 by Elizabeth Ethington, MD; Andia Mitri, BS; David Surprenant, MD; Michael Murphy, BS; Rebecca Rovner, MD; Jeave Reserva, MD; James Swan, MD; William Adams, PhD; Rebecca Tung, MD; and Kristin Lee, MD
by Elizabeth Ethington, MD; Andia Mitri, BS; David Surprenant, MD; Michael Murphy, BS; Rebecca Rovner, MD; Jeave Reserva, MD; James Swan, MD; William Adams, PhD; Rebecca Tung, MD; and Kristin Lee, MD
Drs. Ethington, Surprenant, Rovner, Reserva, Swan, Lee, and Mr. Murphy are with the Divison of Dermatology at Loyola University in Maywood, Illinois. Ms. Andia is with the Stritch School of Medicine at Loyola University in Maywood, Illinois. Dr. Adams is with the Department of Public Health Sciences, Loyola University, in Maywood, Illinois. Dr. Tung is with Florida Dermatology and Skin Cancer Centers in Florida.
FUNDING: No funding was provided for this study.
DISCLOSURES: The authors have no conflicts of interest relevant to the content of this article.
ABSTRACT: Background.Seborrheic keratoses (SKs) are one of the most common benign epithelial tumors seen by dermatologists. Many people elect to have these lesions removed, most commonly by way of cryosurgery or electrodesiccation.
Objective.We sought to evaluate the comparative efficacy and patient preferences regarding cryosurgery and electrodesiccation for the treatment of truncal SK lesions.
Methods. In this randomized, blinded clinical trial, 33 eligible subjects with two similar truncal SKs were assigned to receive treatment with cryosurgery and electrodesiccation applied to separate lesions. Patients rated their pain and preference at the time of treatment and follow up at two and eight weeks. Physicians rated the color, texture, and efficacy of lesion removal at eight weeks.
Results. Patients did not have a treatment preference (p=0.10) and there was no significant difference in pain when comparing cryosurgery to electrodesiccation (p=0.43). Both treatment modalities were similar in terms of efficacy (p=0.50). Skin texture was rated similarly (p=0.64); however, lesions treated with cryosurgery were nominally less likely to have posttreatment hyperpigmentation compared to lesions treated with electrodesiccation (odds ratio: 0.35, 95% confidence interval: 0.12–1.002; p=0.0504).
Conclusion.Cryosurgery and electrodesiccation are both effective treatment modalities for truncal SKs. While cosmetic outcomes were similar, cryosurgery resulted in less postinflammatory hyperpigmentation.
KEYWORDS: Seborrheic keratoses, cryosurgery, electrodesiccation
J Clin Aesthet Dermatol. 2019;12(9):E53–E56
Seborrheic keratoses (SKs) are the most common benign epithelial tumors, impacting about 83 million Americans.1 The lesions increase in incidence with age and are typically found on the face, neck, and trunk. SKs present as hyperpigmented papules or plaques with a waxy, “stuck-on” hyperkeratotic surface and can range in size.1 The etiology and pathogenesis of these benign skin tumors continues to be poorly understood. However, it is known that SKs exhibit lower apoptosis rates compared to normal skin, resulting in an altered balance between cell proliferation and loss.2 Although dermatologists can easily recognize and assure patients that these lesions are benign, many patients desire removal. Motivations behind elective treatment of these benign lesions are mostly cosmetic, but can include concern of future malignancy, pruritus, and irritation. As the baby boomer generation is now reaching the age where SKs are more common, dermatologists are frequently consulted for the removal of these lesions to uphold a youthful appearance.3
Despite the high prevalence and frequency with which patients seek evaluation by a dermatologist, there is limited literature regarding this condition and approved treatment options, and a lack of well controlled clinical trials that assess the efficacy and safety of currently available treatment options. Case reports in the literature describe the use of diclofenac gel,4 imiquimod,5 debesilate,6 calcitriol,7 and acitretin8 in the management of SK lesions. Cryotherapy, curettage, and ablative lasers are the traditional therapies employed in the treatment of SK lesions.3 One comparative clinical study revealed that patients preferred cryotherapy rather than curettage, despite a statistically significant higher level of pain associated with cryotherapy.9 This preference was largely due to decreased wound care responsibilities with cryotherapy. Blinded physician ratings at follow up also demonstrated superior cosmetic outcome with cryotherapy in terms of pigmentation at treatment site.
The efficacy of cryotherapy has been compared to that of erbium-doped yttrium aluminum garnet (Er:YAG) laser therapy. SK lesions treated with Er:YAG laser had better postprocedure cosmetic outcomes and demonstrated faster healing rates (100% healing rate with Er:YAG lasers vs. 68% with cryotherapy).10 A novel topical 40% hydrogen peroxide (H?O?) solution was recently approved for the treatment of SKs.11 Kao et al12 compared topical 40% H?O? with cryosurgery, specifically evaluating skin architecture, metabolic activity, and cytotoxicity, with an emphasis on melanocytes. Their study used a validated ex-vivo human reconstituted full-thickness model derived from Fitzpatrick V skin. Cryosurgery was found to be more cytotoxic and have higher posttreatment pigmentary alterations compared to H?O?.12 The H?O? solution at 40% concentration exhibited superior efficacy in treating facial SKs compared to the lower-concentration solution (32.5%).13 In patients who do not wish to undergo invasive or tissue-destructive procedures, a novel aqueous solution containing nitric acid, zinc and copper salts, and organic acids might also be a promising alternative. One study demonstrated a complete response in 37 out of 50 SK lesions following an average of three applications per lesion.14
Two effective treatment modalities that we commonly use for the resolution of SKs are cryosurgery and electrodesiccation. However, negative features of these techniques include pain, the need for local anesthetic, scarring, and, particularly in patients with dark skin, hyperpigmentation. Our objective in this study was to investigate the comparative efficacy and patient preference of cryosurgery and electrodesiccation in the removal of truncal SKs.
Methods
Thirty-three adults with SKs were enrolled in our study. Patients were excluded if they had a history of keloids or hypertrophic scars, were smokers, had an implanted cardiac device (e.g., pacemaker, defibrillator), or were allergic to local anesthetics or adhesive bandages. The study was approved by the Loyola University Medical Center institutional review board and patients provided written informed consent.
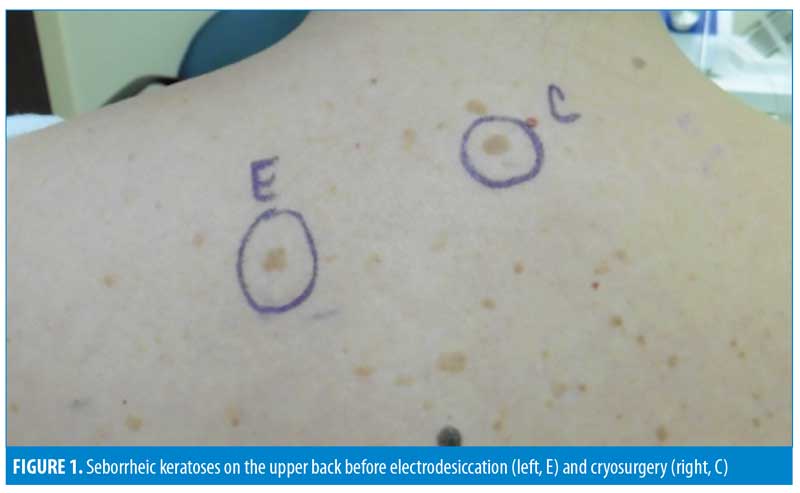
The study was a randomized clinical trial wherein the units of observation were noninflamed SK lesions. Each participant contributed two lesions to the analysis (Figure 1). The left lesion was assigned to cryosurgery or electrodesiccation using a 1:1 block randomization scheme; the opposite procedure was used on the right lesion. Lesions treated with electrodesiccation were first cleaned with alcohol and then anesthetized with 0.5cc of lidocaine 1%, with 1:100,000 epinephrine. These lesions were then treated with a fine-tipped monopolar electrode, which was connected to an electrosurgical generator unit (ConMed, Utica, New York). This device was set to a low setting (3 to 6) and lesions were treated until the endpoint of mild gray char and crusting was achieved. The crust was left in place as a natural wound dressing. Conversely, lesions undergoing cryotherapy were treated using liquid nitrogen spray for 10 seconds or less via a handheld device (Cry-Ac®; Brymill, Ellington, Connecticut) to ensure complete freezing within the boundaries of the lesion. After treatment, all lesions were cleansed with normal saline and covered with a thin hydrocolloid dressing (DuoDERM® Extra Thin Dressing; ConvaTec, Deeside, United Kingdom). Subjects were instructed to leave the dressing in place for one week and then to proceed with dressing changes by cleansing with a gentle cleanser and rinsing with water, followed by the application of petrolatum and a bandage until the lesion was completely healed.
Response measures. Immediately following the surgery, patients rated their pain for each lesion on a 10-point ordinal scale, ranging from 1 (no pain) to 10 (extreme pain), and noted their preference for cryosurgery, electrodesiccation, or both. At two and eight weeks later, patients were asked again to report their preference for cryosurgery or electrodesiccation (or both). At the eight-week follow-up visit, a blinded physician rated the color of both lesions on a 10-point ordinal scale, ranging from -5 (hypopigmentation) to +5 (hyperpigmentation). The blinded physician also rated the texture of both lesions on a 10-point ordinal scale, ranging from 1 (flat) to 10 (most elevated). Finally, a blinded physician rated the effectiveness of lesion removal on a three-point ordinal scale that included the anchors not effective, partially effective, and effective.
Statistical methods. Power for this trial was supported by Wood et al.15 In their study using a standard ordinal cosmesis scale that ranged from 1 (no change in lesion) to 10 (normal appearing skin) points, the mean rating at the six-week follow-up visit was 8.58 for cryotherapy versus 8.28 for curettage. Based on these estimates, a sample size of 34 can achieve 80 percent power to detect a mean difference in paired hyperpigmentation scores of 0.30 between cryotherapy versus electrodesiccation at the eight-week follow-up visit. This computation assumed an estimated standard deviation of the difference score of 0.59 and a significance level (alpha) of 0.05 using a two-sided Wilcoxon test.
For the pain outcome, a generalized linear mixed-effects model was used to estimate the odds of a higher pain score for cryosurgery versus electrodesiccation. This multivariable model controlled for lesion size and depth and specified a multinomial distribution with cumulative logit link for the pain response. Because patients contributed multiple lesions (i.e., multiple pain scores) to the analysis, random intercepts were allowed for each participant using an unstructured covariance matrix to account for their within-subject correlation. In these comparisons, a Kenward–Roger correction was used to adjust the denominator degrees of freedom.16 A similar approach was used for the physician pigmentation scores, elevation scores, and effectiveness scores.
Regarding patients’ preference for cryosurgery, electrodesiccation, or both procedures, these responses were recorded at baseline, two weeks, and eight weeks postprocedure. Therefore, a univariable generalized linear mixed-effects model was used to estimate the odds of preferring cryosurgery, electrodesiccation, or both procedures as a function of elapsed time. This model specified a multinomial distribution with a generalized logit link for the response and, as before, random intercepts were allowed for each participant to account for their within-subject correlation; a Kenward–Roger correction was used to adjust the denominator degrees of freedom. All analyses were completed using SAS version 9.4 (SAS Institute, Cary, North Carolina), and the study was approved by the Loyola University Stritch School of Medicine Institutional Review Board.
Results
Thirty-three patients were included in this trial. Most patients were female (70%) and identified as non-Hispanic white (97%); only one patient (3.0%) identified as Black or African-American. Regarding Fitzpatrick Skin Type, one patient (3.0%) was Type I, 30 patients (91%) were Type II, one patient (3.0%) was Type III, and one patient (3.0%) was Type V.
Seventeen (52%) patients were randomized to receive electrodesiccation on the left SK lesion and cryosurgery on the right SK lesion. In this cohort, the average lesion size for the electrodesiccation procedure was 8.82mm (standard deviation [SD]: 4.49mm), while the average depth for the same lesion was 0.91 mm (SD: 0.48mm). For the cryosurgery lesion, the average lesion size was 8.71mm (SD: 3.90mm) and the average depth was 0.85mm (SD: 0.39mm). The remaining 16 (48%) patients were randomized to receive electrodesiccation on the right SK lesion and cryosurgery on the left SK lesion. In this cohort, the average lesion size for the electrodesiccation procedure was 8.31mm (SD: 2.52mm), and the average depth for the same lesion was 0.87mm (SD: 0.50mm); for the cryosurgery lesion, the average lesion size was 9.00mm (SD: 2.71mm) and the average depth was 0.84mm (SD: 0.39mm).
Among lesions treated with cryosurgery (k=33), the median pain score immediately following the procedure was 3 (interquartile range [IQR]: 2–4; range: 1–7), while, among lesions treated with electrodesiccation (k=33), the median pain score was 2 (IQR: 1–3; range: 1–8). Controlling for lesion size and depth, there was no significant difference in the odds of a higher pain score between lesions treated with cryosurgery versus electrodesiccation (odds ratio [OR]: 1.43, 95% confidence interval [CI]: 0.58–3.52; p=0.43).
Regarding the preferred procedure, 32 patients reported their preference for cryosurgery versus electrodesiccation immediately after the procedure. Among these patients, 13 (41%) preferred electrodesiccation, 10 (31%) preferred cryosurgery, and nine (28%) liked both procedures equally. Two-weeks later, all 33 patients reported their preferred procedure, including 19 (57%) who preferred electrodesiccation and 11 (33%) who preferred cryosurgery; three (9.1%) patients reported liking both procedures equally at this visit. At the eight-week follow-up visit, 31 patients reported their preference, including 16 (52%) who preferred cryosurgery and 12 (39%) who preferred electrodesiccation, while three (9.7%) patients continued to like both procedures equally at this visit. Overall, patient preference for electrodesiccation versus cryotherapy was comparable at baseline (Week 0), two weeks, and eight weeks following the procedure (overall model p=0.10).
At the eight-week follow-up visit, the median pigmentation score for lesions treated with cryosurgery was 5 (IQR: 4–5; range: 1–10) and the median pigmentation score for lesions treated with electrodesiccation was 5 (IQR: 5–6; range: 1–8). Controlling for lesion size and depth, lesions treated with cryosurgery were only 0.35 (95% CI: 0.12–1.002) times as likely to have higher hyperpigmentation scores compared to those treated with electrodesiccation (Figures 2 and 3), though this finding was not statistically significant (p=0.0504). Regarding texture, the elevation score for lesions treated with cryosurgery (Mdn: 1; IQR: 1–2; range: 1–10) was comparable with that of those treated with electrodesiccation (Mdn: 1; IQR: 1–3; range: 1–9). In fact, controlling for lesion size and depth, there was no difference in the odds of a higher elevation score between cryosurgery versus electrodesiccation (OR: 0.76, 95% CI: 0.24–2.41; p=0.64).


Finally, among the 31 cryosurgery lesions evaluated at the eight-week follow-up appointment, 25 (81%) were deemed effectively removed by the blinded physician, two (6.5%) were deemed partially effectively removed, and four (13%) were deemed ineffectively removed. This was comparable to the rates for the 31 electrodesiccation lesions evaluated at the eight-week follow-up appointment, including 25 (81%) that were deemed effectively removed, five (16%) that were deemed partially effectively removed, and one (3.2%) that was deemed ineffectively removed. Controlling for lesion size and depth, there was no difference in the odds of a higher efficacy score between lesions treated with cryosurgery versus electrodesiccation (OR: 0.61, 95% CI: 0.14–2.62; p=0.50).
Discussion
In this study, we evaluated the effectiveness and cosmetic outcomes following treatment of noninflamed SKs with cryosurgery and electrodesiccation. Most patients did not have a preference regarding treatment modality, and there was no significant difference in pain perception between the procedures. There was a nominal difference in pigmentation that favored cryosurgery over electrodesiccation, though the finding was not statistically significant. Our results suggest that cryotherapy might be associated with less postinflammatory hyperpigmentation compared to electrodesiccation.
The primary limitation of this study was that most patients (91%) had Fitzpatrick Type II skin. While postinflammatory hyperpigmentation after procedures can occur in all skin types, it is most concerning for patients with darker Fitzpatrick Skin Types (III–V). Postinflammatory hyperpigmentation is a consequence of increased melanin production secondary to postinflammatory cytokine secretion; that is, the melanin is abnormally relocated to the dermis and surrounded by macrophages in the papillary dermis.17 Our results suggest that cryotherapy might be a better treatment modality than electrodesiccation in individuals who are more prone to postinflammatory hyperpigmentation. However, since SKs vary in their properties and locations, and our results might not be able to be generalized to all SK cases. Additionally, results after cryotherapy can vary depending on operator technique.
Our findings are in line with and add to the limited data available in the literature. Although SKs are one of the most common reasons for dermatologic consultation, there remains a paucity of data and research on available treatments and comparative outcomes.
Conclusion
In this study, both cryotherapy and electrodesiccation were similarly successful in the removal of noninflamed SKs. Cryotherapy might be associated with less postinflammatory hyperpigmentation compared to electrodesiccation.
References
- Bickers DR, Lim HW, Margolis D, et al. The burden of skin diseases: 2004 a joint project of the American Academy of Dermatology Association and the Society for Investigative Dermatology. J Am Acad Dermatol. 2006;55(3):490–500.
- Simionescu O, Popescu BO, Costache M, et al. Apoptosis in seborrheic keratoses: an open door to a new dermoscopic score. J Cell Mol Med. 2012;16(6):1223–1231.
- Jackson JM, Alexis A, Berman B, et al. Current understanding of seborrheic keratosis: prevalence, etiology, clinical presentation, diagnosis, and management. J Drugs Dermatol. 2015;14(1):1119–1125.
- Akta? H, Ergin C, Kesero?lu HÖ. Diclofenac gel may be a new treatment option for seborrheic keratosis. Indian Dermatol Online J. 2016;7(3):211–212. 5.
- Karadag AS, Ozlu E, Uzuncakmak TK, et al. Inverted follicular keratosis successfully treated with imiquimod. Indian Dermatol Online J. 2016;7(3):177–179.
- Cuevas P, Angulo J, Salgüero I, Giménez-Gallego G. Clearance of seborrhoeic keratoses with topical dobesilate. BMJ Case Rep. 2012;2012 .
- Lu’o’ng Kv, Nguyn LT. The roles of vitamin D in seborrhoeic keratosis: possible genetic and cellular signaling mechanisms. Int J Cosmet Sci. 2013;35(6):525–531.
- Thyssen JP, Zachariae C. Successful treatment of multiple seborrheic keratoses using acitretin. J Eur Acad Dermatol Venereol. 2007;21(2):269–270.
- Wood LD, Stucki JK, Hollenbeak CS, Miller JJ. Effectiveness of cryosurgery vs. curettage in the treatment of seborrheic keratoses. JAMA Dermatol. 2013;149(1):108–109.
- Gurel MS, Aral BB. Effectiveness of erbium:YAG laser and cryosurgery in seborrheic keratoses: randomized, prospective intraindividual comparison study. J Dermatolog Treat. 2015;26(5):477–480.
- Draelos ZD, Kempers S, Smith SR, et al. Safety and efficacy of A-101 hydrogen peroxide topical solution in adults with seborrheic keratosis: results from the phase 3, randomized double-blind, vehicle-controlled, parallel-group study. Skin J Cutan Med. 2017;1:s119.
- Kao SK, Kiss A, Efimova T, Freidman A. Ex vivo evaluation of cytotoxicity and melanocyte viability after A-101 hydrogen peroxide topical solution 40% or cryosurgery treatment in seborrheic keratosis lesions. J Am Acad Dermatol. 2018;79(4):767–768.
- Dubois JC, Jarratt M, Beger BB, et al. A-101, a Proprietary topical formulation of high concentration hydrogen peroxide solution: a randomized, double-blind, vehicle controlled, parallel group study of the dose- response profile in subjects with seborrheic keratosis of the face. Dermatol Surg. 2018;44(3):330–340.
- Lacarrubba F, Nasca MR, Verzi AE, Micali G. A novel topical agent in the treatment of seborrheic keratoses: A concept study by clinical and dermoscopic evaluation. Dermatol Ther. 2017;30(5).
- Wood, LD, Stucki JK, Hollenbeak CS, Miller JJ. Effectiveness of cryosurgery vs curettage in the treatment of seborrheic keratoses. JAMA Dermatol. 2013;149(1):108–109.
- Kenward MG, Roger JH. Small sample inference for fixed effects from restricted maximum likelihood. Biometrics. 1997;53(3):983–997.
- Brenner M, Hearing VJ. Modifying skin pigmentation – approaches through intrinsic biochemistry and exogenous agents. Drug Discov Today Dis Mech. 2008;5(2):e189–e199.

