 J Clin Aesthet Dermatol. 2021;14(8):41–43.
J Clin Aesthet Dermatol. 2021;14(8):41–43.
by David Cassarino, MD, PhD and My Diep, BS
Dr. Cassarino is with the Department of Pathology at Kaiser SCPMG in Los Angeles, California. Mr. Diep is with the College of Osteopathic Medicine of the Pacific, Western University of Health Sciences in Pomona, California.
FUNDING: No funding was provided for this article.
DISCLOSURES: The authors report no conflicts of interest relevant to the content of this article.
ABSTRACT: Angiolipomas are benign vascularized variants of lipomas. They can present as a solitary lesion or in clusters, occurring equally in both male and female patients, often after puberty. Angiolipomas are uncommon and few cases have been documented, especially cases with very high counts or multiple clusters. The clinical presentation is similar to that of lipomas; however, they have distinct histological characteristics with varying levels of vascularity and microthrombi intimately associated with mature adipocytes. Angiolipomas can be further classified as non-infiltrating or infiltrating depending on their encapsulation and relation to other structures. Although the etiology is unknown, angiolipomas have been shown to be associated with systemic disease, such as diabetes mellitus and HIV, and a link to HIV protease inhibitors has also been documented in several case reports. However, no cases have been reported in patients with liver disease before. Herein, we present a rare and unusual case of a male patient with a history of hepatitis B and hepatocellular carcinoma and at least 68 angiolipomas.
Keywords: Angiolipoma, lipoma, hepatitis B, hepatocellular carcinoma
Angiolipomas are benign vascularized subcutaneous nodules.1 They can appear solitarily or in clusters, occurring equally in both male and female patients, and often after puberty.1–3 Their clinical presentation is similar to that of lipomas; however, they have distinct histological characteristics, with varying levels of vascularity and microthrombi that infiltrate mature adipocytes.4–7 Additionally, angiolipomas can be further classified as noninfiltrating or infiltrating depending on their encapsulation and relation to other structures.5–7 Although the etiology is unknown, angiolipomas have been shown to be associated with systemic disease, such as diabetes mellitus and human immunodeficiency virus (HIV).8–11 A link to HIV protease inhibitors has also be documented in several case reports. Angiolipomas are uncommon, and few cases have been documented, especially cases with high counts or multiple clusters.12 Here, we present a very rare case of a male patient with a history of hepatitis B and hepatocellular carcinoma and at least 68 angiolipomas.
Case Presentation
A 65 year-old male patient presented to the clinic with a series of angiolipomas with a history of at least 68 masses bilateral on the upper extremities, most of which were removed. The patient had a medical history of hepatitis B and hepatocellular carcinoma. Additionally, the patient had undergone laparoscopic hepatectomy and cholecystectomy. Upon physical examination, the patient appeared alert and well, with no apparent distress. Skin examination showed bilateral multiple angiolipomas that were visible and palpable on the upper extremities. The patient identified three separate clusters of two and three angiolipomas, which were mobile and nontender, on the left forearm that were most bothersome and which he wanted removed.
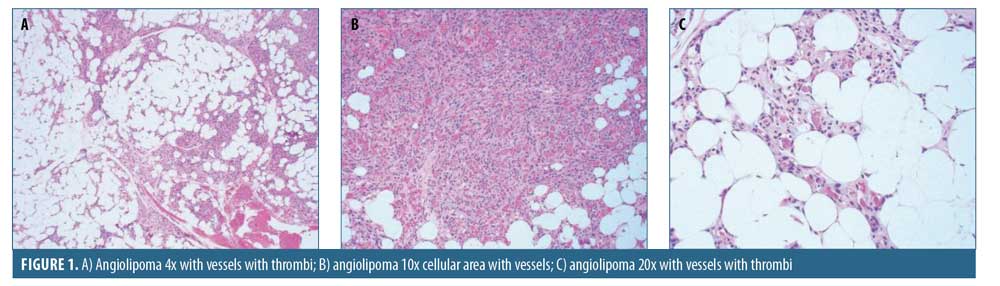
Numerous biopsies were performed over several years, all of which showed typical features, including a proliferation of mature adipocytes intimately associated with numerous small capillary type vessels (Figures 1A, 1B, and 1C), many of which had intraluminal thrombi. Some of the tumors showed more cellular areas composed of numerous small, closely packed blood vessels (Figure 1B).
Discussion
Angiolipomas are subcutaneous nodules that, on clinical presentation, are almost identical to an ordinary lipoma. The similarity in clinical appearance often leads to the preoperative diagnosis of lipoma in patients if not excised and examined.1 Thus, histopathological evaluation is necessary for the diagnosis of angiolipomas.2 The histological features of angiolipomas consist of mature adipocytes that are transversed by prominent vasculature. The degree of vascularity can vary from less than one percent to 90 percent, where the proportion of vascularity is not correlated with size of the angiolipoma.1,3 In examining the ultrastructure of angiolipomas, Dixon et al1 noted that the branching pattern of vasculature was more complex with higher pericyte proliferation relative to capillaries that were found in lipomas. This further differentiates angiolipomas from lipomas beyond just the presence of extensive vascularity. Additionally, within the vasculature are miniature thrombi that are mostly located on the periphery. However, the thrombi do not normally cause necrosis due to collateral supply.4 The microthrombi are theorized to arise from damage caused by the chronic growth of the angiolipoma.4
Additionally, angiolipomas can be further categorized as noninfiltrating or infiltrating angiolipomas.4–6 Noninfiltrating angiolipomas are more common and can exist either as a single mass or in multiples, while noninfiltrating angiolipomas have well-defined borders, encapsulated by collagen fibers.5 On the other hand, infiltrating angiolipomas have poorly demarcated borders and can encroach on nearby structures, such as nerves and skeletal tissue. Among the subtypes of angiolipomas, infiltrating angiolipomas occur more rarely and can elicit additional symptoms, such as nerve suppression.6 Furthermore, in both instances, noninfiltrating or infiltrating angiolipoma can cause pain or tenderness, which are not commonly seen in lipomas.4 Pain has also been shown to be correlated with the degree of vascularity and the relative size of the angiolipoma, with larger tumors being more painful.1,3
The cause of angiolipomas has not been fully elucidated; however, several explanations have been offered in the current literature. One of the speculations is that angiolipomas originate from congenital migration of multipotent cells that are later activated by hormones during puberty.3–6 This corresponds with the occurrence of angiolipoma only in patients after puberty. It is also believed that the vasculature in angiolipomas arise from repeated trauma to the area.7 Furthermore, angiolipomas are linked to other conditions, such as diabetes mellitus, and antiretroviral medication usage, which can provide some insight into their etiology.8–11
Protease inhibitors, antiretroviral medications used in patients with HIV, have been noted to be associated with the onset of angiolipomas. The protease inhibitors that were documented were indinavir and saquinavir.8,11 Their known side effects include lipodystrophy, hyperlipidemia, and insulin resistance. Lipodystrophy has clinical manifestations of increased anterior cervical and dorsocervical fat as well as increased breast fat and centripetal obesity.10 The fat redistribution that causes these gross bodily changes can also be a process that triggers the growth of angiolipomas. Though there is no direct evidence of their causation of angiolipomas, the timing of the introduction of medications and the appearance of these lesions in multiple cases found in the current literature are suggestive of their association.8,10,11 Further support for their link can also be seen in cases where angiolipomas regressed once protease inhibitor therapy was stopped. In their case report, Dank et al11 alluded to a hypothesized mechanism on how protease inhibitors lead to lipodystrophy. The suggested process involves cytochrome P-450 3A in peripheral adipocytes; the inhibition of this cytochrome leads to the dysfunctional production of cis-9-retinoic acid, which can cause impaired fat storage and lipid release in adipocytes. As a result, there is a greater accumulation of fat in central adipocytes.11 With a possible link between angiolipomas and lipodystrophy, this mechanism should be investigated as a possible pathophysiology of angiolipomas in different settings.
However, the mechanism incorporating protease inhibitors only describes the increase in adipose tissue, and the angiogenic properties of angiolipomas have been speculated to be an effect of HIV. This was suggested by Blanes et al,10 who proposed that the HIV transactivator of transcription (Tat) might be involved in the pathogenesis of angiolipomas in HIV infection. HIV Tat, a nuclear transactivator of the viral gene, is released by infected cells and has been shown to have angiogenic properties.10 This is proposed as a possible cause or trigger in the development of angiolipomas in HIV patients. Another case report documents the appearance of multiple angiolipomas in a patient with HIV prior to any initiation of antiretroviral drugs.12 This patient showcases a potential link between HIV infection and angiolipomas. Thus, further investigation of the angiogenic properties of HIV Tat might be useful in identifying the disease process of both HIV and angiolipomas.
In addition to HIV medications, diabetes has also been recorded to have an association with angiolipomas. One case report documented a male patient who presented with six angiolipomas two months after a diagnosis of diabetes mellitus.9 Once blood glucose was properly managed in this patient, the angiolipomas decreased in size and two resolved completely. This unique presentation and other cases can offer further insight into the possible factors that contribute to the development of angiolipomas. The onset of angiolipomas in various disease states, especially in cases of metabolic dysfunction, might be suggestive of the mechanisms involved in angiolipomas. In addition, angiolipomas can possibly be utilized as an indicator of metabolic impairments in patients presenting with these lesions who are unaware of any other systemic abnormalities.
Our patient presented with a remarkable history of chronic hepatitis B infection, hepatocellular carcinoma, several surgical procedures, and the use of several medications. Currently, there is no recorded link between angiolipomas and hepatitis B infection or hepatocellular carcinoma. Hepatitis B is often associated with extrahepatic cutaneous manifestations. In a study by Rostey and Souto,13 88.9 percent of 108 patients diagnosed with hepatitis B or C displayed cutaneous findings. However, whether the skin findings were a direct result of viral hepatitis was not proven in their study.13 Cutaneous symptoms include urticaria, angioedema, polyarteritis nodosa (PAN), and cryoglobulinemic vasculitis,14,15 and most cutaneous associations arise from immune responses due to the hepatitis B virus. Of the cutaneous manifestations, PAN development provides the most relevance and insight to elucidating the occurrence of angiolipomas in our patient. During the disease process, PAN can form subcutaneous nodules alongside arteries.16 Angiolipomas, being subcutaneous nodules, can possibly be triggered by hepatitis B infection, similar to the case of the development of PAN. However, there is no evidence that supports this notion, and further survey of the patient population will be necessary to elucidate this association.
Additionally, liver diseases, including hepatocellular carcinoma, have also been shown to affect the endocrine system.17 The offset in hormones during disease pathogenesis could potentially trigger angiolipoma emergence. This is based on the theory of hormonal involvement in the development of angiolipomas that was mentioned earlier.1,4,7 Again, further investigation is warranted in identifying whether there is a relationship between liver diseases and the cutaneous manifestations of angiolipomas.
As for treatment, angiolipomas are benign tumors, and so are often removed for discomfort and cosmetic reasons. Angiolipomas can typically be fully excised to prevent recurrence.4 However, the extent of excision is also dependent on the degree of infiltration. When angiolipomas have infiltrated nearby soft tissue structures, such as nerves and major vessels, full excision might not be possible in order to conserve critical structures.18 In such a case, radiotherapy can be used in conjunction to address the remnants of the angiolipoma.18 Another treatment option is liposuction,19 where cannulas of varying sizes can be used to extract the angiolipoma. This procedure can be advantageous in cases with multiple angiolipomas. Liposuction minimizes scarring compared to direct excision of the mass. This is because one incision site can be utilized as an access point to target multiple angiolipomas in the surrounding area. Additionally, further scarring can be minimized through careful placement of the incision, and liposuction allows for such flexibility.19 Although there are several options for angiolipoma removal, like in the case of our patient, recurrences can still occur, and there is no treatment to fully prevent their growth.
Conclusion
Our patient had multiple clusters of angiolipomas on his upper extremities, which, although nontender, were uncomfortable. His numerous lesions, along with his extensive medical history of hepatitis B and hepatocellular carcinoma, is very rare and has not been previously documented. The etiology of angiolipomas remains unclear, and so it becomes challenging to assess their link to the patient’s history. However, hepatitis B and hepatocellular carcinoma have both been shown to be associated with extrahepatic cutaneous manifestations as a result of immune responses and changes in the endocrine system. Additionally, the current literature also documents angiolipomas in relation to diabetes mellitus, HIV infection, and antiretroviral medications. Their association can be another valuable avenue to understand the mechanism and factors behind the emergence of these lesions. Further investigation of the association between angiolipomas and liver disease, as well as other systemic conditions, may provide new understanding of the pathogenesis of these conditions.
References
- Dixon AY, McGregon DH, Lee SH. Angiolipomas: An ultrastructural and clinicopathological study. Hum Pathol. 1981;12(8)739–747.
- Kumar PS, Kamath SM, Shyam Prasad AL, et al. Acute-onset of multiple painful nodules over forearms and back. J Clin Diagn Res. 2013;7(10):2314–2316.
- Belcher RW. Multiple (subcutaneous) angiolipomas. Clinical, pathologic, and pharmacologic studies. Arch Dermatol. 1974;110(4)583–585.
- Lin JJ, Lin F. Two entities in angiolipoma(A study of 459 cases of lipoma with review of literature on infiltrating angiolipoma). Cancer. 1974;34(3):720–727.
- Puig L, Moreno A, De Moragas JM. Infiltrating angiolipoma: report of two cases and review of the literature. J Dermatol Surg Oncol. 1986;12(6)617–619.
- Dionne GP, Seemayer TA. Infiltrating lipomas and angiolipomas revisited. Cancer. 1974:33(3):732–738.
- Howard WR, Helwig EB. Angiolipoma. Arch Dermatol. 1960;82(6):924–931.
- Daudén E, Alvarez S, and García-Díez A. Eruptive angiolipomas associated with antiretroviral therapy. AIDS Lond Engl. 2002;16(5):805–806.
- Levitt J, Ali SAL, Sapadin A. Multiple subcutaneous angiolipoma associated with new-onset diabetes mellitus. Int J Dermatol. 2002;41(11):783–785.
- Blanes M, Boix V, Belinchón I, Portilla J. Angiolipomas, a rare manifestation of HIV-associated lipodystrophy. AIDS Lond Engl. 2008;22(4):552–554.
- Dank JP. Colven R. Protease inhibitor–associated angiolipomatosis. J Am Acad Dermatol. 2000;42(1 Pt 1):129–131.
- Motswaledi HM. Multiple nodules on the trunk and arms. Int J Dermatol. 2010;49(12): 1349–1350.
- Rostey RRL, Souto FJD. Observational descriptive study of cutaneous manifestations in patients from Mato Grosso with viral chronic hepatitis. An Bras Dermatol. 2015;90(6):828–835.
- Dogra S, Jindal R. Cutaneous manifestations of common liver diseases. J Clin Exp Hepatol. 2011;1(3):177–184.
- Pyrsopoulos NT, Reddy KR. Extrahepatic manifestations of chronic viral hepatitis. Curr Gastroenterol Rep. 2001;3(1):71–78.
- McElgunn SJ. Dermatologic manifestations of hepatitis B virus infection. J Am Acad Dermatol. 1983;8(4):539–548.
- Burra P. Liver abnormalities and endocrine diseases. Best Pract Res Clin Gastroenterol. 2013;27(4):553–563.
- Yeo ED, Chung BM, Kim EJ, Kim WT. Infiltrating angiolipoma of the foot: magnetic resonance imaging features and review of the literature. Skeletal Radiol. 2018;47(6):859–864.
- Kaneko T, Tokushige H, Kimura n, et al. The treatment of multiple angiolipomas by liposuction surgery. J Dermatol Surg Oncol. 1994;20(10): 690–692.

