Dear Editor:
Eyelid margin defects are produced by injuries, burns, bites, scars, and benign and malignant lesions. In most cases, adjoining tissues are involved, which require flaps and/or tissue grafts carried out by a skilled surgeon (Figures 1 and 2). The eyelid comprises three layers: the anterior layer is composed of skin and the obicularis muscle, the middle layer is composed of the orbital septum and the tarsal plate, and the posterior layer is composed by the conjunctiva and the lower eyelid retractors.

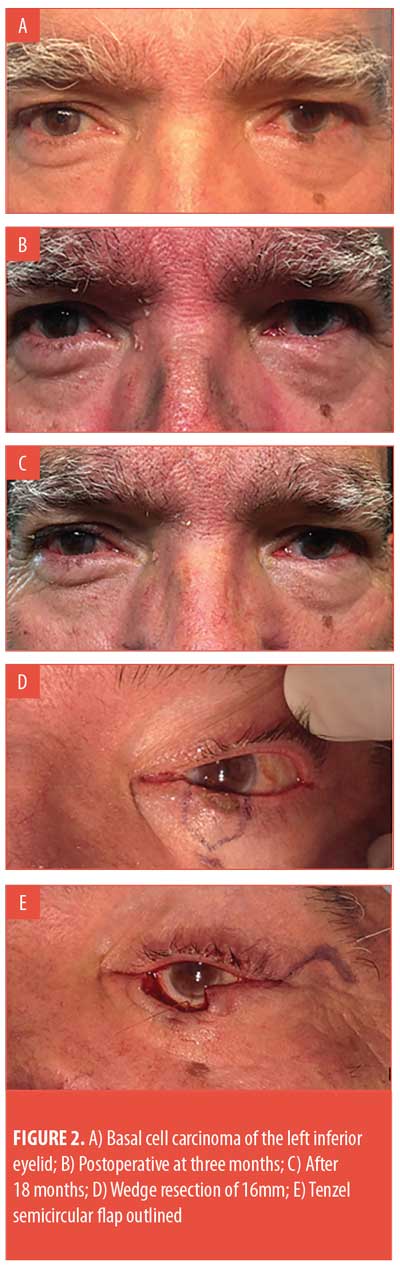
During the repair, each layer must be sutured with its corresponding layer on the opposing side of the incision. The traditional technique for eyelid margin repair (EMR) and its modifications uses three 6-0 silk sutures to join the cut ends of the eyelid margin.1–3 Another technique does not rely on margin sutures at all.4 In this technical note, the authors report their experience of over 20 years with the one-suture eyelid margin technique for EMR.
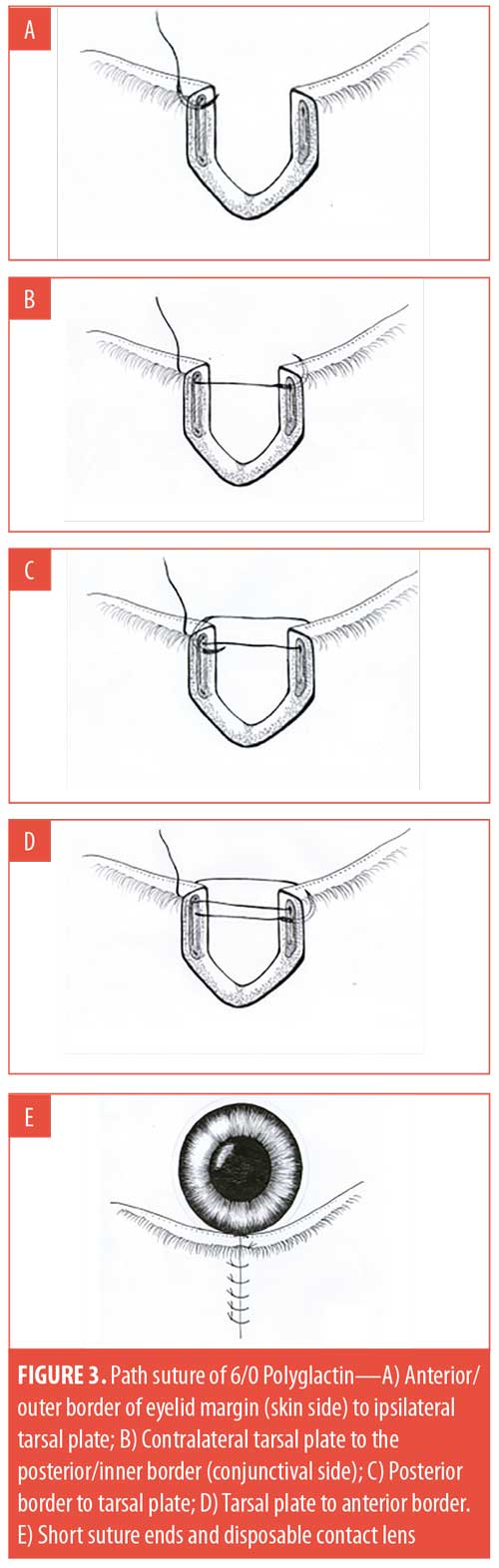
Once the eyeball has been carefully examined and any debris eliminated, a soft contact lens is inserted. To repair the eyelid margin lesion, first the adjoining tissues must be treated and then the lid margin must be sutured under magnification with an absorbable 6-0 Polyglactin suture (Figure 3). Topical antibiotic and steroid eye drops are used for 10 days, at which time the soft contact lens is removed.
With regard,
Jorge Schwember, MD; Gerardo Schwember, MD, Phd; and Luisa Madrid, MD
Drs. J. Schwember and Madrid are with Centro Laser in La Serena, Chile. Dr. G. Schwember is with Clínica Alemana de Santiago and Hospital Padre Hurtado de Santiago in Santiago, Chile.
Acknowledgments. The authors would like to acknowledge Paulina Vildosola for her drawings (Figure 3).
Disclosures. The author has no conflicts of interest relevant to the content of this article.
Correspondence. Jorge Schwember, MD; Email: jschwember@centrolaserlaserena.cl
References
- Mustarde JC. Repair and reconstruction in the orbital region. 1st ed. Edinburgh, Scotland: E & S Livingstone Ltd;1966:100–104.
- Perry JD, Aguilar CL, Kuchtey R. Modified vertical mattress technique for eyelid margin repair. Dermatol Surg. 2004;30:1580–1582.
- Custer PL, Vick V. Repair of marginal eyelid defects with 7-0 chromic sutures. Ophthal Plast Reconstr Surg. 2006;22:256–258.
- Willey A and Caesar RH. Diagonal tarsal suture technique sine marginal sutures for closure of full-thickness eyelid defects. Ophthalmic Plast Reconstr Surg. 2013;29(2):137–138.

