J Clin Aesthet Dermatol. 2020;13(2):E69–E75
 by Swapnil Shah, MD; Jagadish Sakhiya, MD; Pranoti Deshpande, MD; Dhruv Sakhiya, MBBS; and Arun C. Inamadar, MD
by Swapnil Shah, MD; Jagadish Sakhiya, MD; Pranoti Deshpande, MD; Dhruv Sakhiya, MBBS; and Arun C. Inamadar, MD
Dr. Shah is with the Ashwini Rural Medical College Hospital and Research Center Solapur in Maharashtra, India. Drs J. Sakhiya and D. Sakhiya are with Sakhiya Skin Clinic in Surat, India. Dr. Deshpande is with VM Medical College in Solpaur, India. Dr. Inamdar is with MB Patil Medical College, in Vijaypura, Karnataka, India.
FUNDING: No funding was provided for this study.
DISCLOSURES: The authors have no conflicts of interest relevant to the content of this article.
ABSTRACT: Background. Vitiligo is an acquired disorder characterized by depigmented macules or patches on the skin due to the loss of functional melanocytes. Segmental vitiligo (SV) is a subtype of vitiligo refractory to treatment.
Objective. We studied safety and efficacy of 308-nm monochromatic excimer light (MEL) in combination with 0.1% tacrolimus ointment for the treatment of SV.
Methods. Fifty patients with SV were enrolled. MEL was given on alternate dates in combination with topical tacrolimus. Clinical photographs were taken once a month. Two independent dermatologists analyzed and graded the results.
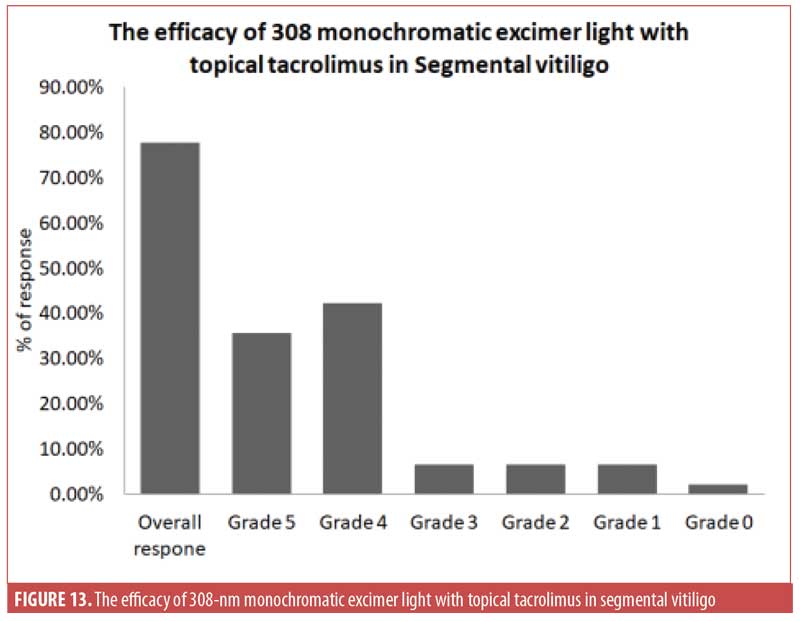
Results.Five patients were lost to follow-up. Concerning overall treatment success, 77.8 percent of patients demonstrated at least 75-percent repigmentation. More specifically, 35.6 percent of patients showed complete (100%) repigmentation (Grade 5), whereas 42.2 percent of patients showed more than 75-percent repigmentation (Grade 4).
Conclusion. Combination therapy with topical 0.1% tacrolimus and a 308-nm excimer lamp appears to be efficacious with a good safety profile. The duration of disease was a statistically significant factor inversely correlated with treatment success rate. The site of vitiligo also plays a significant part in the outcome, as facial lesions responded best to the treatment.
Key words: Monochromatic excimer light, skin pigmentation, tacrolimus, vitiligo
Vitiligo is an acquired pigmentation disorder characterized by depigmented macules or patches on the skin due to the loss of functional melanocytes. It affects around 0.5 percent of the global population.1 Vitiligo is classified as either focal, generalized, or segmental. While various treatments, such as topical steroids, topical calcineurin inhibitors, psoralen ultraviolet A, and narrowband ultraviolet B are effective in repigmenting focal and generalized vitiligo, their efficacy in segmental vitiligo (SV) is more limited.2 SV is usually refractory to treatment and surgical intervention is a preferred intervention modality.3 However, though surgery often results in satisfactory repigmentation in most cases, it is difficult to conduct in children and is often associated with complications, including color mismatch, cobblestoning, and donor site scarring.4
The excimer laser has been used previously in the treatment of vitiligo, including SV, and can target lesions individually, thus facilitating the delivery of higher fluences and providing better protection to the surrounding normal skin. Excimer laser application alone is not beneficial in the treatment of SV.5 However, in recent reports, it has been demonstrated to be effective in the treatment of SV in combination with a topical steroid or topical calcineurin inhibitor.6–8
Topical calcineurin inhibitors, which act by immunomodulation, are useful in vitiligo and promote repigmentation without causing systemic immunosuppression.9
A 308-nm monochromatic excimer lamp (MEL) shares a similar mechanism of action as that of the 308-nm excimer laser.10 In this study, we examined the application of MEL in combination with topical tacrolimus 0.1% ointment for the treatment of SV.
Materials and Methods
This study was conducted in a dermatology clinic in central India. Ethical clearance was obtained and informed consent and photoconsent was obtained from the participating patients. A total of 50 consecutive patients clinically diagnosed with SV were included in this study; however, five patients were lost to follow-up after one month and were excluded from the study. Patients excluded from this study were those with generalized vitiligo, those previously treated with any form of phototherapy in the previous three months, those with a history of using immunosuppressive or photosensitizing agents, and those who had undergone any surgery for vitiligo.
Treatment. After providing informed consent, all patients were treated with xenon chloride 308-nm MEL (Exciplex; Clarteis, Antipolis, France). The spot size available with this system was 5×5cm. A suitable silicone stencil of the size of SV was used to protect the surrounding skin from burns and to avoid perilesional hyperpigmentation. Treatment was started with a fluence of 100MJ/cm2 and was increased by 50MJ/cm2 per session until slight erythema appeared after 24 hours. If intense erythema was present for more than 48 hours, the next session was skipped until the erythema resolved and the dose was reduced by 100MJ/cm2. The reduced dose was continued for the following two sessions and then it was increased by 50MJ/cm2. Treatment was administered 2 to 3 times per week on nonconsecutive days. Additionally, patients were instructed to use tacrolimus 0.1% ointment twice a day on the affected areas. If the patient did not show any pigmentation after undergoing 15 to 20 sessions of MEL irradiation, the case was ruled as a treatment failure. In addition, treatment was discontinued if, after the initial response, there was no progress in repigmentation after 10 to15 consecutive sessions.
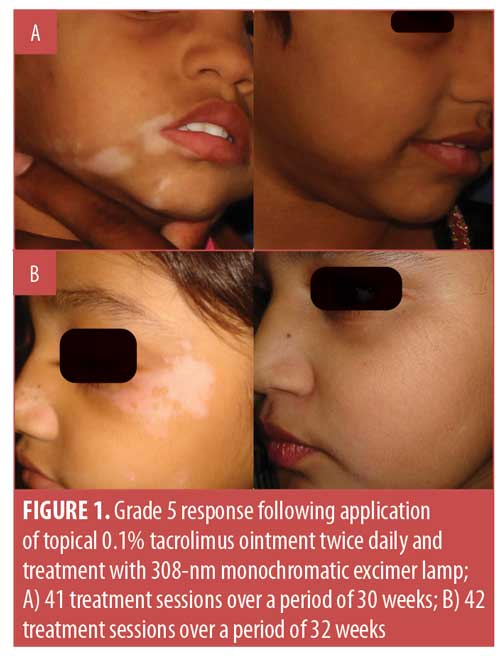
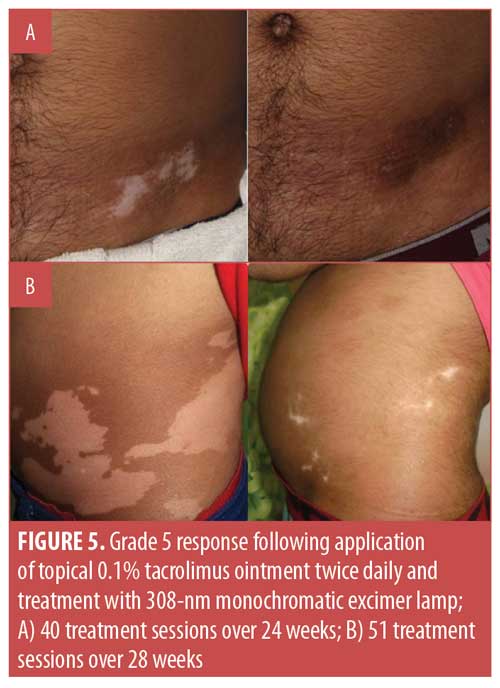
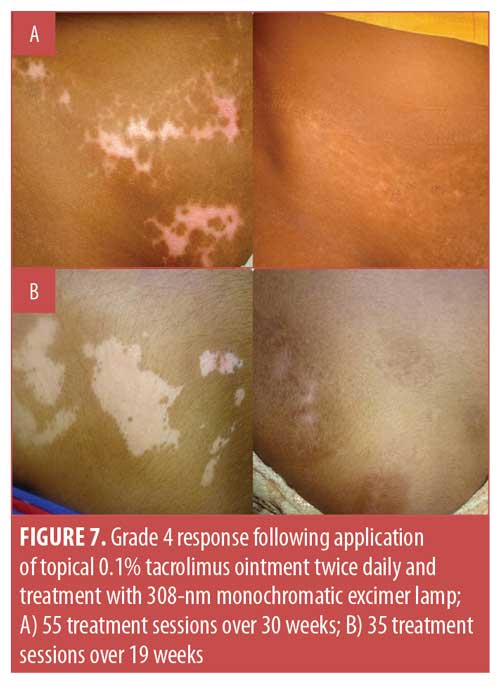
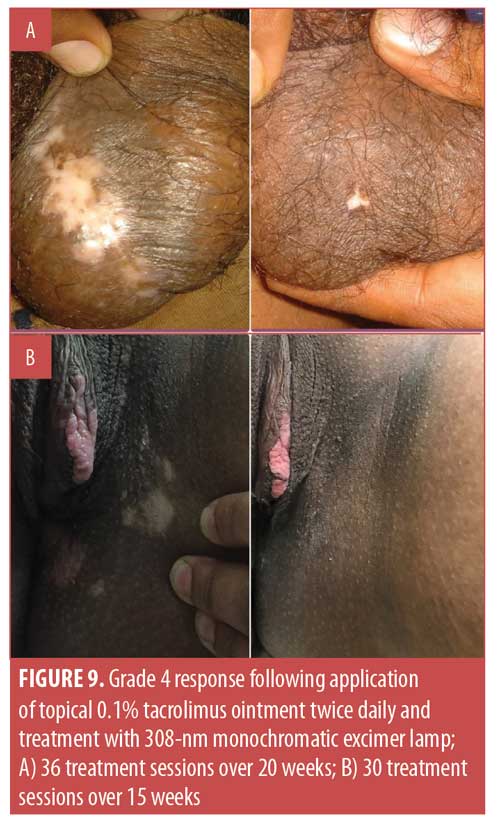
For analysis purposes, clinical photographs of all the patients were taken once a month, and two independent dermatologists evaluated the results by reviewing these photographs. Repigmentation was graded as follows: Grade 0 (no repigmentation), Grade 1 (1% to 25% repigmentation), Grade 2 (25% to 50% repigmentation), Grade 3, (50% to 75% repigmentation), Grade 4 (75% to 99% repigmentation), and Grade 5 (100% repigmentation).
Any side effects observed during the treatment period were also recorded.
Statistical analysis. Univariable and multivariable logistic regression were performed using the Statistical Package for the Social Sciences version 21 software program (IBM Corp., Armonk, New York) in a series to determine the independent prognostic factors associated with treatment success. The Microsoft Excel 2007 edition (Microsoft Corp., Redmond, Washington) was used to calculate odds ratios (ORs) and 95% confidence intervals (CIs).
Results
The demographic details of the 45 SV patients analyzed in the present study are presented in Table 1. In our study, female patients outnumbered male patients, with a ratio of 2.4:1. The average age of onset of SV was 18 years, with the youngest subject being three years old and the oldest being 60 years old. The average duration of the disease at the time of this study was 16 months. Most of the patients (n=21/45; 46.6%) presented with vitiligo lesions on the face, followed by seven who presented with lesions on the waist (15.6%) and six who presented with lesions on the neck (13.3%).
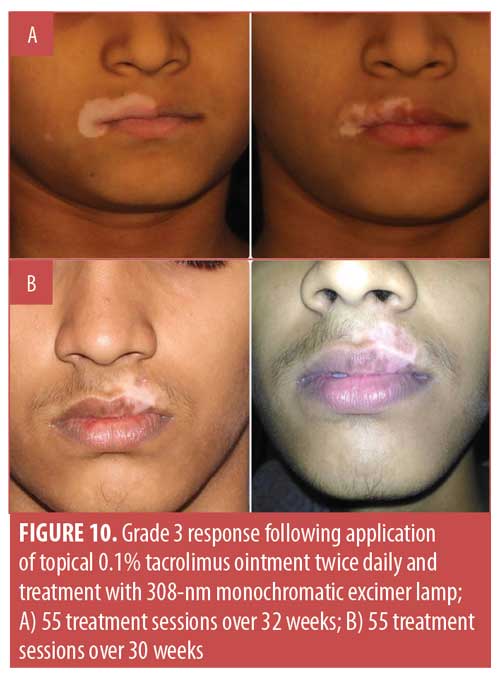
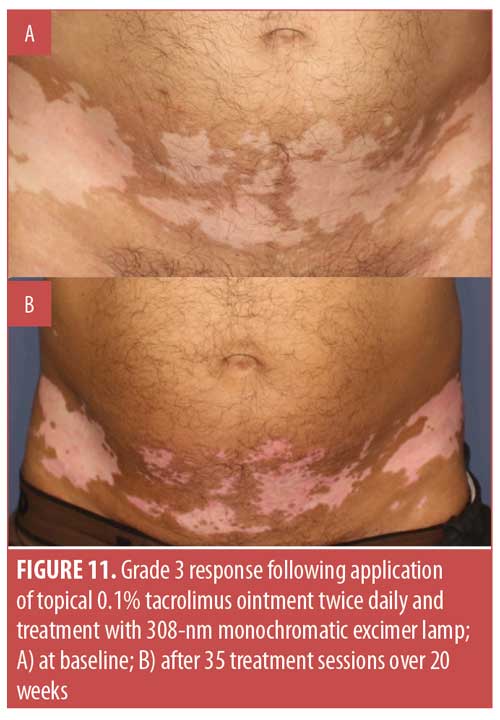
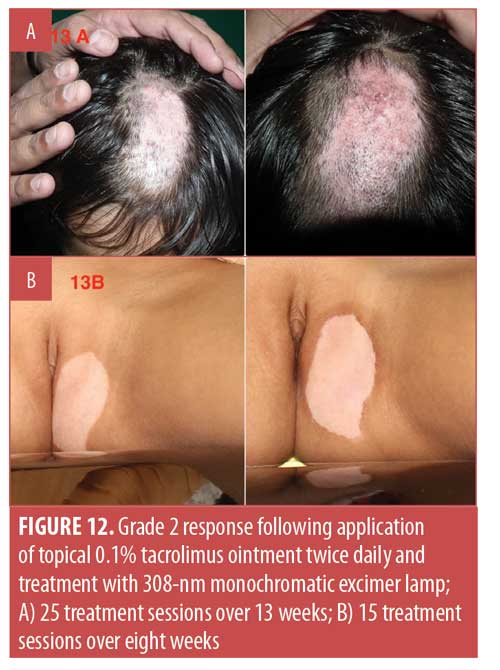
Considering the overall treatment success, the percentage of patients showing at least 75-percent repigmentation in the total population was 77.8 percent (n=35). Separately, 35.6 percent (n=16) of patients demonstrated 100-percent repigmentation (Grade 5) (Figures 1–5), whereas 42.2 percent (n=19) of patients showed more than 75-percent repigmentation (Grade 4) (Figures 6–9). Meanwhile, 6.7 percent (n=3), 6.7 percent (n=3) and 2.2 percent (n=1) showed Grades 3, 2, and 1 responses, respectively (Figures 10–12). The overall rate of response to the combination therapy of 308-nm monochromatic excimer light with topical tacrolimus in SV is shown in Table 2, while a graphical representation is presented in Figure 13.
In the univariable analysis, disease duration of six months or less (OR: 4.80, 95% CI: 1.36–16.78; p=0.01), final dose of 300 to 900mJ (OR: 4.90, 95% CI: 1.49–16.28; p=0.01), completion of 20 or less treatment sessions (OR: 8.50, 95% CI: 1.42–49.40; p=0.02 ), average energy of less than 400mJ (OR: 16.78, 95% CI: 2.05–137, p=0.01) and face and waist as the most common site of vitiligo (OR: 188.67, 95% CI: 3.13–11,271.13; p=0.01 for face and OR: 105.64, 95% CI: 1.55–7,269.01; p=0.03 for waist) were statistically significant covariates negatively associated with the success of the combination therapy treatment (Table 3).
During the multivariable analysis, final dose of 300 to 900mJ (OR: 15.96, 95% CI: 1.72–148.41; p=0.02) and waist or groin as the site of vitiligo (OR: 237.46, 95% CI: 1.73–32,869.62; p=0.03 for waist and OR: 0.11, 95% CI: 0.00–22.87; p=0.02 for groin) were identified as independent factors associated with the efficacy of the combination therapy (Table 3).
The age-based analysis showed that the success rate for childhood-onset vitiligo (i.e., occurring at an age younger than 12 years) was 80.95 percent (n=17/21), whereas that among adult patients (i.e., occurring at an age older than 12 years) was 75 percent (n=18/24).
Out of 45 patients, nine (20%) experienced an adverse event related to the combination therapy, while 36 (80%) patients had no issues. Out of the nine patients who showed complications, erythema was observed in three (33.3%) patients, crusting occurred in two (22.2%) patients, erythema and blistering were seen in one (11.1%) patient, perilesional hyperpigmentation was seen in one (11.1%) patient, blistering was observed in one (11.1%) patient, and postinflammatory hyperpigmentation was observed in one (11.1%) patient.





Discussion
An excimer laser uses the combination of a noble gas (e.g., argon, krypton, or xenon) and a reactive gas (e.g., fluorine or chlorine). An excimer (i.e., excited dimer) is a short-lived molecule formed from two species, at least one of which is in an electronically excited state. Diatomic complexes involving a noble gas and a halide, such as xenon chloride, are common in the construction of excimer lasers.10 Under appropriate conditions of electrical stimulation and high pressure, a pseudo-molecule called an excimer is created, which can only exist in an energized state and which releases energy in the form of ultraviolet light upon returning to the ground state.11 By definition, the atoms of an excimer molecule are two or more atoms of the same chemical element. In the case of atoms of different elements (e.g., xenon chloride), the phenomenon is called an “exciplex.”12
Xenon chloride excimer laser or MEL emits monochromatic radiation with a wavelength of 308 nm. MEL differs from laser since the light emitted is noncoherent and noncollimated. However, it still has the medically relevant characteristic of monochromaticity required for treatment of vitiligo. MEL is found to be more erythemogenic than an excimer laser.10
Excimer laser and MEL have similar mechanisms of action. The 308-nm wavelength impacts nuclear DNA, which acts as a chromophore, facilitating DNA breakage and leading to a decrease in T-cell proliferation.13 Such also upregulates the tumor suppressor gene p53, thereby causing cell-cycle arrest and apoptosis.14 Apart from these immunological actions, it is also hypothesized to cause melanocyte migration and proliferation from an increase in peptide endothelin-1 in keratinocytes.15
MEL has certain advantages over excimer laser, such as cost. Excimer lasers have a recurring cost involving the change of potential toxic gases. In MEL, the active medium, xenon chloride, is hermetically sealed in a glass tube and does not need to be changed. The laser has a smaller spot size relative to light. It also raises a variety of safety issues due to high-voltage discharges and the disposal of potentially toxic gases. Further, MEL has several advantages over standard narrowband ultraviolet B therapy, which is slow-acting, requires significant office space, and is difficult to use in pediatric cases. Since exposure to normal skin is prevented with treatment by MEL, supraerythemogenic doses can be used. The modality occupies less space and the treatment is relatively faster. MEL is superior to narrowband ultraviolet B phototherapy in the induction of T-cell apoptosis.16 Le Duff et al10 and Qiong Shi et al17 showed similar efficacy of excimer laser and MEL in the treatment of vitiligo. Casacci et al18 reported that the excimer lamp was more effective than narrowband ultraviolet B.
Topical tacrolimus is an excellent immunomodulator. It downregulates various proinflammatory cytokines, such as interleukin (IL)-2, IL-3, IL-4, IL-5, interferon-c, tumor necrosis factor alpha, and granulocyte-stimulating factors. It enhances the proliferation and migration of melanocytes.9,19
Tacrolimus ointment, when used as a monotherapy, produces a variable but unsatisfactory response in patients with SV.20 However, various studies have demonstrated the effectiveness of combination treatment with tacrolimus and excimer laser or lamp in vitiligo.8,21
SV is a type of vitiligo characterized by depigmented macules or patches arranged in a patterned distribution. It constitutes 5 to 27.9 percent of studied cases of vitiligo.22,23 It accounts for 30 percent of cases of childhood vitiligo.24 An Indian study reported a prevalence of 6.7 percent among patients with vitiligo in India.25 It has an early onset in childhood. The lesions develop rapidly over a short period of time in a localized area, then remain stable. The pattern of distribution of lesions can be dermatomal, blaschkoid, phylloid, or checkerboard.26,27 Several hypotheses have been proposed for the etiopathogenesis of SV, including neuronal mechanism, somatic mosaicism, microvascular skin-homing, and a combination three-step theory.28 There is a lower incidence of autoimmunity and family history in SV.29,30 It responds poorly to medical treatment. However, when treated early after onset, the lesions seem to be more sensitive to the therapy.31 In one study, a potent topical corticosteroid was reported to provoke over 50-percent repigmentation in 34.2 percent of patients.32 Surgical therapy alone or in combination with adjuvant medical treatment often produces a satisfactory response in SV.33,34
In the present study of 45 patients with SV, female patients outnumbered male patients. This might be due to a greater desire for treatment among female patients due to social stigma.
The response to phototherapy, either with PUVA,35 311-nm narrow-band ultraviolet B,36 or excimer laser is poorer in patients with SV than in those with non-SV.5 However, a retrospective study by Bae Jung et al6 reported more than 75-percent repigmentation in 50 percent of their patients.6 They used a combination of treatment, including excimer laser, topical tacrolimus, and a short course of oral steroids. In the present study, 16 (35.6%) patients demonstrated complete repigmentation and 19 (42.2%) patients showed 75 to 99-percent repigmentation. The overall response to treatment was 77.8 percent, with only one patient not showing any repigmentation. The present study protocol did not use systemic steroids.
Disease duration was a statistically significant factor in the outcome of SV. Disease duration was negatively correlated with the success of treatment.28 Bae Jung et al6 reported that a disease duration of more than 12 months was an independent prognostic factor in the outcome of the disease. In our study, a disease duration of more than six months negatively affected the success rate. The site of involvement is also an important factor in the treatment outcome.37 Patients with facial lesions respond faster to treatment relative to those with acral lesions. The present study found that facial lesions and lesions on the waist responded significantly better to the treatment. The varying responsiveness seen in different lesion sites might be influenced by disease duration, as patients with facial lesions tended to present earlier for treatment than patients with lesions elsewhere. Children responded better to treatment than adults, but the difference was not statistically significant. The final dose of MEL and the number of treatment sessions were inversely related with the response rate in the present study. The procedure was well-tolerated without significant side effects. Mild side effects, such as erythema and perilesional hyperpigmentation were noted and resolved without any intervention. None of the patients dropped out from the study because of their side effects. The limitations of our study were its small sample size and lack of control group.
Conclusion
SV responds poorly to treatment, making surgical modalities the mainstay of treatment. Due to certain complications related to surgery and the difficulty in conducting procedures in children, 308-nm MEL was examined in this study. It is less expensive, faster, compact for use, and safer, targeting only the lesions of interest. As combination therapies work best for vitiligo, 308-nm excimer lamp and topical immunomodulator 0.1% tacrolimus were combined. This combination was found to be efficacious and safe if started early on in the course of the disease.
References
- Taïeb A, Picardo M. Clinical practice. Vitiligo. N Engl J Med. 2009; 360(2):160–169.
- Alikhan A, Felsten LM, Daly M, et al. Vitiligo: a comprehensive overview Part I. Introduction, epidemiology, quality of life, diagnosis, differential diagnosis, associations, histopathology, etiology, and work-up. J Am Acad Dermatol. 2011;65(3):473–491.
- Lee DY, Kin CR, Park JH, et al. The incidence of leukotrichia in segmental vitiligo: implication of poor response to medical treatment. Int J Dermatol. 2011;50(8):925–927.
- Lee DY, Park JH, Lee JH, et al. Surgical treatment is indicated in long-duration segmental vitiligo. Dermatol Surg. 2010;36(4):568–569.
- Do JE, Shin JY, Kim DY, et al. The effect of 308nm excimer laser on segmental vitiligo: a retrospective study of 80patients with segmental vitiligo. Photodermatol Photoimmunol Photomed. 2011;27(3):147–151.
- Bae JM, Yoo HJ, Kim H, et al. Combination therapy with 308-nm excimer laser, topical tacrolimus, and short-term systemic corticosteroids for segmental vitiligo: a retrospective study of 159 patients. J Am Acad Dermatol. 2015;73(1):76–82.
- Passeron T, Ortonne JP. Use of the 308-nm excimer laser for psoriasis and vitiligo. Clin Dermatol. 2006;24(1):33–42.
- Li L, Liang Y, Hong J, et al. The effectiveness of topical therapy combined with 308-nm excimer laser on vitiligo compared to excimer laser monotherapy in pediatric patients. Pediatr Dermatol. 2019;36(1):e53–e55.
- Lan CC, Chen GS, Chiou MH, et al. FK506 promotes melanocyte and melanoblast growth and creates a favourable milieu for cell migration via keratinocytes: possible mechanisms of how tacrolimus ointment induces repigmentation in patients with vitiligo. Br J Dermatol. 2005;153(3):498–505.
- Le Duff F, Fontas E, Giacchero D, et al. 308-nm excimer lamp vs. 308-nm excimer laser for treating vitiligo: a randomized study. Br J Dermatol. 2010;163(1):188–192.
- Park KK, Liao W, Murase JE. A review of monochromatic excimer light in vitiligo. Br J Dermatol. 2012;167(3):468–478.
- Spencer JM, Hadi SM. The excimer lasers. J Drugs Dermatol. 2004;3(5):522–525.
- Beggs S, Short J, Rengifo-Pardo M, Ehrlich A. Applications of the excimer laser: a review. Dermatol Surg. 2015;41(11):1201–1211.
- Bulat V, Situm M, Deiol I, et al. The mechanisms of action of phototherapy in the treatment of the most common dermatoses. Coll Antropol. 2011;35(Suppl 2):147–151.
- Pacifico A, Leone G. Photo(chemo)therapy for vitiligo. Photodermatol Photoimmunol Photomed. 2011;27(5):261–277.
- Ozawa M, Ferenczi K, Kikuchi T et al. 312-nanometer ultraviolet B light (narrow-band UVB) induces apoptosis of T cells within psoriatic lesions. J Exp Med. 1999;189(4):711–718.
- Shi Q, Li K, Fu J, et al. Comparison of the 308-nm excimer laser with the 308-nm excimer lamp in the treatment of vitiligo—a randomized bilateral comparison study. Photodermatol Photoimmunol Photomed. 2013;29(1):27–33.
- Casacci M, Thomas P, Pacifico A, et al. Comparison between 308 nm monochromatic excimer light and narrowband UVB phototherapy (311–313 nm) in the treatment of vitiligo—a multicentre controlled study. J Eur Acad Dermatol Venereol. 2007;21(7):956–963.
- Jung H, Oh ES. FK506 positively regulates the migratory potential of melanocyte-derived cells by enhancing syndecan-2 expression. Pigment Cell Melanoma Res. 2016;29(4):434–443.
- Kathuria S, Khaitan BK, Ramam M, Sharma VK. Segmental vitiligo: a randomized controlled trial to evaluate efficacy and safety of 0.1% tacrolimus ointment vs 0.05% fluticasone propionate cream. Indian J Dermatol Venereol Leprol. 2012;78(1):68–73.
- Wu Y, Sun Y, Qiu L, et al. A multi-centre, randomized, split-face and/or neck comparison of 308-nm excimer laser and 0.1% tacrolimus ointment for stable vitiligo, plus intramuscular slow-releasing betamethasone for active vitiligo. Br J Dermatol. 2019;181(1):210–211.
- el-Mofty AM, el-Mofty M. Vitiligo A symptom complex. Int J Dermatol. 1980;19(5):237–244.
- Koga M, Tango T. Clinical features and course of type A and type B vitiligo. Br J Dermatol. 1988;118(2):223–228.
- Hann SK, Lee HJ. Segmental vitiligo: clinical findings in 208 patients. J Am Acad Dermatol. 1996; 35(5 Pt 1):671–674.
- Khaitan BK, Pasricha JS, Sood A. clinical profile of 450 Indian vitiligo patients. American Academy of Dermatology 61st Annual Meeting; March 21–26, 2003; San Francisco, CA.
- van Geel N, Bosma S, Boone B, et al. Classification of segmental vitiligo on the trunk. Br J Dermatol. 2014;170(2):322–327.
- Kim DY, Oh SH, Hann SK. Classification of segmental vitiligo on the face: clues for prognosis. Br J Dermatol. 2011;164(5):1004–1009.
- van Geel N, Speeckaert R. Segmental vitiligo. Dermatol Clin. 2017;35(2):145–150.
- Khaitan BK, Kathuria S, Ramam M. A descriptive study to characterize segmental vitiligo. Indian J Dermatol Venereol Leprol. 2012;78(6):715–721.
- Ezzedine K, Diallo A, Léauté-Labrèze C, et al. Multivariate analysis of factors associated with early-onset segmental and nonsegmental vitiligo: a prospective observational study of 213 patients. Br J Dermatol. 2011;165(1):44–49.
- Park JH, Park SW, Lee DY, et al. The effectiveness of early treatment in segmental vitiligo: retrospective study according to disease duration. Photodermatol Photoimmunol Photomed. 2013;29(2):103–105.
- Khalid M, Mujtaba G. Response of segmental vitiligo to 0.05% clobetasol propionate cream. Int J Dermatol. 1998;37(9):705–708 .
- Lee DY, Park JH, Lee JH, et al. Surgical treatment is indicated in long-duration segmental vitiligo. Dermatol Surg. 2010;36(4):568–569.
- Mulekar SV. A long-term follow-up study of segmental and focal vitiligo treated by autologous, non- cultured melanocyte keratinocyte cell transplantation. Arch Dermatol. 2004;140(10):1211–1215.
- Tallab T, Joharji H, Bahamdan K, et al. Response of vitiligo to PUVA therapy in Saudi patients. Int J Dermatol. 2005;44(7):556–558.
- Anbar TS, Westerhof W, Abdel-Rahman AT, El-Khayyat MA. Evaluation of the effects of NB-UVB in both segmental and non-segmental vitiligo affecting different body sites. Photodermatol Photoimmunol Photomed. 2006;22(3):157–163.
- Cho S, Zheng Z, Park YK, Roh MR. The 308-nm excimer laser: a promising device for the treatment of childhood vitiligo. Photodermatol Photoimmunol Photomed. 2011;27(1):24–29.

