 J Clin Aesthet Dermatol. 2023;16(3):32–36.
J Clin Aesthet Dermatol. 2023;16(3):32–36.
by Khaled Gharib, MD; Alshimaa Ibrahim, MD; Yasmeen El Sharkawi, MBBCH; Nagia Elmegrab, MD; and Mohamed Attia, MD
All authors are with the Dermatology, Venereology and Andrology Department, Faculty of Medicine at Zagazig University in Zagazig, Egypt.
FUNDING: No funding was provided for this article
DISCLOSURES: The authors report no conflicts on interest relevant to the content of this article.
ABSTRACT: Background. Methotrexate has been used successfully in the treatment of vitiligo. It leads to decrease in the number of TNF-α secreting T cells in association with increase in the number of interleukin (IL)-10 producing T cells. Topical forms of methotrexate do not have significant hematologic or hepatotoxic side effects unlike the systemic forms of the drug.
Objective. We sought to evaluate the efficacy and safety of methotrexate gel for the treatment of vitiligo, either alone or combined with narrowband (NB) ultraviolet B (UVB) or with excimer light.
Methods. Forty-eight patients with vitiligo were randomized into three treatment groups. Group I was treated with methotrexate gel twice daily. Group II was treated with methotrexate gel twice daily plus NB-UVB twice weekly. Group III was treated with methotrexate gel twice daily combined with excimer light twice weekly. Treatment was continued for three months followed by a one-month follow-up period.
Results. there was a statistically significant difference between groups regarding the therapeutic response. The highest response was recorded in the group treated with methotrexate gel and NB-UVB. More patients in Group II showed good or excellent response than in the other groups.
Conclusion. Methotrexate gel could increase the therapeutic effect of NB-UVB and excimer laser and shorten the treatment period of vitiligo. However, it was not effective enough to induce repigmentation when used alone.
Keywords: Methotrexate, vitiligo, laser
Vitiligo is the most prevalent depigmenting skin disorder that causes the selective destruction of melanocytes, resulting in depigmentation of the skin, hair, and mucosa. It appears to be equally prevalent in men and women, and there are no differences in the rate of occurrence according to skin type or race.1
The basic goals of vitiligo treatment are stopping the progression of the disease, repigmentation via promoting melanocyte differentiation and proliferation, and avoiding relapses. One of the safest and most successful treatments for vitiligo is narrowband (NB) ultraviolet B (UVB) therapy. Excimer laser (EL), a targeted phototherapy device, inhibits inflammation and induces T-cell apoptosis by emitting coherent and monochromatic light at 308 nm, which is close to 311 nm NB-UVB. Additionally, it stimulates melanocyte stem cells to differentiate, which is associated with increased migration of melanocytes to induce repigmentation with no effect on nearby skin.2,3
Methotrexate (MTX) is a folic acid antagonist, antiproliferative and immunomodulating drug that leads to decrease in the number of TNF-α-producing T cells, whereas the number of IL-10 producing T cells increases. Additionally, it suppresses B cells and controls the generation of interleukin (IL)-6 and reactive oxygen species. All of these factors help in the treatment of vitiligo. Unlike oral MXT, it has been suggested that topical preparations of the drug have no significant related hepatotoxic and hematologic adverse effects.4–7
The aim of this study was to evaluate the efficacy and safety of MTX topical gel, either alone or combined with NB-UVB or excimer light, for the treatment of vitiligo.
Methods
Patients. This study included 48 patients of both sexes with localized, non-segmental vitiligo. Their ages ranged from 6 to 62 years. They were recruited from the Dermatology Department of Zagazig University Hospital. Approval was obtained from the Zagazig University Institutional Review Board (IRB #5947/5-3-2020). Patients on other treatment modalities for vitiligo, patients with photosensitivity, patients with renal or hematological disorders, patients with hepatic disease, pregnant and lactating patients were excluded. Included patients were randomly divided according to computer generated random list into three groups. Group I wass treated only by topical methotrexate gel 1% twice daily. Patients were instructed to apply one finger tip unit of methotrexate gel twice daily to the treated areas. Group II was treated with topical methorexate gel 1% twice daily combined with NB-UVB (Philips TL100, Hamburg, Germany) twice weekly with a starting dose of 200 mJ/cm2 irrespective of skin type. Increment in dose was 10% to 20% per session. The dose was adjusted according to NB-UVB treatment guidelines.2 Group III was treated with topical methotrexate gel 1% twice daily combined with excimer lamp (Peninsula Excimer system; Peninsula Company, China) with starting a dose of 100 to 150mJ/cm2 for the head and neck and from 200 to 600 mJ/cm2 for other sites. The dose was increased by 50 mJ/cm2 per session, according to the protocol described by Beggs et al.8 The duration of treatment was three months, followed by one-month follow-up period.
Methotrexate gel preparation. MTX gel was prepared in the Department of Pharmaceutics at Zagazig University. Sodium benzoate and methotrexate were initially dispersed in distilled water containing 15% w/w glycerin. Then the gel base (Na CMC) was added to the solution and mixed using a mechanical stirrer at 10,000 rpm until homogeneity was attained.
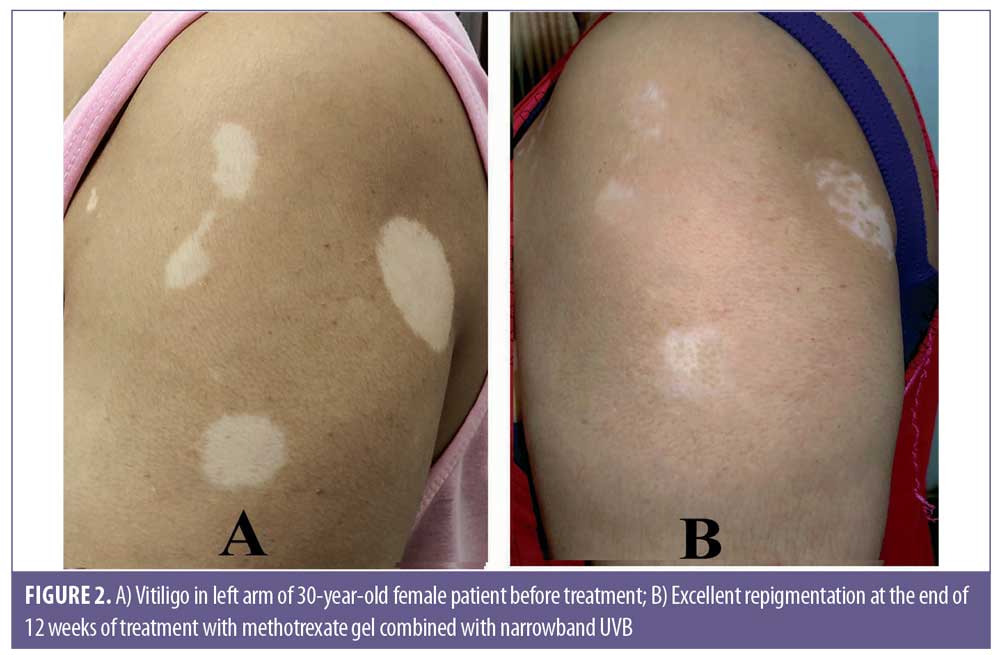
Assessment of improvement. Patients were photographed before and after treatment. The improvement was classified according to the percentage of repigmentation at the end of treatment: G0=No response (0%); G1=poor (<25%); G2=moderate (25 to <50%), G3=good (≥50–75%), and G4=excellent if repigmentation 75% or greater.9
Statistical analysis. All data were collected, tabulated, and statistically analyzed using IBM Corp. Released 2015. IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp. Quantitative data were expressed as the mean ± SD &median (range), and qualitative data were expressed as & (percentage). Kruskall Wallis test was used to compare between more than two groups of non-normally distributed variables. Percent of categorical variables were compared using Chi-square test. All tests were two sided. p<0.05 was considered statistically significant, p<0.001 was considered statistically highly significant.
Results
Demographic and clinical data of the studied patients. Forty-eight patients (26 female, 22 male) completed the study. Their ages ranged from 6 to 62 years. The disease duration ranged from six months to seven years. The disease severity was assessed according to VASI score. VASI scores of patients in Group I ranged from 0.11 to 5.48, with a median of 0.45. In Group II, the VASI score ranged from 0.06 to 7.4, with a median of 2.62. In Group III, VASI scores ranged from 0.08 to 2.25 with a median of 0.2. No significant differences in the demographic and baseline characteristics were observed between the studied groups, however the VASI scores of patients in Group II was significantly higher than patients in Groups I and III.
Therapeutic response for treatment modalities among the studied groups. There was a statistically significant difference between groups regarding the therapeutic response (P<0.05). The therapeutic response was better in Group II (methotrexate gel combined with NB-UVB). The mean percentage of repigmentation in Group II was (49.7±33.5) versus (19.3±20.7) in Group I (methotrexate gel alone), and (39.9±33.8) in Group III (combined methotrexate gel with excimer light). Grade 3 (Very Good response) and Grade 4 (Excellent response) were reported more frequently in Group II than the other groups. Grade 0 (No response) was reported in six patients in Group I, three patients in Group II, and four patients in Group III (Table 1, Figures 1–3).1–3


Adverse effects of treatment among the studied groups. Mild itching was reported in three patients in Group I and two patients in Group III. In Group III, peripheral hyperpigmentation of the treated patches was reported in three patients in addition to blistering in four patients. Erythema was reported in four patients in Group II and three patients in Group III.
Relation between patients’ therapeutic response and their demographic and basic clinical characters. There was a significant correlation between patients’ therapeutic response in all groups and the site of lesion. Facial lesions showed the best response, while acral sites showed less response in all groups (P<0.05). On the other hand, there was no significant correlation between patients’ therapeutic response in all groups and other clinical or demographic characters (p>0.05).
Discussion
The etiopathogenesis of vitiligo is complex, and the disease’s symptoms, development, and therapeutic response are variable. Melanocyte loss is thought to be caused by a number of factors, including genetic predisposition, environmental stimuli, metabolic disturbances, and altered inflammatory and immunological responses.10,11
Vitiligo has been treated with a variety of topical medications, including corticosteroids, calcineurin inhibitors, and vitamin-D3 analogues, with varying degrees of success. According to an increasing number of publications, topical medications with NB-UVB phototherapy or excimer light may have synergistic benefits. Phototherapy is acting through immunosuppression and stimulation of melanocyte activity and migration from hair follicles to the epidermis. Since phototherapy causes T-cell apoptosis, decreases in antigen-presenting cells, suppression of inflammatory cytokines, and increases of interleukin 10, it is capable of slowing the disease activity.12,13,14
There are two types of devices that can deliver monochromatic excimer light (MEL, 308 nm)—excimer lamp and the excimer laser. The excimer laser emits monochromatic coherent light that is only directed at the affected skin, while the excimer lamp emits incoherent monochromatic light that can treat a larger affected area. Comparative studies of the excimer laser and light have revealed that the treatments for vitiligo were equally effective with both tools.12
Systemic MTX has been used successfully in the treatment of vitiligo. However, patients presented with localized or mild disease shouldn’t be treated with systemic MTX due to the risk of hematologic and hepatic side effects.Topical MTX avoids these side effects. Topical MTX has been utilized in the treatment of psoriasis, early stage mycosis fungoides, lymphomatoid papulosis, oral precancerous lesions, and localized alopecia areata.15,16
To our knowledge, there are no controlled studies that evaluate the efficacy of topical MTX in the treatment of vitiligo. There is only one case report that recorded significant repigmentation in one patient who presented with localized truncal vitiligo.7
In the present study, we evaluated the efficacy of methotrexate gel either alone or combined with NB-UVB or excimer light in treatment of vitiligo. Our study included 48 patients who were divided into three treatment groups. There was no statistically significant difference between the three studied groups regarding age, sex, disease duration, or site of lesions.
The difference between groups regarding therapeutic response was statistically significant. The highest response was reported in Group II (methotrexate gel combined with NB- UVB). The mean percentage of repigmentation in Group II was 49.7±33.5 versus 19.3±20.7 in Group I (methotrexate gel alone), and 39.9±33.8 in Group III (combined methotrexate gel with excimer light).
In Group I, good response (> 50% repigmentation) was noted only in 6.3% of patients. The therapeutic response to methotrexate gel in the present study was lower than studies that were done with other topical medications, such as mometasone, pimecrolimus, and tacrolimus, with mean repigmentation rates ranging from (42 % to 65% ).5,17
In Group II (treated with methotrexate gel combined with NB UVB); good to excellent response (>50% repigmentation) was noted in 56.3% of cases. This response was much higher than that reported by Verhaeghe et al18 and Poolsuwan et al9 who reported greater than 50% repigmentation in 20% and 30.56% of vitiliginous lesions treated by NB-UVB alone for three months. On the other hand, the result of the present study was similar to the results reported by Yones et al19 that showed greater than 50% repigmentation in 64% of patients treated with NB-UVB alone for six months, which was a longer treatment duration than our study.
In Group III (treated by MTX gel combined with excimer light), >50% repigmentation was noted in 37.5% of patients. This came in agreement with Poolsuwan et al9 who reported >50% repigmentation in 33.33% of lesions treated with excimer laser for six months.
Our results were better than the results of Soliman et al20 who reported that no lesion treated with excimer laser for three months showed excellent response or good response, only (48.9%) of lesions showed moderate response, and 51.1% of lesions showed less than 25% repigmentation.
These findings may indicate that combination of topical methotrexate with NB-UVB or excimer laser can increase the efficacy of treatment and shorten the treatment period.
Methotrexate has anti-inflammatory, immunomodulatory and antiproliferative effect through a decrease in the number of TNF-α-producing T cells, whereas the number of T cells producing IL-10 increase. MTX possibly suppresses TNF-α-induced nuclear factor-κB activation through the release of adenosine. Moreover, it modulates IL-6 synthesis and reactive oxygen species production21,22
Our results were worse than Elsaadany et al23 who reported greater than 50% repigmentation in 72.22% of the excimer treated patches. This difference in results may be due to the greater number of acral lesions that were included in our study (43.8%) than in Elsaadany et al’s study (11.11%) or difference in the used excimer device.
In agreement with our study, Koh et al24 reported higher response rate with NB-UVB than excimer lamp phototherapy in the treatment of Asian children with vitiligo. Several meta-analyses have shown similar efficacy between excimer light and NB-UVB for the treatment of vitiligo. They suggested that the therapeutic impact of the 308-nm excimer light and NB-UVB may be similar because their wavelengths are so near to one another.25,26
Some studies reported that excimer light is more effective than NB-UVB in treatment of vitiligo. They proposed that this may be related to the fact that the two treatment modalities have different modes of action, with excimer light delivering higher energy fluences to the treatment area faster than NB-UVB. As a result, excimer light may induce a greater number of apoptotic cells than NB-UVB at the same dosage.27,28
There was significant correlation between patients’ therapeutic response in all groups and the site of lesion. Better therapeutic response was recorded in facial sites. Acral sites showed poor response in all groups. These findings are in agreement with most of studies as reported by Fai et al,29 Xu et al,30 and Fa et al.31
Concerning side effects, the side effect in all groups were mild and well tolerated in the form of mild itching, symptomatic erythema. In addition to perilesional hyperpigmentation reported in (18.8%) and blister formation in (26.7%) of patients treated by excimer laser combined with methotrexate gel, this result was in agreement with Bae et al.12
Conclusion
Topical methotrexate could increase the therapeutic effect of NB-UVB and excimer laser and shorten the treatment period of vitiligo. However, it was not effective enough to induce repigmentation when used alone.
References
- Latipov II, Axmedovich MF, Hamza o’g’li OJ. Clinical and immunogycal aspects of pathogenesis and complex therapy of vitiligo. Academicia Globe: Inderscience Research. 2021 Nov 17;2(11):14–20.
- Khanna U, Khandpur S. What is new in narrow-band ultraviolet-B therapy for vitiligo? Indian Dermatology Online Journal. 2019 May;10(3):234.
- Rodrigues M, Ezzedine K, Hamzavi I, et al. Vitiligo Working Group. New discoveries in the pathogenesis and classification of vitiligo. Journal of the American Academy of Dermatology. 2017 Jul 1;77(1):1–3.
- Tharp MD. Calcineurin inhibitors. Dermatologic Therapy. 2002 Dec;15(4):325–332.
- AbdElazim NE, Yassa HA, Mahran AM. The efficacy, safety, and stability of tacrolimus 0.03% ointment in treatment of nonsegmental vitiligo. Journal of Current Medical Research and Practice. 2020 Jan 1;5(1):41.
- ElGhareeb MI, Metwalli M, AbdelMoneim N. Combination of oral methotrexate and oral mini-pulse dexamethasone vs either agent alone in vitiligo treatment with follow up by dermoscope. Dermatologic Therapy. 2020 Jul;33(4):e13586.
- Abdelmaksoud A, Dave DD, Lotti T, et al. Topical methotrexate 1% gel for treatment of vitiligo: A case report and review of the literature. Dermatologic Therapy. 2019 Sep;32(5):e13013.
- Beggs S, Short J, Rengifo-Pardo M, et al. Applications of the excimer laser: a review. Dermatologic Surgery. 2015 Nov 1;41(11):1201–1211.
- Poolsuwan P, Churee C, Pattamadilok B. Comparative efficacy between localized 308 nm excimer light and targeted 311 nm narrowband ultraviolet B phototherapy in vitiligo: A randomized, single-blind comparison study. Photodermatology, Photoimmunology & Photomedicine. 2021 Mar;37(2):123–130.
- Picardo M and Taïeb A. (2019): Vitiligo (Springer, Heidelberg and New York, 2019 Jul. pp. 141-150.
- Abdel-Malek ZA, Jordan C, Ho T, et al. The enigma and challenges of vitiligo pathophysiology and treatment. Pigment cell & melanoma research. 2020 Nov;33(6):778–787.
- Bae JM, Hong BY, Lee JH, et al. The efficacy of 308-nm excimer laser/light (EL) and topical agent combination therapy versus EL monotherapy for vitiligo: a systematic review and meta-analysis of randomized controlled trials (RCTs). Journal of the American Academy of Dermatology. 2016 May 1;74(5):907–915.
- Sassi F, Cazzaniga S, Tessari G, et al. Randomized controlled trial comparing the effectiveness of 308 nm excimer laser alone or in combination with topical hydrocortisone 17-butyrate cream in the treatment of vitiligo of the face and neck. British Journal of Dermatology. 2008 Nov;159(5):1186–1191.
- Felsten LM, Alikhan A, Petronic-Rosic V. Vitiligo: A comprehensive overview: Part II: Treatment options and approach to treatment. Journal of the American Academy of Dermatology. 2011 Sep 1;65(3):493–514.
- Aickara D, Bashyam AM, Pichardo RO, et al. Topical methotrexate in dermatology: A review of the literature. Journal of Dermatological Treatment. 2022 Jan 2;33(1):512–527.
- Hamdino M, El-Barbary RA, Darwish HM. Intralesional methotrexate versus triamcinolone acetonide for localized alopecia areata treatment: A randomized clinical trial. Journal of Cosmetic Dermatology. 2022 Feb;21(2):707–715.
- Köse O, Arca E, Kurumlu Z. Mometasone cream versus pimecrolimus cream for the treatment of childhood localized vitiligo. Journal of dermatological treatment. 2010 May 1;21(3):133–139.
- Verhaeghe E, Lodewick EV, van Geel N, et al. Intrapatient comparison of 308-nm monochromatic excimer light and localized narrow-band UVB phototherapy in the treatment of vitiligo: a randomized controlled trial. Dermatology. 2011;223(4):343–348.
- Sung JY, Hong JH, Kang HS, et al. Methotrexate suppresses the interleukin-6 induced generation of reactive oxygen species in the synoviocytes of rheumatoid arthritis. Immunopharmacology. 2000 Apr 1;47(1):35–44.
- Majumdar S, Aggarwal BB. Methotrexate suppresses NF-κB activation through inhibition of IκBα phosphorylation and degradation. The Journal of Immunology. 2001 Sep 1;167(5):2911–2920.
- Yones SS, Palmer RA, Garibaldinos TM, et al. Randomized double-blind trial of treatment of vitiligo: efficacy of psoralen–UV-A therapy vs narrowband–UV-B therapy. Archives of dermatology. 2007 May 1;143(5):578–584.
- Soliman M, Samy NA, Abo Eittah M, et al. Comparative study between excimer light and topical antioxidant versus excimer light alone for treatment of vitiligo. Journal of Cosmetic and Laser Therapy. 2016 Jan 2;18(1):7–11.
- Elsaadany AE, El-Khalawany M, Elshahid AR, et al. Comparison between 308 nm excimer light alone versus 308 nm excimer light and platelet-rich plasma in the treatment for localized vitiligo. Journal of Cosmetic Dermatology. 2022 Jul;21(7):2826–2831.
- Koh MJ, Mok ZR, Chong WS. Phototherapy for the treatment of vitiligo in Asian children. Pediatric Dermatology. 2015 Mar;32(2):192–197.
- Sun Y, Wu Y, Xiao B, et al. Treatment of 308-nm excimer laser on vitiligo: a systemic review of randomized controlled trials. Journal of Dermatological Treatment. 2015 Jul 4;26(4):347–353.
- Xiao BH, Wu Y, Sun Y, et al. Treatment of vitiligo with NB-UVB: A systematic review. Journal of Dermatological Treatment. 2015 Jul 4;26(4):340–346.
- Leone G, Iacovelli P, Paro Vidolin A, et al. Monochromatic excimer light 308 nm in the treatment of vitiligo: a pilot study. Journal of the European Academy of Dermatology and Venereology. 2003 Sep;17(5):531–537.
- Arora AK, Dogra S. Narrowband ultraviolet B and beyond: Evolving role of phototherapy in vitiligo. Pigment International. 2015 Jan 1;2(1):9.
- Fai D, Cassano N, Vena GA. Narrow-band UVB phototherapy combined with tacrolimus ointment in vitiligo: a review of 110 patients. Journal of the European Academy of Dermatology and Venereology. 2007 Aug;21(7):916–920.
- Xu AE, Zhang DM, Wei XD, et al. Efficacy and safety of tarcrolimus cream 0.1% in the treatment of vitiligo. International Journal of Dermatology. 2009 Jan;48(1):86–90.
- Fa Y, Lin Y, Chi XJ, et al. Treatment of vitiligo with 308 nm excimer laser: our experience from a 2-year follow-up of 979 Chinese patients. Journal of the European Academy of Dermatology and Venereology. 2017 Feb;31(2):337–340.

