be associated with a risk of vascular complications. Therefore, in clinical practice, it would be interesting to assess this technique with a liquid product already widely used in the facial region, and at the same time bring the same aesthetic benefits, but with greater durability than hyaluronic acid.
Objective. To investigate the improvement of facial morphology in patients with facial flaccidity submitted to the vector technique using poly-L-lactic acid (PLLA) (Sculptra®; Galderma, Lausanne, Switzerland).
Case series. Here we report the outcomes of three cases of female patients, aged between 41 and 55 years, seeking improvement of facial flaccidity. In each patient, PLLA was applied in the posterior temporal region as a bolus, in three points, with a 2-mL injection in the upper region, 1.5mL in the midpoint, and 1.5mL at the bottom point. Each of the three patients showed an improvement in face morphology, with concomitant improvement in the support and stretching of the face and improvement in skin sagging in the upper, middle, and bottom regions.
Conclusion. The vector technique with PLLA is a viable alternative for the treatment of patients with facial skin flaccidity, providing harmonious and progressive improvement in the face morphology.
Keywords: Facial aging, cosmetic techniques, poly-L-lactic acid, vector technique
The number of aesthetic procedures in recent decades has increased significantly worldwide.1,2 Minimally invasive techniques have become increasingly popular due to the lower risk and shorter recovery time when compared to surgical procedures.3–5
As we age, we can observe a significant and gradual loss of facial volume due to bone and fat resorption and the loss of collagen and decreased collagen production, leading to changes in skin texture, tone, and quality.6 Recent studies on facial anatomy with a focus on morphology and its geometric changes have found that facial aging occurs in a three-dimensional manner—not only by reduced collagen and elastin in the skin, but also reduced superficial and deep fat pads due to bone resorption and ligament laxity; this results in a reduction in overall facial support.7,8 In this sense, the deepening and visibility of the temporal region is a typical sign of advancing age.
These changes also brought the line concept formed by facial ligaments recently proposed by Casabona et al,9 in which the medial and lateral facial layers are arranged differently. Medially, the facial layers are oriented obliquely to the skin surface, while laterally to this line, they are arranged parallel to the skin surface, forming a facial support network that, with aging, is gradually lost.
Further knowledge has also emerged with new facial anatomy assessments, demonstrating that in the more superficial layers (subcutaneous and superficial adipose pads), the vascular and nervous network are distributed in a way that provides greater safety in performing injectable procedures. The application of cutaneous fillers in these layers and laterally to the aforementioned ligament line can result in a lifting effect and consequent change in the face’s morphology.8,10
Based on these findings and concepts, a new technique was proposed by Casabona et al to improve volume and to produce a “lifting effect” through the vector application of hyaluronic acid application in the temporal region.9,11 The results presented were very satisfactory, with face morphology improvement, increased volume in the temporal region, reduction of periorbital wrinkles, eyebrow tail lifting, malar region repositioning and distally, marionette line reduction.7
Despite the encouraging results of the hyaluronic acid application in the temporal region, there is a significant risk of complications resulting from vascular obstruction due to its high viscosity.12 Therefore, a liquid product, such as poly-L-lactic acid (PLLA), could produce the same results with a good safety profile. PLLA is a biodegradable and biocompatible collagen biostimulator, whose effects result from a controlled, subclinical inflammatory response, which culminates in tissue collagen deposition.13 Its complete elimination occurs within approximately 18 months, but its clinical effects are noticed for up to 25 months.14
In this paper, we report our experience using the vector technique in the posterior temporal region with PLLA (Sculptra®; Galderma, Lausanne, Switzerland) and share the outcomes in three patients.
Methods
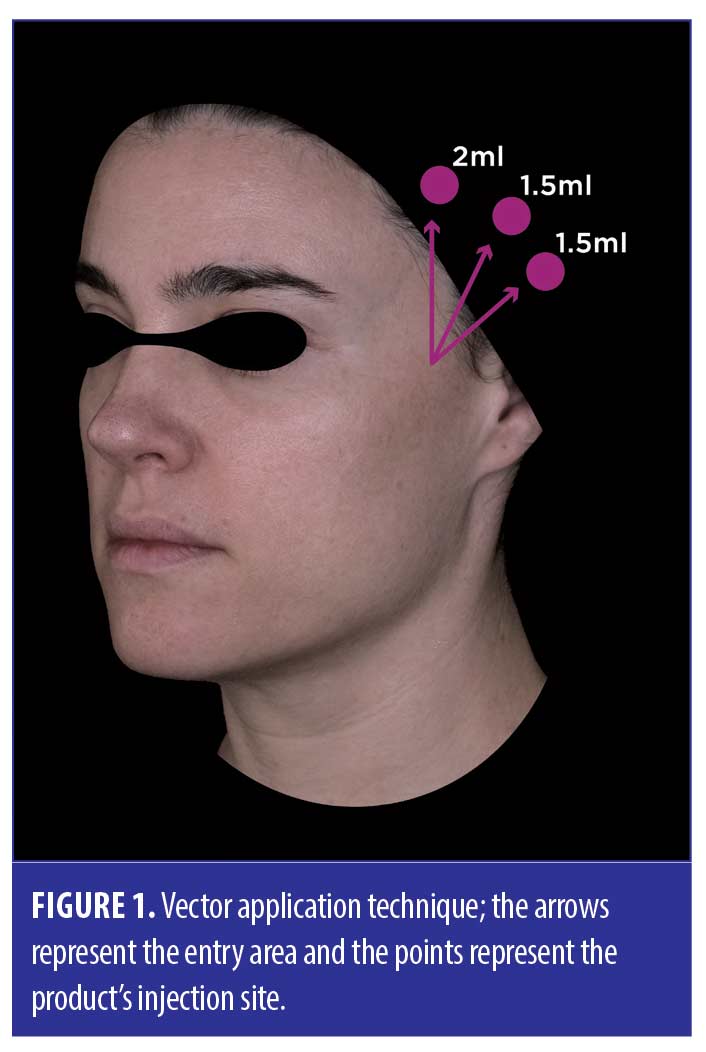
Vector technique description. The vector technique is indicated for patients who present loss of contour in the lower third of the face, loss of projection in the malar region, and greater visibility of the nasolabial and marionette lines. It consists of poly-L-lactic acid application in bolus, in the posterior temporal region, at three distinct points: lower (1.5mL injection), medium (1.5mL injection) and upper (2mL injection) through a single entry site, using the technique described above.7,8
In brief, before treatment, a thorough facial evaluation is performed to identify the areas that need to be treated and to confirm the suitability of the vector technique. A point is marked at 1cm from the capillary border, on the zygomatic arch. The patient is then placed in the supine position with the head turned to the contralateral side to the area to be injected; the cannula insertion hole is made with a 21G needle. The skin is raised through a pinch maneuver and the 22Gx70mm cannula is carefully introduced, parallel to the skin, to reach the subcutaneous plane with its path towards the superior temporal region, up to its size limit, to the lowest point. A slight resistance is observed in the passage, during the inferior temporal septum transfixation. This resistance must not be observed in the path and, if this occurs, this could indicate application in an incorrect plane. With the cannula in position and after light aspiration (to ensure non-intravascular location), 2mL-PLLA is applied in bolus along the first vector. The cannula is retracted posteriorly and directed to the superior temporal region midpoint, up to its limit and another 1.5mL-product is applied (again after light aspiration). Finally, a last point of application is performed with the product’s 1.5mL injection at the upper point of the injected area. Thus, with the distribution in three points, we performed the treatment of the lateral temporal-malar pad entire area (Figure 1).
Case Series
Case 1. A 55-year-old female patient came to the office seeking improvement for facial flaccidity and what she described as a tired-looking expression. Upon examination, there was a moderate degree of facial ptosis, descent of the cutaneous tissues, with periorbital groove (nasojugal and eyelid groove), nasolabial groove, marionette lines, and jowling, resulting in worsening of facial contour (Figures 2A and 2C). On physical examination, significant tissue mobilization was observed when performing manual traction posterior to the area to be treated.
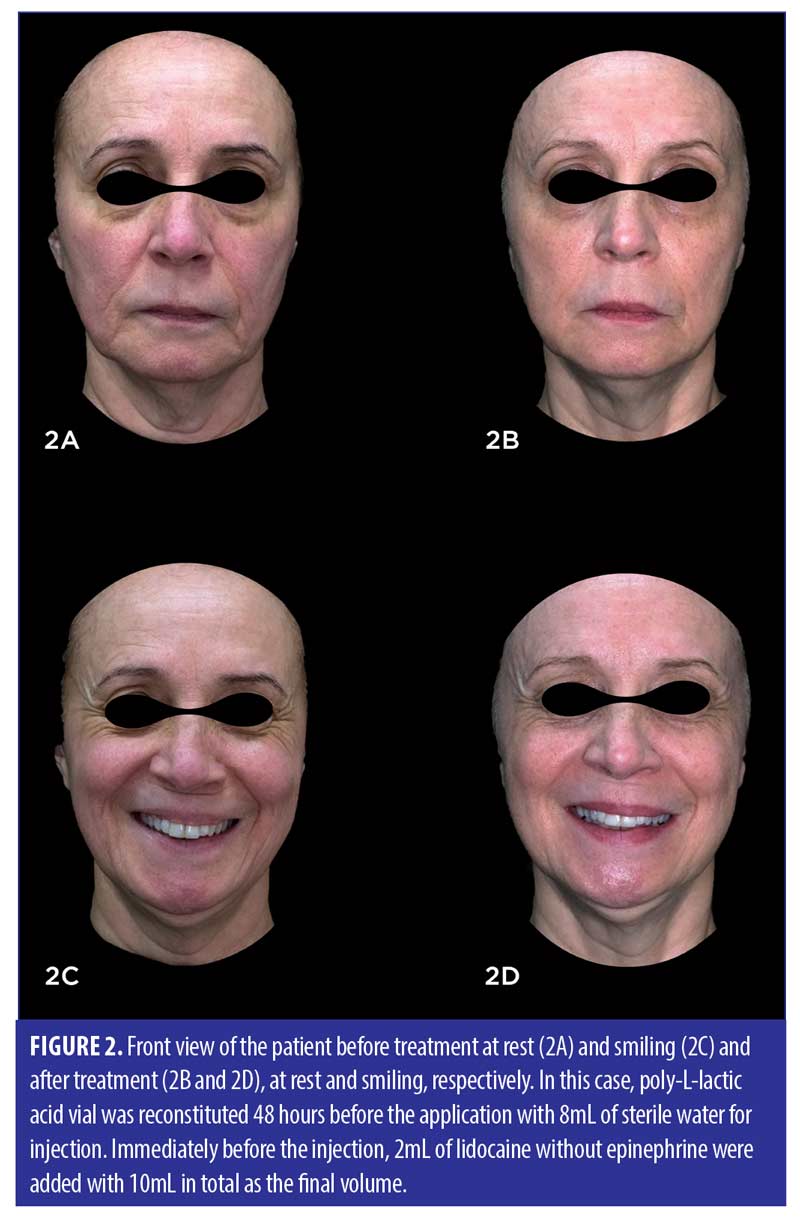
Due to the patient’s desire to reduce sagging and the tired-looking expression while maintaining a natural appearance without a clear increase in the face volume, the vector technique was chosen using PLLA in four sessions at monthly intervals.
Ninety days after the last application, a greater glance opening was observed in the upper third, with an apparent lifting of the eyebrows, increased distance between the eyebrows and the supraorbital groove, as well as a reduciton in the upper eyelid folds. In the middle third of the face, there was a significant reduction in the periorbital groove, with an appearance improvement of the infrapalpebral bags, nasolabial groove, in addition to an important repositioning of the malar and lateral zygomatic regions, giving an appearance of slight volumization. In the lower third of the face, we noticed an improvement in the marionette lines, as well as in the jowling, significantly impacting the facial contour of this patient (Figure 2B).
In the dynamic evaluation in the frontal view with the patient smiling with the same tooth exposure, there is an evident improvement of the periorbital wrinkles, including the most inferior ones, caused by the zygomatic muscle contraction during smiling, by elevating the malar region. To a lesser degree, an improvement in the accordion lines was also noted, as well as a more drawn lower facial contour, even in motion (Figure 2D).
Based on the description above, it is possible to observe the change in the patient’s facial shape before and after treatment, with an improvement in the face contour, going from a more square shape to a more oval shape, which gives a more youthful appearance overall.
Case 2. A 52-year-old female patient came to the office with facial flaccidity, deep nasolabial and labiomental grooves, noncontinuous facial contour in the lower third of the face, sagging around the mouth, and bags under the eyes.
Upon examination, the complaints presented by the patient were confirmed, with the visualization of skin flaccidity, well-demarcated nasolabial and labiomental grooves, and malar bags visualized at rest (Figure 3A). When smiling, cutaneous redundancy was observed with greater emphasis, especially in the lower third of the face (Figure 3C).

Given the presentation of flaccidity in the middle and lower third of the face and the need to reposition structures in the middle third (middle and medial malar fat pad) and improve the premandibular groove region, it was decided to apply PLLA in the temporal region based on the vector technique, in four sessions over four months.
After treatment, the repositioning of facial structures was observed, with a reduction in malar bags, facial groove smoothing, greater opening of the eyebrow tail, improved contour in the lower third of the face, and reduced visualization of the premandibular groove, both at rest and smiling (Figures 3B and 3B).
Case 3. A 41-year-old female patient, presented with complaints of wrinkles when smiling, a marked nasolabial fold, sagging in the lower part of the face, and a very round face. On examination, we examined accordion lines when smiling, mild flaccidity of the face’s lower and middle third, “heavy face” type, and a mild nasolabial groove (Figure 4A). Given the clinical presentation, the patient’s wishes, and in order to restructure the facial morphology and promote a superolateral lifting effect with consequent repositioning of the face’s middle and lower-third structures, the vector technique in the posterior temple region with PLLA was chosen.
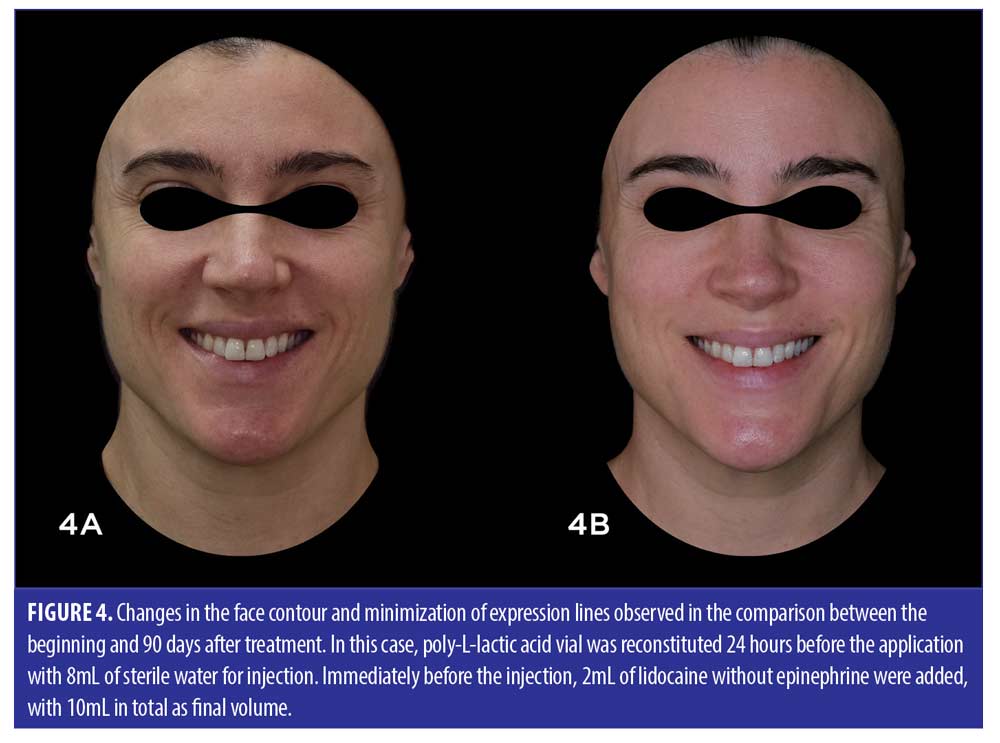
After treatment, we observed an improvement in accordion lines, improvement and definition of the facial contour in the temporomandibular region, change in face morphology (stretching), and lifting of the eyebrow tail when smiling (Figure 4B). In the middle third of the face, there was a reduction in the periorbital groove, with an improved appearance of the infrapalpebral bags, possibly due to the soft tissues repositioning. Also, visible improvement of nasolabial grooves was observed as an important repositioning of the malar and lateral zygomatic regions, giving an appearance of slight volumization.
Discussion
In these case reports, we present the face morphology changes both local and distant to the application site, such as in the mandibular region and nasolabial and labiomental groove, showing that PLLA application in a strategic region, based on the action vectors of the facial ligaments can lead to interesting results, with less need for the product and less discomfort and risk to the patient.
The vector action of forces at a given point has been studied for hundreds of years and the vector technique can be explained by it. Physiologically, the gravitational force on facial tissues generates a downward movement, specially of soft tissues. To keep the tissues in place, an opposing force to support these tissues is generated by the ligaments that support the face architecture. However, with aging, slackness of these ligaments causes the reaction force to the gravitational action to decrease, causing flaccidity and the loss of face contour and the facial tissues force. The vector technique aims at making up for the absence of strength in the ligaments due to aging, by giving traction support to areas with looser ligaments. What we observed in the cases presented here, as well as in published studies using the vector technique, was a perceived improvement in the face morphology, especially in the malar and mandibular regions, in addition to the nasolabial and labial-mental grooves attenuation.8,9,11,15
Among the important face ligaments responsible for supporting the architecture of the face, there are the zygomatic, masseteric, mandibular, maxillary, and eye orbit retainers. Since its publication, the vector technique with an adjuvant action for ligaments, some techniques have been proposed to act in different locations and ligaments.9,11 In our reports, we chose to apply it only in the posterior temporal region, for several reasons.
First, the choice was based on the importance of the temporal region as a vectorial support to the facial structures. The loss or reduction of the zygomatic ligaments action is easily observed with malar ptosis, the mandibular region and the appearance or enhancement of nasolabial and labial grooves, factors resulting from the gravitational action imbalance on antigravity facial fat, i.e., changes in the temporal region support directly or indirectly influence various face parts.15 For this broad effect, we raise the hypothesis of a myomodulator effect, generated by neocollagenesis, which causes tissue repositioning through the force vector generated, pulling the region super-laterally and, indirectly, the adjacent regions, thus impacting the overall facial mimicry dynamics.
The second reason is the areas ability to keep the product localized without suffering gravitational action. The temporal region is formed by 10 layers from the most superficial to the deepest layer: skin, superficial fat, superficial and deep temporal fascia, superficial temporal fat pad, deep lamina of deep temporal fascia, deep temporal fat pad, temporal muscle, and periosteum. The second layer, the superficial fat, contains the upper and lower superficial fat compartments and filler application in this region has been advocated because there is no movement of the injected product in the craniocaudal direction, thus providing stability to the injected product, even with the gravity action.7 In addition, it was observed that the fibers’ direction do not change even with aging, and this makes the subdermal fat layer an ideal place for treatments aimed at lifting and volumizing.9,11 For this reason, we decided to perform the application only in the posterior temporal region, subcutaneously.
Finally, but of paramount importance, is patient safety. Complications are a major concern when performing cosmetic procedures. Obstruction/vascular injury and nerve damage has been reported with PLLA. Although the temporal region is highly vascularized and innervated, pinching the area helps to locate the subcutaneous plane, above the superficial temporal fascia and the superficial temporal artery and vein.10
We chose to use PLLA over other fillers because PLLA is a safe, liquid product (reconstituted with sterile distilled water) consisting of very small particles, offering a lower risk of obstruction, even in small vessels. In addition, the temporal region application is already used and recommended for the PLLA application in association with other areas.18 As a biostimulator, the action of PLLA is longer lasting than with other products, as it acts through a controlled inflammatory process capable of stimulating endogenous collagen production, improving skin elasticity and promoting local support, with a high level of patient satisfaction.14,18–20
It is worth noting that, despite being an interesting and safe procedure, it is essential to understand all aspects of the aging process, anatomy, and the application plan. Beyond this, future studies with a large sample should be carried out to demonstrate the safety and the efficacy of the application, once this technique has previously used injectable hyaluronic acid, not PLLA.7,9,11,15
Conclusion
Based on the cases presented here, we conclude that the vector technique with PLLA could be an excellent alternative for the facial treatment of patients with overall facial flaccidity, improving the face morphology harmoniously and safely.
Acknowledgements
The authors thank Dr. Josy Davidson, Dr. Cristhine Kamamoto and Medsense Ltda for editorial assistance.
References
- International Society of Aesthetic Plastic Surgery (ISAPS). International Survey on Aesthetic/Cosmetic Procedures: Results 2018. 2018; 1–49.
- American Society of Aesthetic Plastic Surgeons. Cosmetic Procedures Performed in 2010. 2010; 1–11.
- Jacono AA, Malone MH, Lavin TJ. Nonsurgical facial rejuvenation procedures in patients under 50 prior to undergoing facelift: Habits, costs, and results. Aesthetic Surgery Journal. 2017; 37:448–453.
- Chao YYY: A single-visit approach using fillers and incobotulinumtoxin a: Full face enhancement in asian patients. Plastic and Reconstructive Surgery – Global Open. 2018; 6:1–4.
- Hojjat H, Raad R, Lucas J, et al. Public Perception of Facial Fillers. Facial Plastic Surgery. 2019; 35:204–209.
- Mendelson BC, Wong CH: Changes in the Facial Skeleton with Aging: Implications and Clinical Applications in Facial Rejuvenation. Aesthetic Plastic Surgery. 2020; 44:1159–1161.
- Suwanchinda A, Webb KL, Rudolph C et al. The posterior temporal supraSMAS minimally invasive lifting technique using soft-tissue fillers. Journal of Cosmetic Dermatology. 2018; 17:617–624.
- Cotofana S, Gaete A, Hernandez CA, et al. The six different injection techniques for the temple relevant for soft tissue filler augmentation procedures – Clinical anatomy and danger zones. Journal of Cosmetic Dermatology. 2020; 19:1570–1579.
- Casabona G, Frank K, Koban KC, et al. Lifting vs volumizing—The difference in facial minimally invasive procedures when respecting the line of ligaments. Journal of Cosmetic Dermatology. 2019; 18:1237–1243.
- Suwanchinda A, Rudolph C, Hladik C, et al. The layered anatomy of the jawline. Journal of Cosmetic Dermatology. 2018; 17:625–631.
- Casabona G, Frank K, Moellhoff N, et al. Full-face effects of temporal volumizing and temporal lifting techniques. Journal of Cosmetic Dermatology. 2020; 19:2830–2837.
- Othman S, Cohn JE, Burdett J, et al. Temporal Augmentation: A Systematic Review. Facial Plastic Surgery. 2020; 36:217–225.
- Machado Filho CDAS, dos Santos TC, Rodrigues APLJ, da Cunha MG. PolyLlactic acid: A biostimulating agent. Surgical and Cosmetic Dermatology. 2013; 5:345–350.
- Narins RS, Baumann L, Brandt FS, et al. A randomized study of the efficacy and safety of injectable poly-L-lactic acid versus human-based collagen implant in the treatment of nasolabial fold wrinkles. Journal of the American Academy of Dermatology. 2010; 62:448–462.
- Cohen S, Artzi O, Mehrabi JN, Heller L. Vectorial facial sculpting: A novel sub-SMAS filler injection technique to reverse the impact of the attenuated retaining ligaments. Journal of Cosmetic Dermatology. 2020; 19:1948–1954.
- Palm M, Weinkle S, Cho Y, et al. A Randomized Study on PLLA Using Higher Dilution Volume and Immediate Use Following Reconstitution. Journal of Drugs in Dermatology. 2021; 20:760–766.
- Bravo BSF, Carvalho R de M: Safety in immediate reconstitution of poly-L-lactic acid for facial biostimulation treatment. Journal of Cosmetic Dermatology. 2021; 20:1435–1438.
- Alessio R, Rzany B, Eve L, et al. European expert recommendations on the use of injectable poly-L-lactic acid for facial rejuvenation. Journal of Drugs in Dermatology. 2014; 13:1057–1066.
- Vleggaar D, Fitzgerald R, Lorenc ZP, et al. Consensus recommendations on the use of injectable poly-L-lactic acid for facial and nonfacial volumization. Journal of Drugs in Dermatology. 2014; 13:s44–s51.
- Haddad A, Menezes A, Guarnieri C, et al. Recommendations on the Use of Injectable Poly-L-Lactic Acid for Skin Laxity in Off-Face Areas. Journal of Drugs in Dermatology. 2019; 18:929–935.

