 J Clin Aesthet Dermatol. 2022;15(7):44-48.
J Clin Aesthet Dermatol. 2022;15(7):44-48.
by Yanisa Ratanapokasatit MD, MSc, and Punyaphat Sirithanabadeekul, MD
Both authors are with the Department of Dermatology, Chulabhorn International College of Medicine at Thammasat University in Pathum Thani, Thailand.
FUNDING: No funding was provided for this article.
DISCLOSURES: The authors report no conflicts of interest relevant to the content of this article.
ABSTRACT: Background. Epidermal growth factor (EGF) stimulates collagen production and supports the wound healing process. However, there are no studies on fractional carbon dioxide (CO2) laser combined with EGF for acne scar treatment.
Objective. We sought to evaluate the efficacy and safety of fractional CO2 laser combined with topical EGF versus fractional CO2 laser alone in the treatment of acne scars.
Methods. Twenty-three patients with atrophic acne scars underwent three monthly sessions of randomized split-face application of fractional CO2 laser combined with topical EGF or placebo twice daily for seven days following each laser session. Scar improvement was evaluated at one month and three months posttreatment by two blinded dermatologists and the Antera 3D® skin analysis system. Wound healing response and adverse events were also evaluated.
Results: Twenty-one patients completed the trial. According to dermatologist grading and skin analysis system, EGF showed significant superiority at three months posttreatment compared to placebo. The wound healing response did not differ between the groups. Surprisingly, the melanin index on the EGF side showed a significant decrease at three months posttreatment, compared to placebo. There was no allergic reaction to the topical EGF.
Conclusion: Treatment with topical EGF after ablative fractional CO2 laser improves the clinical appearance of atrophic acne scars, and EGF may help decrease skin pigmentation after laser treatment. The use of topical EGF is safe when applied to post-laser ablation.
Keywords: Epidermal growth factor, fractional carbon dioxide laser, acne scar
As a result of inflammatory acne and aberrant collagen production, atrophic acne scars are prevalent and regularly cause physical and psychological impacts. There are three subtypes of atrophic acne scars: icepick, rolling, and boxcar scars. At present, there are several approaches to treat this condition, including subcision, chemical peel, dermabrasion, laser treatment, punch procedure, microneeding, radiofrequency, and tissue augmentation, which are diverse in terms of therapeutic success and complications.1
Epidermal growth factor (EGF) is a single-chain acidic polypeptide with 53 amino acid residues and a molecular weight of 5,400 daltons.2 It is secreted by platelets, macrophages, fibroblasts, and bone marrow-derived mesenchymal stem cells and is found in most body fluids. EGF plays a vital role in stimulating the epithelium and fibroblast differentiation, enhancing collagen synthesis, and supporting the wound healing process.3 The current use of EGF varies between clinical and aesthetic fields. Topical EGF has been demonstrated to benefit diabetic foot ulcer conditions, demonstrating its increasing wound healing rate.4 EGF has also been used as a regenerating agent in aesthetics due to its effect in promoting collagen. Recent studies have shown that topical EGF can improve atrophic acne scars by enhancing collagen synthesis in EGF.5,6
Fractional CO2 lasers can emit energy to create numerous microthermal treatment zones in the skin and spare tissue surrounding it.7 The laser deploys a 10,600-nm wavelength of irradiation to selectively damage the specific chromophore, which is a water-containing tissue. Therefore, the stratum corneum, epidermis, and dermis can deteriorate. By inducing dermal injury and creating new collagen formation, this device demonstrated efficacy for treating atrophic acne scars. However, studies have shown varying levels of therapeutic outcomes, ranging from mild to moderate clinical improvement. In addition, some undesirable side effects, including redness, edema, and pigmentary alteration, persist.
To achieve the best clinical outcome and fewer side effects, topical EGF used in combination with fractional CO2 for atrophic acne scar treatment have been proposed in this study. Both of these factors can stimulate collagen synthesis. Besides, EGF might help lower the duration of scab shedding and unwanted side effects, such as erythema and edema, by promoting the wound healing process following laser treatment. Furthermore, several studies have shown that microchannels created by fractional laser through the skin can facilitate the penetration of applied topical drugs.8 For the first time, this study aimed to evaluate the efficacy and safety of topical EGF combined with a CO2 laser for atrophic acne scar treatment.
Methods
Patients. Twenty-three patients aged 18 to 50 years with Fitzpatrick Skin Types III to V and mild to severe atrophic acne scars were included. Patients with a history of keloid or hypertrophic scars, active facial inflammation, herpes labialis, skin cancer, diabetes mellitus, collagen vascular disease, allergy to topical EGF or anesthetic cream, oral isotretinoin use within the preceding six months, ablative or nonablative laser skin resurfacing within the preceding six months, and pregnancy or lactation were excluded. This was a randomized, split-face, controlled study. The study was conducted according to the principles of the 1975 Declaration of Helsinki and was approved by the Institutional Review Board of the Human Research Ethics Committee, Faculty of Medicine, Thammasat University. Written informed consent was obtained from all patients before conducting the study.
Treatment protocol. Local anesthetic cream, lidocaine 2.5% and prilocaine 2.5% cream was applied under occlusion 45 minutes prior to the procedure. Afterward, the whole face was cleansed and irradiated with a fractional CO2 laser (Smartxide Touch Fractionated CO2 Laser; Deka, Florence, Italy). Each treatment session used a smart stack scanning mode with a power of 15 W, HP emission mode, spacing of 700μm, Stack 2, pulse energy of 44.1mJ, and density of 10.4 percent. One pass of the laser was performed on the entire face. The second laser pass was then performed specifically over the scar area. Immediately after fractional CO2 laser, facial halves were randomly assigned to receive the application of topical EGF (Epidermal Growth Factor; Siam Bioscience Co., Ltd., Thailand) on one side and placebo on the other side, with full-face occlusion for 30 minutes. Concurrent air cooling and ice packs were used to minimize pain during and after the procedure. Topical EGF and placebo were administered twice daily for seven days following each laser session. All patients underwent three treatment sessions at monthly intervals. They were instructed to avoid direct sun exposure and to apply sunscreen with an SPF of 50. No prophylactic antibiotics or antivirals were administered.
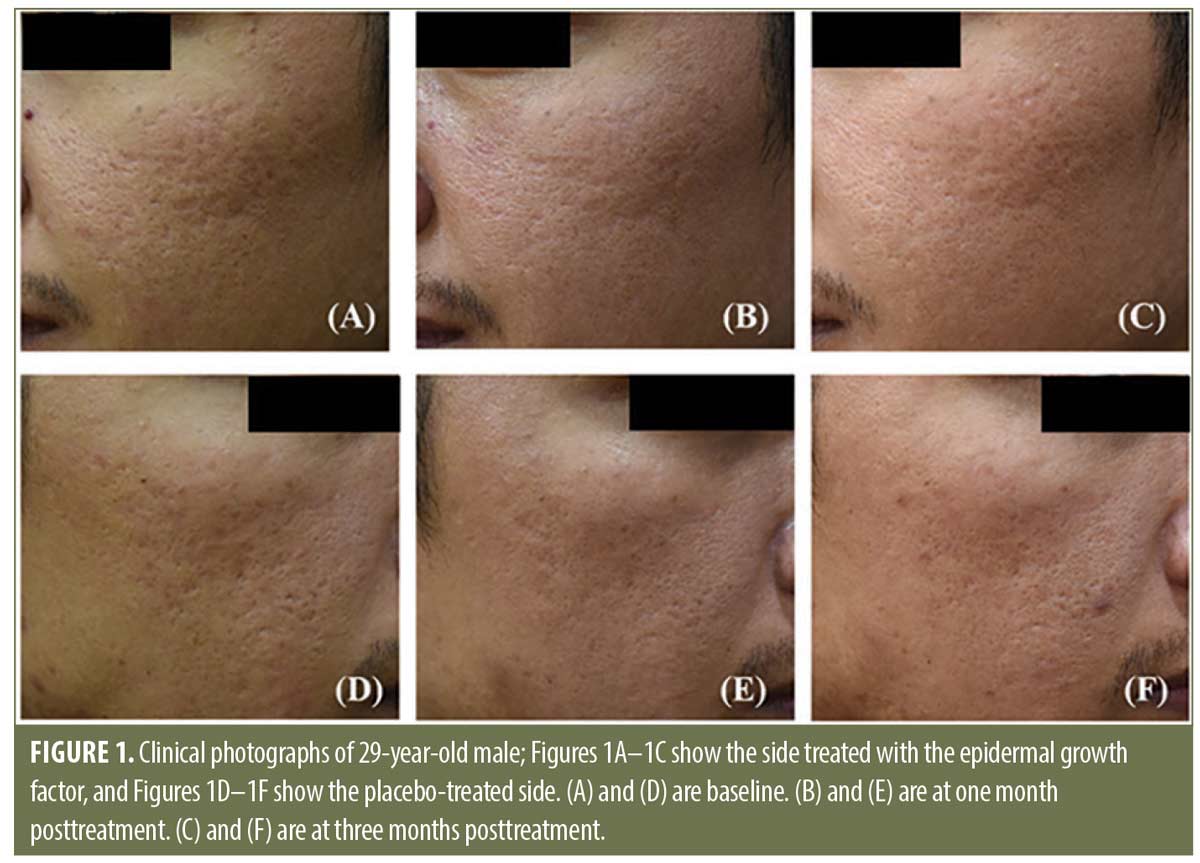
Evaluations. All patients were photographed at baseline, one month, and three months after the last treatment session (five months after starting therapy) using a digital camera (Nikon D750, Nikon Corp, Tokyo, Japan) and a skin analysis camera (Antera 3D®, Miravex Co., Ltd, Dublin, Ireland). Two blinded dermatologists evaluated overall scar improvement from photographs using a quartile grading scale (0=no improvement; 1=<25% improvement; 2=25 %–50% improvement; 3=51%–75% improvement; and 4=>75% improvement). The skin analysis camera was used as the objective measurement. Scar volume (mm3) was assessed, and percentages of scar volume reduction were evaluated and compared to the baseline. Wound healing response, including post-laser erythema and duration of scab shedding, was assessed by the investigator. Post-laser erythema was evaluated by clinical photographs at seven days after the first treatment session using a five-point scale (0=none, 1=trace, 2=mild, 3=moderate, 4=severe). The duration of scab shedding (days) was determined using patient-initiated photography. For safety profiles, side effects were recorded at every visit. The erythema and melanin indices were also assessed using the skin analysis camera at every visit. The overall patient satisfaction score, rated at four satisfactory levels as not satisfied, slightly satisfied, moderately satisfied, and extremely satisfied, was measured at one month and three months after the final laser.
Statistical methods. Descriptive data were presented as means, standard deviations, and percentages, as appropriate. A paired t-test was used to determine the numerical variables between the study groups. The Wilcoxon signed-rank test was used to compare two paired comparisons with the discrete data. Statistical significance was set at P<0.05. All statistical analyses were performed using SPSS version 19.0 (SPSS Inc., Chicago, Illinois).
Results
Twenty-one of the 23 patients who were initially enrolled completed the trial, 14 (67%) were male, and seven (33%) were female. Patients ranged in age from 23 to 39 years (mean age, 30.09 ± 4.67). Most of the patients were categorized as having Fitzpatrick Skin Type III (15 patients, 71.43%). The remaining six patients had Skin Type IV (28.57%). A mild degree of atrophic acne scars was observed in six patients (28.57%), a moderate degree in 11 patients (52.38%), and a severe degree in four patients (19.05%).
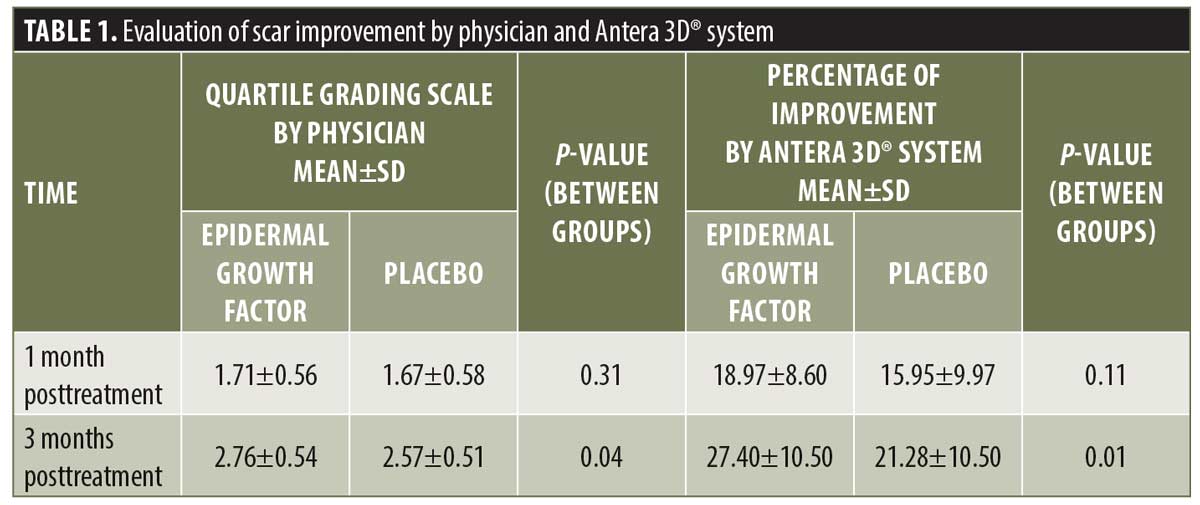
Efficacy. According to the physician’s assessment using a quartile grading scale, the area treated using fractional CO2 laser combined with topical EGF showed significantly better results at three months posttreatment (P=0.04) than the placebo side.
Corresponding to the Antera 3D® system, the percentage of scar volume improvement from the baseline was determined. For the EGF side, the mean percentages of improvement were 18.97±8.60 and 27.40±10.50 at one month and three months posttreatment, respectively. In contrast, the mean percentages of improvement for placebo side were 15.95±9.97 and 21.28±10.50, respectively. At three months posttreatment, the percentage of improvement of the EGF side was significantly higher than that of the placebo side (P=0.01).
For the evaluation of wound healing response, post-laser scab shedding of the EGF side was faster than that of the placebo side in two patients. The rest had an equal duration. Scab shedding ranged from 4 to 8 days. The average duration of scab shedding was 6.00±1.22 and 6.09±1.09 days, respectively, for EGF and placebo. There was no significant difference in the duration of scab shedding between the groups. For post-laser erythema, all patients showed no to trace erythema on Day 7. There was no difference in the five-point scale redness and erythema index between the EGF and placebo sides.
According to the patient satisfaction evaluation, most of the patients were moderately and extremely satisfied at one month and three months posttreatment in both groups. At the end of the study, 18 patients (85.71%) rated fractional CO2 laser combined with EGF as extremely satisfied. Three patients (14.29%) were moderately satisfied. In comparison, 17 patients (80.95%) and four patients (19.05%) rated their satisfaction with fractional CO2 laser followed by placebo as extremely satisfied and moderately satisfied, respectively.
Safety. Immediate post-laser erythema and edema were noted on both sides in all cases (100%). Crusting was resolved within 4 to 8 days. Erythema and edema were also reduced to no to trace levels within one week. No allergic reactions, acne, milia, or dermatitis were noted throughout the experiment. No infections were reported. For delayed complications, mild postinflammatory hyperpigmentation (PIH) was observed in two patients (9.52%) on both sides of their faces two months after initiation of the protocol. Topical whitening agents were prescribed. At the end of the study, the PIH was resolved. None of the participants experienced prolonged erythema, hypopigmentation, hypertrophic scarring, or ectropion formation.
For the erythema index, the Antera 3D® system showed a significant increase at one week and one month for both sides. Nevertheless, the average erythema index at three months posttreatment showed no significant difference from baseline in both groups. On the other hand, the average melanin index showed no significant increase at any time point. Surprisingly, the data showed a significant decrease in melanin index at three months posttreatment in the EGF side (P=0.04), compared to the placebo side.
Discussion
The pathogenesis of atrophic scarring following acne vulgaris is still not fully understood; however, the severity and duration of inflammatory acne are thought to be strongly associated with the development of scarring. In addition, scar formation is hypothesized to occur during the proliferative and matrix remodeling stages of wound healing due to abnormal collagen production and the imbalance between extracellular matrix metalloproteinases (MMPs) and tissue inhibitors of MMPs.9
Wound healing is a complex overlapping biological process that consists of numerous cell types, growth factors, cytokines, and chemokines. EGF is known to promote inflammatory responses, re-epithelialization, angiogenesis, and granulation tissue formation. It is essential for epidermal homeostasis and has been shown to stimulate the proliferation and migration of keratinocytes via MAPK/ERK1/2 signaling pathways, accelerating tissue repair in damaged skin.3,10,11 Furthermore, EGF is pro-mitotic for fibroblasts, stimulating their proliferation via the PI3K, Rac, and ERK-dependent signaling pathways, resulting in collagen deposition. This activity takes place during the wound healing process as well as during normal cellular development 3,5,6,12-15. Evidence for this role was provided in both in-vitro and in-vivo studies, which found that EGF promoted collagen deposition in a dose-dependent manner.12–14 Daily use of topical EGF in porcine partial-thickness wounds demonstrated a significant increase in the dermal thickness.12 EGF stimulated fibroblast proliferation and elevated procollagen mRNA contents in developing granulation tissue in rats.13 According to an in-vitro study, EGF also enhanced the expression of Type I collagen and Type III collagen.14
Among existing growth factor therapies, EGF has undergone the most research in humans. EGF is commercially available for wound healing, and it is the first growth factor that is accessible for skin rejuvenation in aesthetic fields.15,16 On the other hand, vascular endothelial growth factor (VEGF) is notable for its role of initiating angiogenesis.17 Platelet-derived growth factor (PDGF) is a potent chemoattractant for mesenchymal cells. However, of particular note, increased cancer risk has been reported in patients treated with more than three tubes of recombinant PDGF.18
Recently, several clinical studies have revealed that EGF stimulates collagen production and improves the appearance of acne scars, fine lines, rhytids, and skin texture.5,6,19 After a 12-week period of twice-daily treatment of topical EGF, atrophic acne scars significantly improved.5,6 Several subjects also reported improvements in wrinkles and overall skin consistency after EGF treatment.6,19
In our study, we used a fractional CO2 laser combined with topical EGF. The efficacy of scar improvement using this combination was superior to that of placebo in both physician grading and Antera 3D® measurements. The ablative fractional CO2 laser can create tissue vaporization and thermally induced dermal coagulation, leading to tissue contraction, collagen production, and dermal remodeling.20 Moreover, it can assist in drug delivery into the skin.21 Therefore, a synergistic effect of fractional CO2 laser and topical EGF was observed.
Considering the large molecular weight of EGF, factors that facilitate topical EGF absorption are hereby discussed. Microchannels created by fractional laser can deliver the topical administration of large molecules into the skin.22 Moreover, they are believed to act as reservoirs for drug accumulation for further diffusion. In addition to direct ablation, the fractional laser can elevate drug delivery by photomechanical wave and photothermal effect mechanisms.21,23
For the efficacy of post-laser wound healing response, the combination showed no significant difference compared to the placebo side. This is in accordance with a previous randomized split-face study, which demonstrated that the use of EGF-containing ointment after fractional CO2 laser showed no significant difference in duration of scab shedding, duration of post-laser erythema, erythema index, and transepidermal water loss on the daily follow up period of seven days, compared to placebo side.24 It is assumed that several mediators and growth factors are involved.21,25 Unlike chronic wounds, such as diabetic foot ulcers, EGF plays a crucial role in wound healing.
For the evaluation of safety, acute and delayed complications were not different between the two groups. There was no allergic reaction, acne, milia, or dermatitis to topical EGF throughout the experiment. Furthermore, according to a large number of preclinical studies, EGF does not cause genotoxicity, mutagenicity, or cytotoxicity.15 Therefore, the application of EGF to post-laser skin is considered safe.
Surprisingly, the current study showed a significant decrease in melanin index at three months posttreatment in the EGF side compared to the placebo side. Previous studies have proposed the mechanisms of EGF that are attributed to the reduction of melanin index as follows. EGF promotes wound healing and subsequently decreases inflammatory-induced melanogenesis. It reduces the tyrosinase activity of melanocytes through downregulation of microphthalmia-associated transcription factor. As a result, melanin synthesis decreases. These studies suggest that EGF may reduce the risk of PIH.26,27 An in-vitro study investigated the role of EGF in laser-treated conditioned cell culture media (LCM). It was shown that EGF treatment decreased the melanogenic effect and reduced tyrosinase activity in melanocytes.26 A split-side study evaluating the effect of EGF-containing creams following 532-nm Q-switched Nd:YAG laser showed that the incidence of PIH and melanin index was significantly lower in the EGF treated group compared to controls.27 Simultaneously, the prior studies also denoted the improvement in hyperpigmentation after the use of topical EGF.6,19
Conclusion
Treatment with topical EGF after ablative fractional CO2 laser synergistically improves the clinical appearance of atrophic acne scars, and EGF may help to decrease skin pigmentation after laser treatment. Lastly, topical EGF is safe when used for post-laser ablation. Further studies should include larger sample sizes and longer follow-up times. In addition, studies should extend to the effect of EGF on chronic wound healing and the combination of several growth factors for skin condition treatments. The application of EGF for wrinkle reduction, skin lightening, post-acne erythema prophylaxis, and acne scar prevention may be considered.
References
- Boen M, Jacob C. A Review and Update of Treatment Options Using the Acne Scar Classification System. Dermatol Surg. 2019;45(3):411–422.
- Boonstra J, Rijken P, Humbel B, et al. The epidermal growth factor. Cell Biol Int. 1995;19(5):413–430.
- Demidova-Rice TN, Hamblin MR, Herman IM. Acute and impaired wound healing: pathophysiology and current methods for drug delivery, part 2: role of growth factors in normal and pathological wound healing: therapeutic potential and methods of delivery. Adv Skin Wound Care. 2012;25(8):349–370.
- Yang S, Geng Z, Ma K, et al. Efficacy of topical recombinant human epidermal growth factor for treatment of diabetic foot ulcer: a systematic review and meta-analysis. Int J Low Extrem Wounds. 2016;15(2):120–125.
- Stoddard MA, Herrmann J, Moy L, et al. Improvement of atrophic acne scars in skin of color using topical synthetic epidermal growth factor (EFG) serum: a pilot study. J Drugs Dermatol. 2017;16(4):322–326.
- Seidel R, Moy RL. Improvement in atrophic acne scars using topical synthetic epidermal growth factor (EGF) serum: a pilot study. J Drugs Dermatol. 2015;14(9):1005–1010.
- Manstein D, Herron GS, Sink RK, et al. Fractional photothermolysis: a new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg Med. 2004;34(5):426–438.
- Braun SA, Schrumpf H, Buhren BA, et al. Laser-assisted drug delivery: mode of action and use in daily clinical practice. J Dtsch Dermatol Ges. 2016;14(5):480–488.
- Fabbrocini G, Annunziata MC, D’Arco V, et al. Acne scars: pathogenesis, classification and treatment. Dermatol Res Pract. 2010;2010:893080.
- Barrientos S, Stojadinovic O, Golinko MS, et al. Growth factors and cytokines in wound healing. Wound Repair Regen. 2008;16(5):585–601.
- Brown GL, Curtsinger L 3rd, Brightwell JR, et al. Enhancement of epidermal regeneration by biosynthetic epidermal growth factor. J Exp Med. 1986;163(5):1319–1324.
- Nanney LB. Epidermal and dermal effects of epidermal growth factor during wound repair. J Invest Dermatol. 1990;94(5):624-629.
- Laato M, Kähäri VM, Niinikoski J, et al. Epidermal growth factor increases collagen production in granulation tissue by stimulation of fibroblast proliferation and not by activation of procollagen genes. Biochem J. 1987;247(2):385-388.
- Shen T, Gao K, Miao Y, et al. Exogenous growth factors enhance the expression of cola1, cola3, and Elastin in fibroblasts via activating MAPK signaling pathway. Mol Cell Biochem. 2018;442(1-2):203-210.
- Berlanga-Acosta J, Gavilondo-Cowley J, López-Saura P, et al. Epidermal growth factor in clinical practice – a review of its biological actions, clinical indications and safety implications. Int Wound J. 2009;6(5):331-346.
- Aldag C, Nogueira Teixeira D, Leventhal PS. Skin rejuvenation using cosmetic products containing growth factors, cytokines, and matrikines: a review of the literature. Clin Cosmet Investig Dermatol. 2016;9:411-419.
- Yamakawa S, Hayashida K. Advances in surgical applications of growth factors for wound healing. Burns Trauma. 2019;7:10.
- Papanas N, Maltezos E. Benefit-risk assessment of becaplermin in the treatment of diabetic foot ulcers. Drug Saf. 2010;33(6):455-461.
- Schouest JM, Luu TK, Moy RL. Improved texture and appearance of human facial skin after daily topical application of barley produced, synthetic, human-like epidermal growth factor (EGF) serum. J Drugs Dermatol. 2012;11(5):613-620.
- Hunzeker CM, Weiss ET, Geronemus RG. Fractionated CO2 laser resurfacing: our experience with more than 2000 treatments. Aesthet Surg J. 2009;29(4):317-322.
- Hsiao CY, Yang SC, Alalaiwe A, et al. Laser ablation and topical drug delivery: a review of recent advances. Expert Opin Drug Deliv. 2019;16(9):937-952.
- Haak CS, Hannibal J, Paasch U, et al. Laser-induced thermal coagulation enhances skin uptake of topically applied compounds. Lasers Surg Med. 2017;49(6):582-591.
- Lin CH, Aljuffali IA, Fang JY. Lasers as an approach for promoting drug delivery via skin. Expert Opin Drug Deliv. 2014;11(4):599-614.
- Techapichetvanich T, Wanitphakdeedecha R, Iamphonrat T, et al. The effects of recombinant human epidermal growth factor containing ointment on wound healing and post inflammatory hyperpigmentation prevention after fractional ablative skin resurfacing: A split-face randomized controlled study. J Cosmet Dermatol. 2018;17(5):756–761.
- Ali FR, Al-Niaimi F. Laser-assisted drug delivery in dermatology: from animal models to clinical practice. Lasers Med Sci. 2016;31(2):373-381.
- Yun WJ, Bang SH, Min KH, et al. Epidermal growth factor and epidermal growth factor signaling attenuate laser-induced melanogenesis. Dermatol Surg. 2013;39(12):1903-1911.
- Park GH, Rhee do Y, Moon HR, et al. Effect of an epidermal growth factor-containing cream on postinflammatory hyperpigmentation after Q-switched 532-nm neodymium-doped yttrium aluminum garnet laser treatment. Dermatol Surg. 2015;41(1):131-135.

