 J Clin Aesthet Dermatol. 2020;13(7):E58–E63
J Clin Aesthet Dermatol. 2020;13(7):E58–E63
by Patrícia Froes Meyer, PhD; Rodrigo Marcel Valentim da Silva, DO; Eneida de Morais Carreiro, MD; Bruna S. da Costa, BA; Débora Freire, BA; Júlio Davi Costa e Silva, BA; Stephany L. Queiroga Farias, BA; Rafaella Rêgo Maia, BA; Liliane Santos de Vasconcellos, MD; and Graziele Maia Alves Serafim, MD
Drs. Meyer, da Silva, and Vasconcellos and Ms. Maia are with the Federal University of Rio Grande do Norte (UFRN) in Natal, Rio Grande do Norte, Brazil. Ms. Da Costa, Freire, and Farias and Mr. Costa e Silva are with Potiguar University (UNP) in Natal, Rio Grande do Norte, Brazil. Dr. Serafim is with Pontifical Catholic University of Minas Gerais (PUC-MG) in Belo Horizonte, Minas Gerais, Brazil. Drs. Meyer and Carreiro are with the University Centre of Rio Grande do Norte (UNI-RN) in Natal, Rio Grande do Norte, Brazil.
FUNDING: No funding was provided for this study.
DISCLOSURES: The authors have no conflicts of interest relevant to the content of this article.
ABSTRACT: Background. Cryofrequency combines cryotherapy with radiofrequency, reaching the tissue in different layers, providing various biological effects, and reducing localized adiposity.
Objective. We sought to evaluate the efficacy of cryofrequency in reducing localized adiposity.
Methods. The study population consisted of 63 women with infra-abdominal adiposity, evaluated before and after treatment using evaluation protocols, questionnaires, and ultrasound imaging. The volunteers were randomly distributed into three subgroups; of these, Group 1 (G01) received the cryofrequency treatment (temperature of –10°C, 85% power); Group 2 (G02) underwent cryofrequency associated with ultracavitation (frequency of 60 Hz, 70% power, shooting at 25%, duty cycle of 60% on and 40% off); and the control group (CG) received cryotherapy alone (temperature of –10°C). All groups were submitted to four treatment sessions, one session per week.
Results. The reduction in the fat layer analyzed by ultrasonography showed that the right side of G01 presented a significant difference in comparison with CG (p=0.01); a significant difference was also observed in the comparison between the G01 and G02 groups (p=0.001). Considering the left side, significant differences were observed in G01 when compared with CG (p=0.01) and between G01 and G02 (p=0.001). The variables of plicometry and perimetry presented a significant difference relative to in CG; however, no differences were observed with regard to weight or body mass index (p>0.05). The majority of participants reported positive feelings about the treatment.
Conclusions. The cryofrequency protocol alone led to a significant reduction in the fat layer but its association with ultracavitation led to superior results.
Keywords: localized fat, cryofrequency, ultracavitation
Localized adiposity is an aesthetic concern that occurs in connective adipose tissue due to abnormal growth of unilocular adipose cells (i.e., hypertrophy). It is caused by an imbalance between ingestion and energy expenditure and is characterized by the accumulation of fat in specific regions of the body. In women, this accumulation mainly affects the hip, the obliques, the abdomen, and the thighs.1,2
There is a growing demand for noninvasive body aesthetic procedures, which aim to minimize the disadvantages associated with surgery, such as complications and recovery time, which require special care. In this way, cryofrequency, resulting from the combination of cryotherapy and radiofrequency, facilitates the treatment of different aesthetic changes, such as localized fat and sagging, while promoting greater patient comfort during the treatment application.3,4
Cryofrequency works by incorporating temperature-emitting technology. The tip of the device cools the skin surface down to about -10°C for the protection of cutaneous tissue, whereas the heat emitted by the radiofrequency aspect reaches deeper layers, stimulating long-term neocolagenesis and neoelastogenesis, apart from promoting lipolysis. The energy released from this electrode leads to better circulatory and nutrient supply, increased oxygenation, and tissue hydration and accelerates the elimination of catabolites, favoring lipolysis, the contraction of the connective tissue, and the contraction of the collagen fibers to simultaneously provoke multiple changes in the external structure of the skin.4,5
Although cryofrequency’s mechanisms of action are still not fully understood, some studies have reported promising results in the treatment of aesthetic concerns without significant adverse effects.6,7 Thus, the present study aimed to evaluate the efficacy of cryofrequency in the reduction of localized adiposity by comparing its effects to different treatment groups using evaluation protocols, questionnaires, and ultrasound imaging.
Materials and Methods
This was an experimental, randomized controlled study approved by the ethics committee of Potiguar University (registration no. 3.205.346) and conducted following the recommendations of the Consolidated Standards of Reporting Trials. All volunteers signed a informed consent form before the study began and treatment was performed by a trained physiotherapist at the Dr. Eneida Carreiro Clinic (Natal, RN, Brazil). The simple randomization consisted of lot drawing of envelopes that contained a response card, which indicated the group to which the participant would be allocated. The group allocation sequence was followed according to a computer-generated list. The intervention was tested in comparison with the control group and among the treated groups using an analysis of independent groups.
Participants. This clinical study evaluated 63 women aged 45 and 60 years and weighing between 55 and 73kg who presented with infra-umbilical localized adiposity. The inclusion criteria were female sex, age between 30 and 60 years, the presence of infra-umbilical localized adiposity, good comprehension capacity, preserved local sensibility, and no circulatory changes. Meanwhile, the exclusion criteria included an adipose layer thickness of less than 1cm or greater than 4cm, cold hypersensitivity, use of a pacemaker, reported dermatitis, epilepsy, cancer, the use of corticosteroids, the presence of metal and/or silicone implants in the treated area, and disagreement with the procedures or an inability to adapt to the schedules and techniques of the study.
Study volunteers were stratified into three subgroups by lot drawing as follows: a control group (CG), with 21 participants with a mean age of 23.5 years (± 1.2 years) and mean weight of 58.7 kg (± 7.88 kg); the cryofrequency group (G01), with 21 participants with a mean age of 22.9 years (± 2.1 years) and mean weight of 63.73 kg (± 7.38 kg); and a cryofrequency associated with ultracavitation groups (G02), with 21 participants with a mean age of 21.5 years (± 1.6 years) and mean weight of 65.54 kg (± 7.4 kg).
Evaluation procedures. All participants were submitted to an anthropometric evaluation and to ultrasonographic measurements, which were performed pretreatment and at one week after the final session. An ultrasound device (Eco palm Wi-fi, 10 MHz; China), a semi-professional camera (SX530 HS; Canon, Tokyo, Japan), a tape measure, an adipometer (Sanny, São Paulo, Brazil), a bathroom scale (Accumed-Glicomed, Rio de Janeiro, Brazil), and a cryofrequency apparatus (BHS 156 Full; Body Health, Brazil).
The data-collection instruments used in this research included the Protocol of Physical Therapy Evaluation in Localized Adiposity, which was previously validated by Meyer et al.8 as an instrument for collecting information concerning identification, anamnesis, life habits, physical examination via measurements and assessments such as weight, height, body mass index (BMI), skinfolds, and abdominal circumference. The skinfolds of the infra-umbilical region were measured three times, 2cm below the umbilical scar, with the final result based on the mean value obtained with the measurements. The measuring of the abdominal circumference was performed 5cm below the umbilical scar.
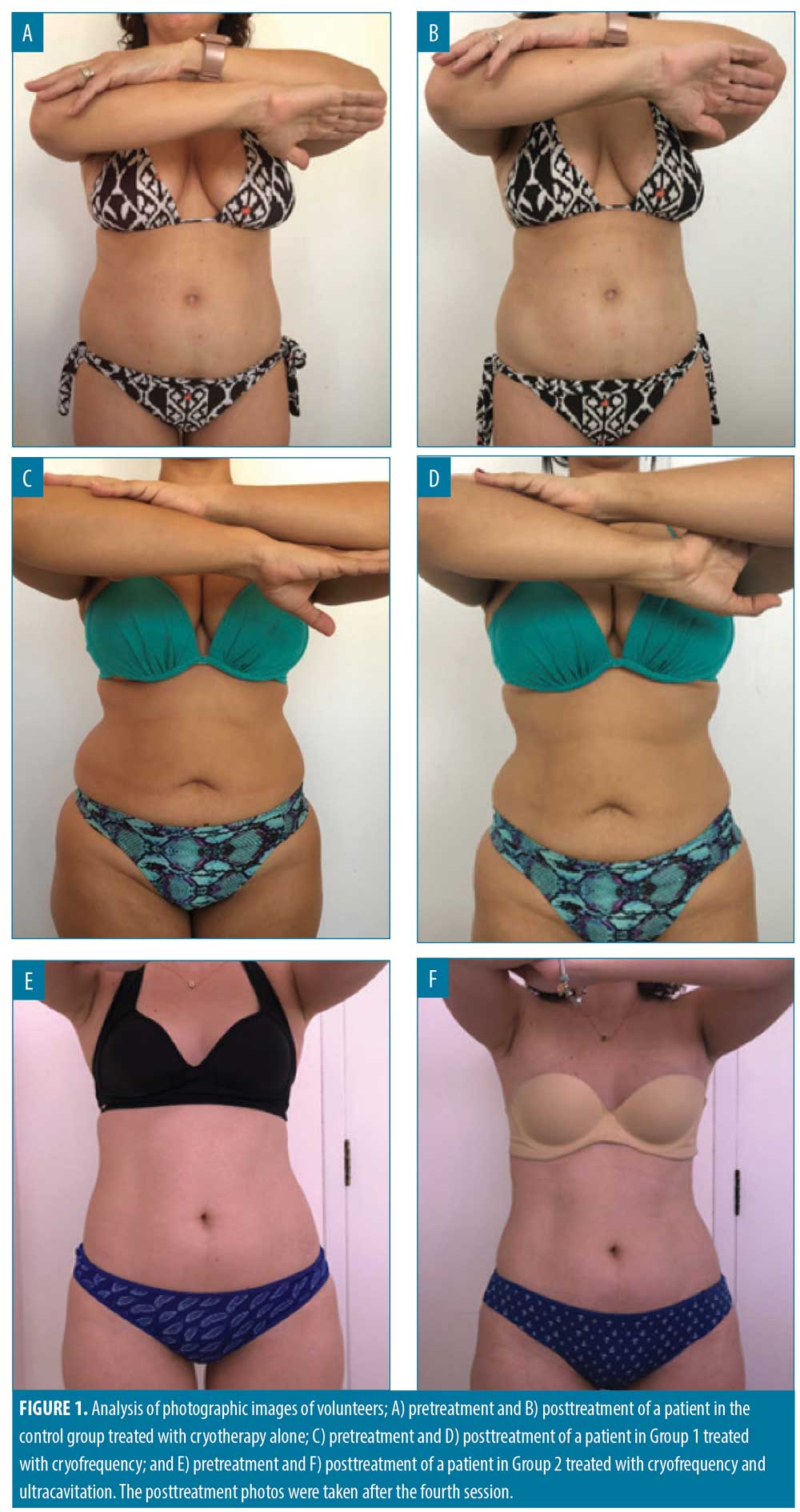
Photographs were taken from the anterior and lateral views (right and left), with the volunteer in orthostatism, and each volunteer was asked to perform a shoulder flexion maneuver at 90° during the photo-shooting session. The same camera was used for all photos and was positioned with the aid of a tripod, which held the camera 76 cm from the floor, 44 cm away from the volunteers, and 80 cm distant from the wall.
Next, volunteers were submitted to ultrasound examination, which was performed by a specialist physician. Ultrasound was used to examine the infra-umbilical region, in a delimited area of 10cm2, with the volunteer in the dorsal decubitus position. This method facilitated the evaluation of the infra-umbilical fat layer thickness in centimeters before the beginning of any procedures and after the proposed treatment.
After progressing through the established study protocol, the volunteers answered patient satisfaction analysis questionnaires, preconized by Segot-chicq et al,9 and the Global Aesthetic Improvement Scale from Narins,10 which is used to classify the response to treatments, enabling a comparative evaluation of results taken at different moments after the intervention.
Treatment protocol. Procedures were performed with the BHS 156 Full device (Body Health, Brazil) during four sessions of once-weekly applications. During the treatment period, all volunteers were placed in the supine position and the applicator was positioned in the infra-umbilical region, which was divided into two quadrants of 10 cm2 for treatment.
Group G01 underwent cryofrequency treatment, which acts through radiofrequency emission, while the poles are at temperatures of less than 0°, with effects on different tissue levels. The following parameters applied: frequency mix and corporal multipolar + monopolar mode, with a temperature of -10°C; 85% power; and 16-minute applications, totaling 32 minutes per session.
Group G02 underwent cryofrequency associated with ultracavitation. The effects during this procedure are the result of unstable cavitation leading to the implosion of adipose cells. The following parameters were applied: frequency of 60 Hz, 70% power, shooting at 25%, duty cycle of 60% on and 40% off, and nine-minute applications per treatment area. The same parameters of G01 were maintained here, totaling 50 minutes per session.
In the CG group, the BHS 156 Full device was used only with the cryotherapy function, with no engagement of the radiofrequency mode. The following parameters were applied: frequency mix and corporal multipolar + monopolar mode, with a temperature of -10°C and 16-minute applications per treatment area, totaling 32 minutes per session.
The reassessment was performed at the end of all sessions with repetition of all the protocols performed before treatment and the application of the proposed questionnaires.
Statistical analysis. The statistical data were analyzed using the Statistical Package for the Social Sciences software version 22.0 for Windows (IBM Corp., Armonk, New York). Two-way analysis of variance was performed with the post-hoc Tukey test. The assigned a level of significance was 95%, with p<0.05.
Results
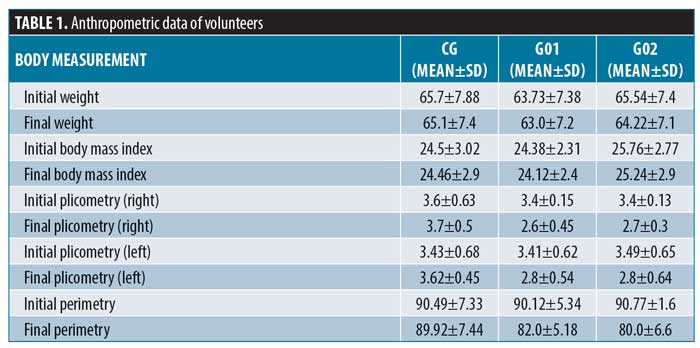
Statistically, no differences were found concerning weight or BMI (p>0.05). The plicometry analysis (right) data showed a statistically significant difference between the G01 and CG groups (p=0.02) and between the G02 and CG groups (p=0.03). In the plicometry analysis (left), statistically significant differences were also found between the G01 and CG groups (p=0.04) and between the G02 and CG groups (p=0.04). As for the perimetry data, a statistically significant difference was observed in the comparison between the G01, G02, and CG groups (p=0.01).
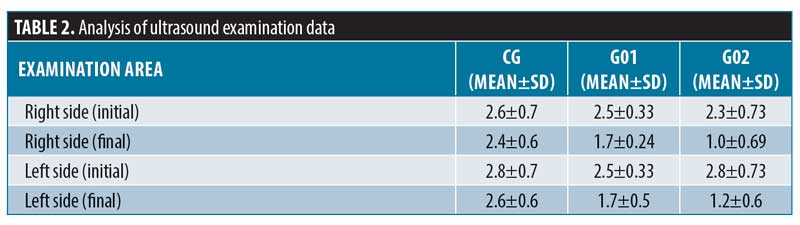
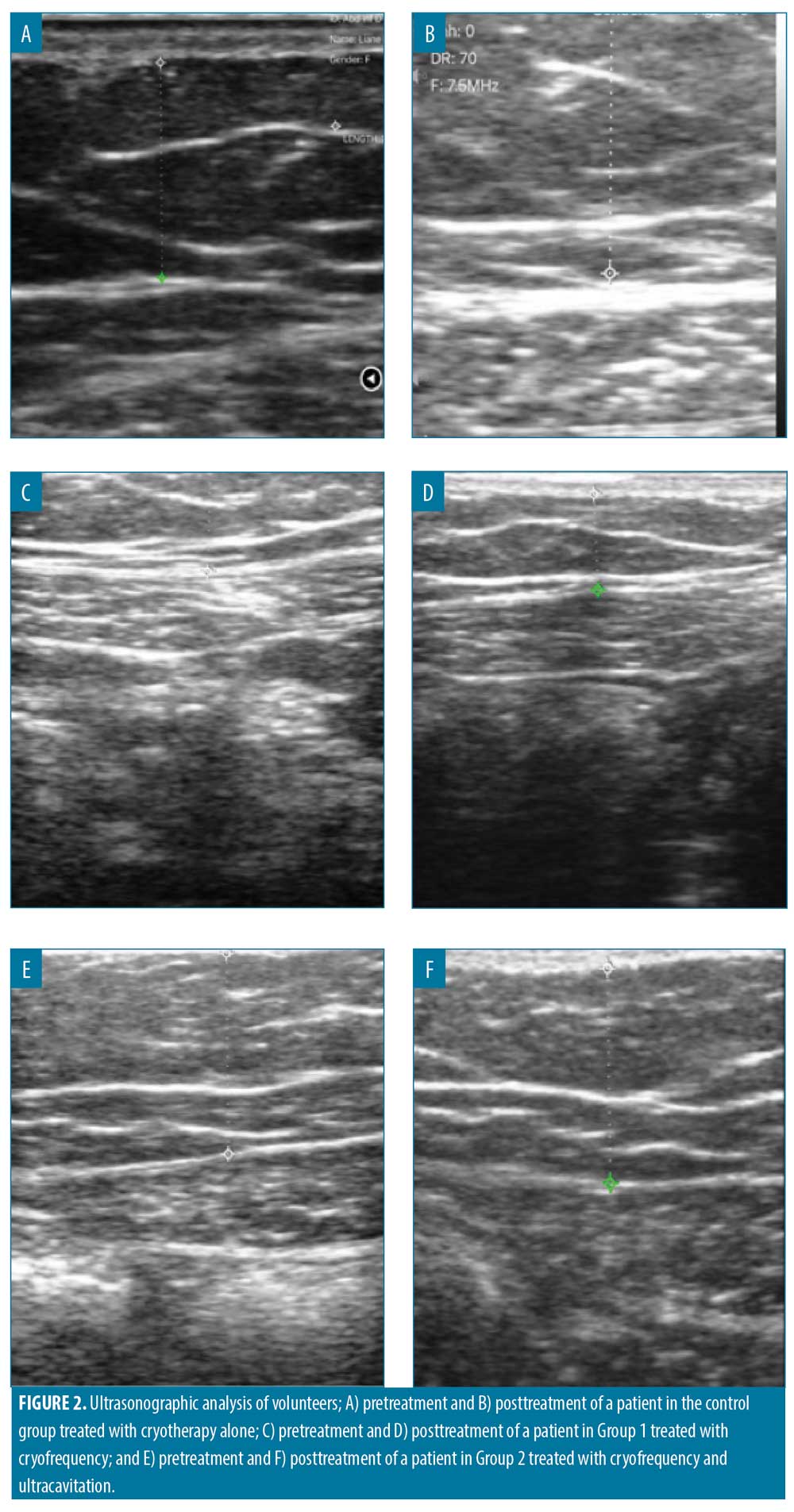
The fat layer thickness was evaluated by pre- and posttreatment ultrasonography. On the right side, a statistically significant difference was found when comparing the G01 and CG groups (p=0.01); also, a statistically significant difference was observed between the G01 and G02 (p=0.001). As for the left side, a statistically significant difference in G01 was found in comparison with in CG (p=0.01), together with a statistically significant difference between G01 and G02 (p=0.001).
Analysis of photographic images of volunteers (Figure 1). Comparing the pre- and posttreatment photographic images, it is possible to observe alterations in the treated groups. The same is apparent when conducting ultrasonographic analysis (Figure 2).
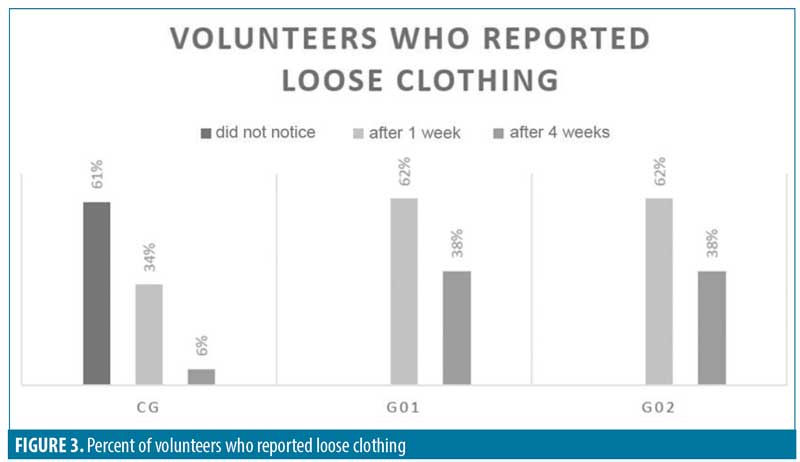
In the analysis of the applied questionnaires, concerning the statement “volunteers who reported loose clothing,” 61 percent of the volunteers from the CG group did not notice this change, 33.5 percent noticed it after one week, and 5.5 percent noticed it after four weeks. G01 and G02 showed the same results: 62 percent noticed it after one week and 38 percent noticed it after four weeks.
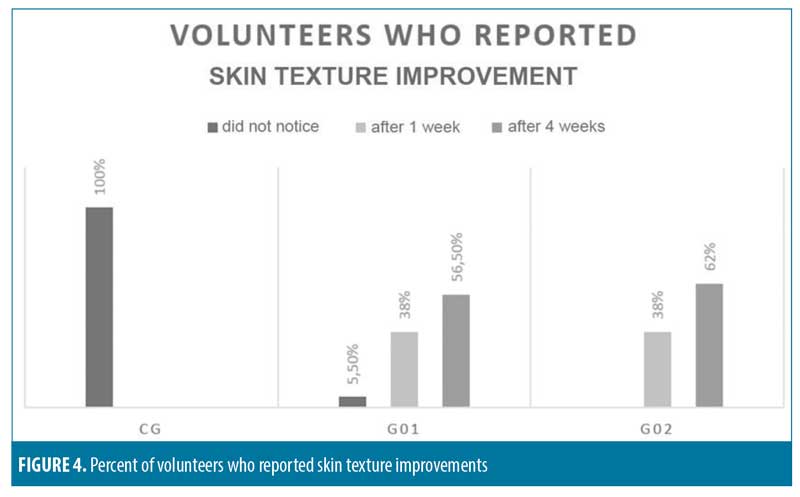
Concerning the statement “volunteers who reported a skin texture improvement,“ 100 percent of the volunteers in the CG group did not notice any such change. Meanwhile, within G01, 5.5 percent did not notice this change, 38 percent noticed this change after one week, and 56.5 percent noticed this change after four weeks. Within G02, 38 percent noticed this change after one week and 62 percent noticed this change after four weeks.
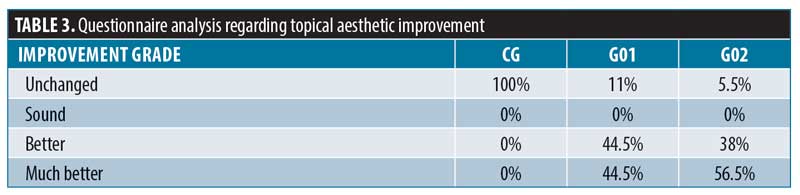
Regarding aesthetic improvements, the results were distributed across four categories: unchanged, sound, better, and much better. It was observed that 100 percent of the CG volunteers reported “unchanged” results, whereas in G01, 44.5 percent reported “better” and 44.5 percent reported “much better” results and only 11 percent reported “unchanged” results”. Within G02, 38 percent stated they noticed “better” results, while 56.5 percent reported “much better,” and 5.5 percent presented “unchanged” results, respectively.
The analysis of the treatment evaluation questionnaire results indicated that 89 percent of the volunteers from G01 reported the therapy they received was a “good treatment,” whereas 11 percent stated it was a “weak treatment.” Within G02, 56.5 percent reported their therapy was an “excellent treatment,” 38 percent said it was a “very good treatment,” and 5.5 percent stated it was a “weak treatment.”
Discussion
Reductions in plicometry, perimetry, and ultrasound measurements were observed within the treated groups when compared to the control group after four treatment sessions. It is believed that cryofrequency acts by inducing adipose tissue degeneration through two pathways: the activation of apoptosis and of inflammatory cells, especially macrophages that phagocyte the apoptotic tissue.4
Cold-stressing can recruit specific proteins, known as heat shock proteins (HSP), which contribute to the protection and repair of damage and consequent apoptosis of adipose tissue cells. Following such thermal changes, the release of HSP60 occurs in adipocytes, which, in addition to interacting, facilitates the action of antigen-presenting cells, leading to the production of proinflammatory cytokines. Among its main biological activities, the modulation of innate and acquired immune responses also occurs, resulting in the infiltration of macrophages in the adipose tissue through the release of chemokines such as monocyte chemoattractant protein-1, which regulates the migration of phagocytic cells. With this, it is possible to justify the significant reduction of the measuring results and the decrease in the fat layer observed via ultrasonographic evaluation.4,11,12
This research confirms the data found by Silva,7 in which six sessions of cryofrequency were performed in the abdominal region of 15 volunteers. At the end of treatment, the results suggested a reduction in the fat layer had occurred based on circumference measurements and ultrasound images, with no relevant serum changes. Such data demonstrate that the application of cryofrequency was able to reduce the aforementioned measures, provide an increase in the firmness, and diminish the wavy aspect of the skin, confirming its effectiveness among existing noninvasive treatments.
In this study, it was verified that the body weight and the BMI of all volunteers did not show modifications after the treatment, suggesting that the noted fat-layer thickness reduction was due to the local treatment. This brings veracity to the measurement reduction results and corroborates with the fact that this study aimed to identify changes in localized adiposity and not in total body mass. These results reinforce the outcomes of the study by Silva et al.6 in which 30 patients with localized fat in the flank region were submitted to eight cryofrequency sessions with no significant changes in body mass or BMI throughout the investigation. However, reductions in the circumference of the treated area and a 0.19-cm reduction of the fat layer were verified after treatment.
When comparing the group treated with cryofrequency alone with that treated with the combination of cryofrequency and ultracavitation, the second group showed superior results, proving that the combination of these technologies is positive. No research concerning the association of these therapies was found, but the action of ultracavitation has been reported before in the literature. The technology acts through the creation of nano-bowels, which, due to their growth and accumulation of energy, become unstable and implode, leading to the lysis of adipocytes. However, the mechanical effect prevents adjacent tissues, including blood vessels, nerves, muscles, and connective tissues, from damage.13,14 For these reasons, this study showed that the association of cryofrequency with ultracavitation is effective in reducing localized adiposity.
Regarding satisfaction with the treatment outcome, most volunteers reported their results were positive and mostly rated their treatment as “excellent,” “very good,” or “good.” The group that received the cryofrequency associated with ultracavitation was the one in which the most number of volunteers rated their treatment as “excellent.” In addition, the treated groups reported a higher perception of changes in the selected measures by noticing loose clothing, increased skin firmness, and aesthetic improvements. For this reason, cryofrequency can be considered an effective treatment with good patient acceptance, which corroborates with previously mentioned research.6
Nevertheless, when analyzing the data presented by the control group, it is possible to notice that, in addition to not experiencing a significant reduction in the analyzed variables, the participants in this group were not influenced by the placebo effect, as most of them did not obtain positive results in the evaluation questionnaires, with only a small portion of the group reporting loose clothing after a few weeks of treatment. However, some studies, despite not identifying significant variable values, report an influence of the placebo effect in the control group’s outcome, both due to the expectations concerning the treatment and the care and attention given to the participants, which led to a positive effect on the questionnaire responses.15–17
Conclusion
Cryofrequency triggered favorable results in terms of less localized adiposity, increased skin tonification, and layer reduction. All results were analyzed using perimetry, plicometry and ultrasonography, generating a positive impact on the satisfaction of all volunteers who received the treatment. Also, the treatment stands out with respect to its high efficiency, which was achieved through its association with ultracavitation. Additional studies are suggested to clarify and explain mechanisms of action of this association, with parameter variations, different models of equipment, and new treatment associations.
References
- Gomes RK, Damazio MG. Cosmetologia: descomplicando os princípios ativos. 3rd ed. São Paulo, Brazil: Livraria Médica Paulista; 2009.
- Fonseca-Alaniz MH, Takada J, Alonso-Vale MI, Lima FB. Adipose tissue as an endocrine organ: from theory to practice. J Pediatr. 2007;83(5 Supl): S192–S203.
- Tagliolatto S, Toschi A, Benemond TM, et al. Criolipolise-revisão da literatura, relato e análise de complicações. Surgical & Cosmetic Dermatology. 2017;9(4):324–327.
- Inácio RF. Análise comportamental do tecido adiposo frente ao tratamento de radiofrequência e criofrequência: revisão bibliográfica. Revista Saúde em Foco. 2017;9(1):248–256.
- Tagliolatto S. Radiofrequência: método não invasivo para tratamento da flacidez cutânea e contorno corporal. Surgical & Cosmetic Dermatology. 2015;7(4).
- Silva RM, Silva MW, Medeiros SF, et al. Effects Of cryofrequency on localized adiposity in flanks. Manual Therapy, Posturology & Rehabilitation Journal. 2019;16.
- Silva MC. Avaliação do uso da criofrequência como terapêutica para a redução da adiposidade abdominal. Lecture presented at: Faculdade de Ciências da Educação e Saúde, Centro Universitário de Brasília; 2016; Asa Norte, Brazil.
- Meyer PF, Mendonça AG, Rodrigues RD, et al. Protocolo de avaliação fisioterapêutica em adiposidade localizada. Fisioter Bras. 2008:26–31.
- Segot-Chicq E, Compan-Zaouati D, Wolkenstein P, et al. Development and validation of a questionnaire to evaluate how a cosmetic product for oily skin is able to improve well-being in women. J Eur Acad Dermatol Venereol. 2007;21(9):1181–1186.
- Narins RS, Baumann L, Brandt FS, et al. A randomized study of the efficacy and safety of injectable poly-L-lactic acid versus human-based collagen implant in the treatment of nasolabial fold wrinkles. Dermatol Surg. 2010;62(3):448–462.
- Carvalho GF, Silva RM, Mesquita Filho JJ, et al. Avaliação dos efeitos da radiofrequência no tecido conjuntivo. Revista Brasileira de Medicina. 2011;68:10–25.
- Marengo EB, Sant’Anna OA. Hsp60 e imunidades: como diante de um espelho partido. ConScientiae Saúde. 2009;8(3):451–458.
- Meyer PF, Carvalho MG, Andrade LL, et al. Efeitos da ultracavitação no tecido adiposo de coelhos. Physical Therapy Brazil. 2012,13(2):106–111.
- Coleman KM, Coleman III WP, Benchetrit A. Non-invasive, external ultrasonic lipolysis. Semin Cut Med Surg. 2009;28(4):263–267.
- Teixeira MZ. Bases psiconeurofisiológicas do fenômeno placebo-nocebo: evidências científicas que valorizam a humanização da relação médicopaciente. Rev Assoc Med Bras. 2009;55(1):13–18.
- Palmieri A, Imbimbo C, Longo N, et al. A first prospective, randomized, double-blind, placebocontrolled clinical trial evaluating extracorporeal shock wave therapy for the treatment of Peyronie’s disease. Eur Urol. 2009;56(2):363–370.
- Mlosek RK, Wozniak W, Malinowska S, et al. The effectiveness of anticellulite treatment using tripolar radiofrequency monitored by classic and high-frequency ultrasound. J Eur Acad Dermatol Venereol. 2012;26(6):696–703

