 J Clin Aesthet Dermatol. 2023;16(3):30–31.
J Clin Aesthet Dermatol. 2023;16(3):30–31.
by Yasuhiro Horiuchi, MD
Dr. Horiuchi is with the Division of Dermatology at Tsuruse Orthopedic Clinic in Saitama, Japan.
FUNDING: No funding was provided for this article
DISCLOSURES: The author reports no conflicts of interest relevant to the content of this article.
Post-acne scarring in severe acne is a major aesthetic problem that can impair a patient’s quality of life. It has been pointed out that blocking mast cell function with tranilast can prevent or minimize scarring and can be a satisfactory therapeutic strategy. Mast cells are prominent in acne lesions, and their involvement in scar formation has also been specified. Here, we discuss the importance of mast cell control in suppressing post-acne scar formation.
KEYWORDS: Severe acne, scar formation, mast cells, tranilast
Acne vulgaris1 is a common inflammatory skin disease. Despite daily treatments,1 such as topical and/or systemic antibiotics and retinoids,2 it is still not completely treatable. Severe acne is characterized by cysts, nodules, or nodulo-cystic lesions, with post-acne scarring as a problematic issue,3 emphasizing the need for earlier adequate therapy to minimize scarring caused by severe acne. The author recently reported the usefulness of combination minocycline and tranilast for preventing post-acne scarring in patients with severe acne.4 Recently, the involvement of mast cells in acne lesions has been reported, although very rarely.5,6 Tranilast has been shown to suppress mast cell degranulation, thereby minimizing and inhibiting acne scar formation. These results, combined with those of previous studies that examined combined treatments, indicate the importance of suppressing mast cell activation.
Tranilast for Preventing Acne Scarring
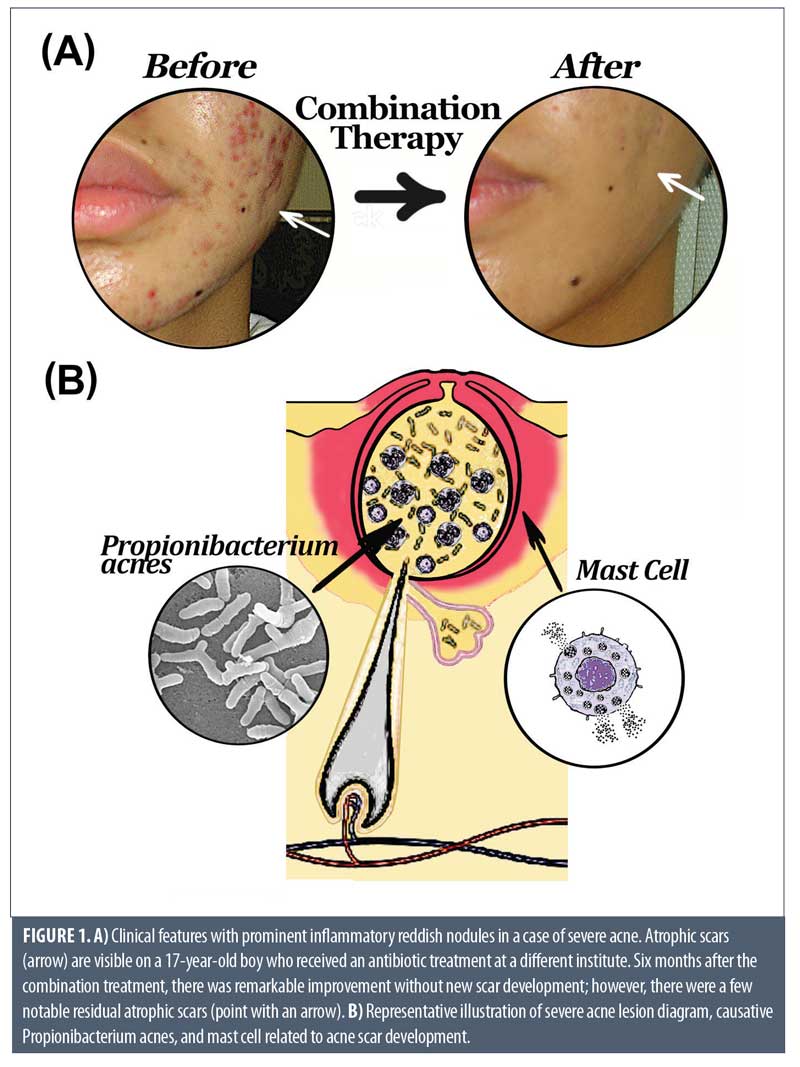
Tranilast,7 (N-[3,4-dimethoxycinnamoyl]-anthranilic acid), initially marketed as an anti-allergic agent, inhibits degranulation of mast cells and can regulate mast cell-derived mediators. Mast cells contribute to allergic reaction via a number of biological processes and its derived mediators,7 such as transforming growth factor (TGF)-β 1 from keloid fibroblasts, which enhances collagen synthesis in keloid fibroblasts in hypertrophic scar tissue, and can regulate the remodeling stages of wound healing.8 Therefore, blocking mast cell function by tranilast can prevent or minimize scarring and can be a satisfactory therapeutic strategy.9 The addition of tranilast and suppression of excessive activation of lesional fibroblasts can prevent post-acne scar formation. Unfortunately, post-acne scar formation is a major problem for patients, particularly in terms of aesthetics,3 which can impair their quality of life. For example, the daily combined use of tranilast with antibiotics can treat severe acne and prevents the formation of new scars (Figure 1A). By contrast, a single treatment with oral and/or externally administered antibiotics causes atrophic scars (Figure 1A). Thus, the combined use of tranilast with antibiotics will be evaluated for its usefulness as a daily treatment in order to suppress and minimize scar formation in severe acne cases.
Acne and Mast Cells
Although treatments for countermeasures are being considered, the involvement of mast cells in the development of acne scars has received little attention or research. Eliasse et al5 reported that acne lesions in the early stage were detected as prominent activated mast cells producing IL-17, clearing pathogens during host defense reactions, and triggering inflammatory events against sebum overproduction and a lesional dysbiosis involving Propionibacterium acnes (Figure 1B).1 Toyoda and Morohashi6 also noted that in inflammatory acne lesions, an increase in the number of mast cells was noted, and on the sebaceous glands, inflammatory reactions can be influenced not only purulent inflammation due to bacteria, but also via mast cell activation, probably resulting in scar development. In addition, they pointed out that the dermal levels of neuropeptides, such as sensory neuropeptide and pruritic mediator substance P from mast cells may stimulate lipogenesis of the sebaceous glands.6 Since acne mainly occurs on the face, it may be difficult to examine the lesioned tissue; therefore, mast cells in acne may not always be histopathologically examined and confirmed. Further studies will be needed on how such mast cell chemical mediators, such as sensory neuropeptides,6 are involved in acne scarring.
Conclusion
Based on these findings, more attention should be paid to the involvement and control of mast cells in the development of scarring in severe acne (Figure 1B). Tranilast is a daily medical agent that has been approved in Japan for more than 30 years, and the author believes that it can be widely and safely applied in conventional practice.
References
- Moradi Tuchayi S, Makrantonaki E, Ganceviciene R, et al. Acne vulgaris. Nat Rev Dis Primers. 2015;1:15029.
- Ghoshal L, Banerjee S, Ghosh SK, et al. Comparative evaluation of effectiveness of adapalene and azithromycin, alone or in combination, in acne vulgaris. Ind J Dermatol. 2007; 52(4): 179–183.
- Layton AM, Henderson CA, Cunliffe WJ. A clinical evaluation of acne scarring and its incidence. Clin Exp Dermatol. 1994; 19(4):303–308.
- Horiuchi Y. Tranilast and minocycline combination for intractable severe acne and prevention of postacne scarring. A case series.Am J Ther. 2022;29(6):e779-e780.
- Eliasse Y, Leveque E, Garidou L, et al. IL-17 + mast cell/T helper cell axis in the early stages of acne. Front Immunol. 2021;12:740540.
- Toyoda M, Morohashi M. New aspects in acne inflammation. Dermatology. 2003; 206(1):17–23.
- Suzawa H, Kikuchi S, Arai N, et al. The mechanism involved in the inhibitory action of tranilast on collagen biosynthesis of keloid fibroblasts. Jpn J Pharmacol. 1992; 60(2): 91–96.
- Komi DEA, Khomtchouk K, Santa Maria PL. A review of the contribution of mast cells in wound healing: Involved molecular and cellular mechanisms. Clin Rev Allergy Immunol. 2020 Jun;58(3):298-312.
- Horiuchi Y. Tranilast for preventing scar formation: A renewed therapeutic option. J Dermatol Res Ther. 2021;7:099.
Importance of Mast Cell Activation Control for Preventing Scar Formation in Severe Acne
Categories:
by Yasuhiro Horiuchi, MD
Dr. Horiuchi is with the Division of Dermatology at Tsuruse Orthopedic Clinic in Saitama, Japan.
FUNDING: No funding was provided for this article
DISCLOSURES: The author reports no conflicts of interest relevant to the content of this article.
Post-acne scarring in severe acne is a major aesthetic problem that can impair a patient’s quality of life. It has been pointed out that blocking mast cell function with tranilast can prevent or minimize scarring and can be a satisfactory therapeutic strategy. Mast cells are prominent in acne lesions, and their involvement in scar formation has also been specified. Here, we discuss the importance of mast cell control in suppressing post-acne scar formation.
KEYWORDS: Severe acne, scar formation, mast cells, tranilast
Acne vulgaris1 is a common inflammatory skin disease. Despite daily treatments,1 such as topical and/or systemic antibiotics and retinoids,2 it is still not completely treatable. Severe acne is characterized by cysts, nodules, or nodulo-cystic lesions, with post-acne scarring as a problematic issue,3 emphasizing the need for earlier adequate therapy to minimize scarring caused by severe acne. The author recently reported the usefulness of combination minocycline and tranilast for preventing post-acne scarring in patients with severe acne.4 Recently, the involvement of mast cells in acne lesions has been reported, although very rarely.5,6 Tranilast has been shown to suppress mast cell degranulation, thereby minimizing and inhibiting acne scar formation. These results, combined with those of previous studies that examined combined treatments, indicate the importance of suppressing mast cell activation.
Tranilast for Preventing Acne Scarring
Tranilast,7 (N-[3,4-dimethoxycinnamoyl]-anthranilic acid), initially marketed as an anti-allergic agent, inhibits degranulation of mast cells and can regulate mast cell-derived mediators. Mast cells contribute to allergic reaction via a number of biological processes and its derived mediators,7 such as transforming growth factor (TGF)-β 1 from keloid fibroblasts, which enhances collagen synthesis in keloid fibroblasts in hypertrophic scar tissue, and can regulate the remodeling stages of wound healing.8 Therefore, blocking mast cell function by tranilast can prevent or minimize scarring and can be a satisfactory therapeutic strategy.9 The addition of tranilast and suppression of excessive activation of lesional fibroblasts can prevent post-acne scar formation. Unfortunately, post-acne scar formation is a major problem for patients, particularly in terms of aesthetics,3 which can impair their quality of life. For example, the daily combined use of tranilast with antibiotics can treat severe acne and prevents the formation of new scars (Figure 1A). By contrast, a single treatment with oral and/or externally administered antibiotics causes atrophic scars (Figure 1A). Thus, the combined use of tranilast with antibiotics will be evaluated for its usefulness as a daily treatment in order to suppress and minimize scar formation in severe acne cases.
Acne and Mast Cells
Although treatments for countermeasures are being considered, the involvement of mast cells in the development of acne scars has received little attention or research. Eliasse et al5 reported that acne lesions in the early stage were detected as prominent activated mast cells producing IL-17, clearing pathogens during host defense reactions, and triggering inflammatory events against sebum overproduction and a lesional dysbiosis involving Propionibacterium acnes (Figure 1B).1 Toyoda and Morohashi6 also noted that in inflammatory acne lesions, an increase in the number of mast cells was noted, and on the sebaceous glands, inflammatory reactions can be influenced not only purulent inflammation due to bacteria, but also via mast cell activation, probably resulting in scar development. In addition, they pointed out that the dermal levels of neuropeptides, such as sensory neuropeptide and pruritic mediator substance P from mast cells may stimulate lipogenesis of the sebaceous glands.6 Since acne mainly occurs on the face, it may be difficult to examine the lesioned tissue; therefore, mast cells in acne may not always be histopathologically examined and confirmed. Further studies will be needed on how such mast cell chemical mediators, such as sensory neuropeptides,6 are involved in acne scarring.
Conclusion
Based on these findings, more attention should be paid to the involvement and control of mast cells in the development of scarring in severe acne (Figure 1B). Tranilast is a daily medical agent that has been approved in Japan for more than 30 years, and the author believes that it can be widely and safely applied in conventional practice.
References
Share:
Recent Articles:
Categories:
Recent Articles:
Tags: