by Davlouros Sotiris, MD; Graziano Pallotta, PhD, PharmD; Giulio Nittari, PhD, PharmD; and Francesco Amenta, MD
by Davlouros Sotiris, MD; Graziano Pallotta, PhD, PharmD; Giulio Nittari, PhD, PharmD; and Francesco Amenta, MD
Dr. Sotiris is with the University of Pavia in Pavia, Italy and the University of Camerino in Camerino, Italy. Drs. Pallotta, Amenta, and Nittari are with the Telemedicine and Telepharmacy Center at the University of Camerino in Camerino, Italy.
J Clin Aesthet Dermatol. 2020;13(8):E59–E63
FUNDING: No funding was provided for this study.
DISCLOSURES: The authors have no conflicts of interest relevant to the content of this article.
ABSTRACT: Background. The Triplex method is a three-step treatment approach to reducing the appearance of small and medium-sized varicose veins and phlebological imperfections of the lower limbs.
Objective. This study evaluated the effectiveness, duration of results, adverse events, patient satisfaction, and improvements in quality of life in patients with small and medium-sized varicose veins who were treated with the Triplex method.
Methods. We conducted a six-year follow-up study of 4,000 patients from the years 2012 to 2018. Patients with chronic venous insufficiency of the lower limbs were included. Patients with active or previous phlebitis or phlebostatic ulcers were excluded. An average of three sessions was performed on each patient in the Triplex group. Follow-up assessments were performed 1, 3, 6, and 12 months after the completion of the treatment, and they included a morphofunctional study, histological examination, and photographic documentation. The first step of the treatment approach utilized an injectable shrinkage solution consisting of sodium salicylate, physiological solution with 10% glycerol, and lidocaine, which was injected into the varices to trigger a reduction of the vessel lumen. For patients in whom the targeted vessels were not sufficienty narrowed by the shrinkage solution, the second step—ultrasound-guided foam sclerotherapy, or scleromousse—was utilized, which consisted of either lauromacrogol 1% or sodium tetradecyl sulfate 1%, with one group of patients (n=50) receiving the former and the other group of patients (n=50) receiving the latter. All patients were administered Step 3 of the treatment approach, which usually included varicose treatment with low concentrations of sodium tetradecyl sulfate (STS) 0.2 to 0.50% or lauromacrogol 0.25%, with compression additionally prescribed in some patients.
Results. Over a follow-up period of six years, in patients who underwent full Triplex treatment, we observed 1) a greater duration of the narrowing of the vessel’s caliber, with disappearance of the varices; 2) reduced utilization of the foam solution at the reflux point due to the narrowing of the gauge; and 3) no relevant hemodynamic effects emerged in patients with recanalization. In patients who underwent Steps 1 and 2 of the treatment approach, reflux was not hemodynamically significant. No significant differences were observed in the lauromacrogol group of patients compared to the sodium tetradecyl sulfate group.
Conclusion. Compared to patients in whom only scleromousse was performed at the reflux site, the narrowing of the varicose wall that is achieved using the Triplex method is associated with longer lasting results in the treatment of small and medium-sized varicose veins, with physiological recovery of superficial venous circulation.
Keywords: Triplex, varicose veins, telangiectasia, scleromousse, sclerosing
The Triplex method is a treatment approach for small and medium-sized varicose veins and phlebological imperfections of the lower limbs. The name “Triplex” is derived from the three steps involved in this treatment approach: Step 1) injection of a solution containing sodium salicylate and lidocaine into verices to shrink vessel lumen and reduce appearance of varicose veins; Step 2) administration of Doppler ultrasonography-guided injection of a soft-foam laser or a sclerosing solution in patients who did not achieve adequate results with Step 1; and Step 3) sclerotherapy of residual telangiectasia using low concentrations of sodium tetradecyl sulfate (STS) or lauromacrogol.
This study evaluated the effectiveness, duration of results, adverse events, patient satisfaction, and improvements in quality of life in patients who underwent treatment of small and medium-sized varicose veins using the Triplex method.
Methods
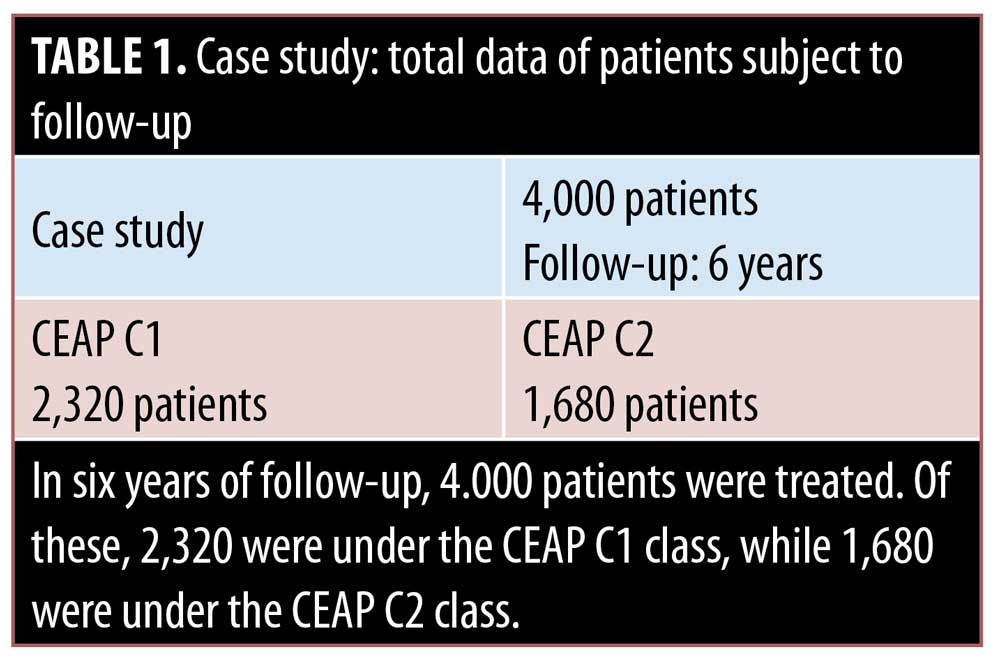
We conducted a six-year follow-up study of 4,000 patients treated at a single center from 2012 to 2018. Patients with chronic venous insufficiency of the lower limbs, classified as C1 or C2 using the CEAP classification system, were included. Patients with active or previous phlebitis or phlebostatic ulcers were excluded.
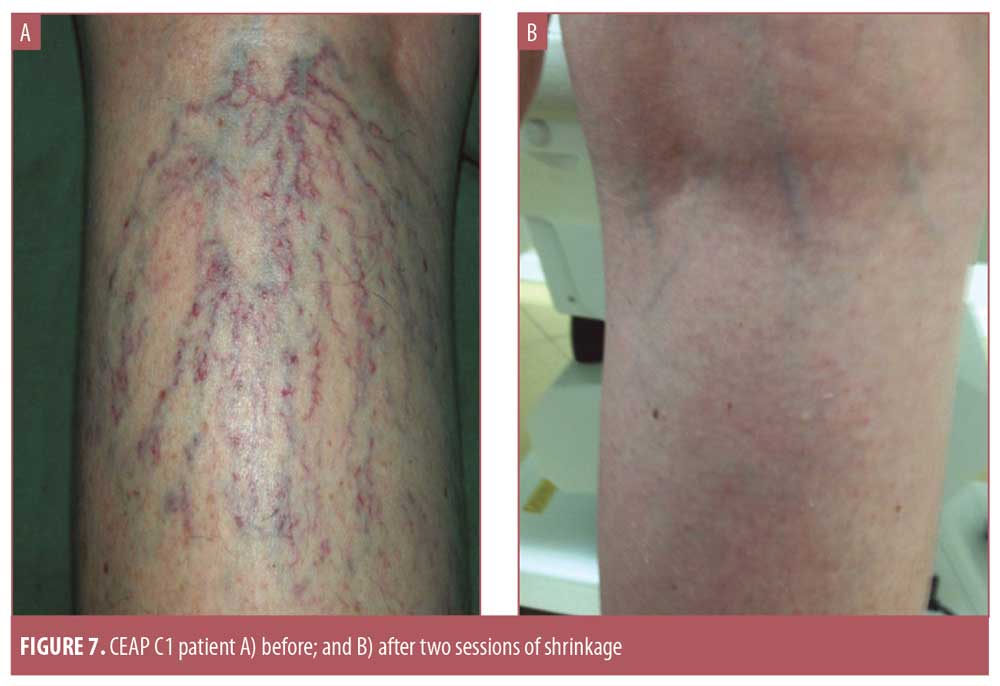
The different manifestations of chronic venous diseases are classified by the Comprehensive Classification System for Chronic Venous Disorders (CEAP), devised by an International Commission of the American Venous Forum and used throughout the world.1 The treatments indicated for C1 patients in the CEAP classification include sclerotherapy and the transdermal-laser, exploiting selective photothermolysis. In our study, 2,320 patients were classified as C1. According to the CEAP classification, C1 patients are those with “venous disturbance,” telangiectasias, and reticular veins; C2 patients present with varicose veins, swelling, and nocturnal cramps.1
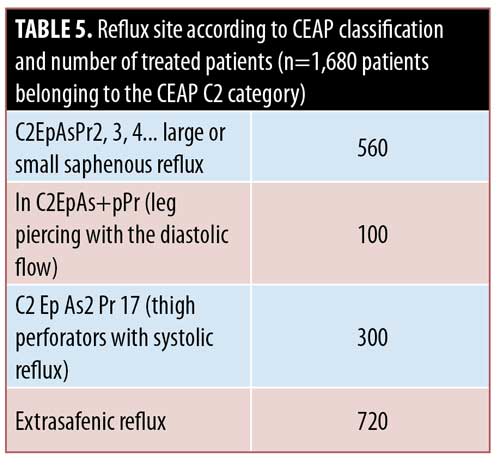
The treatments indicated for category C2 patients in the CEAP classification include tumescent thermal treatments, endoluminal ablation with laser2–4 or radiofrequency,4–8 hemodynamic treatments with the CHIVA4o method, and sclerotherapy.8–10 In our study, 1,680 patients were classified as C2.
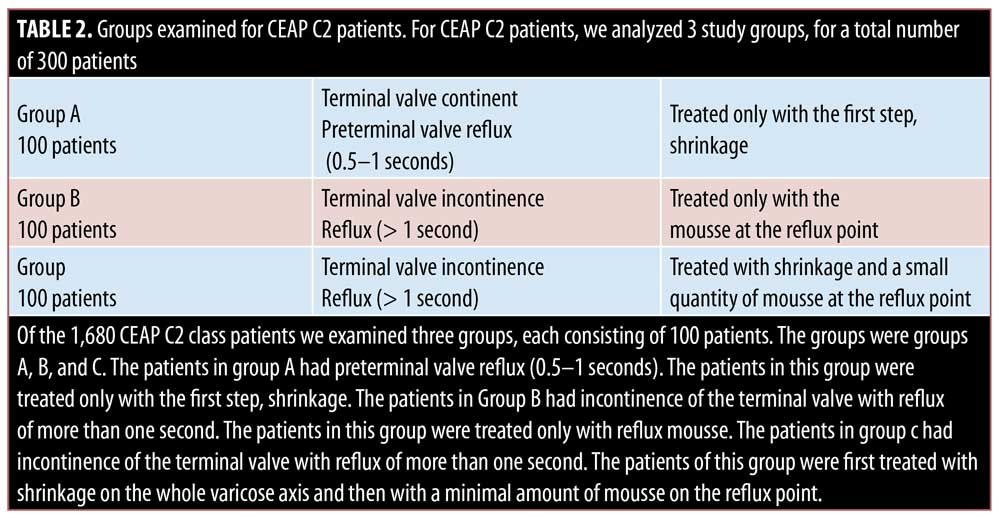
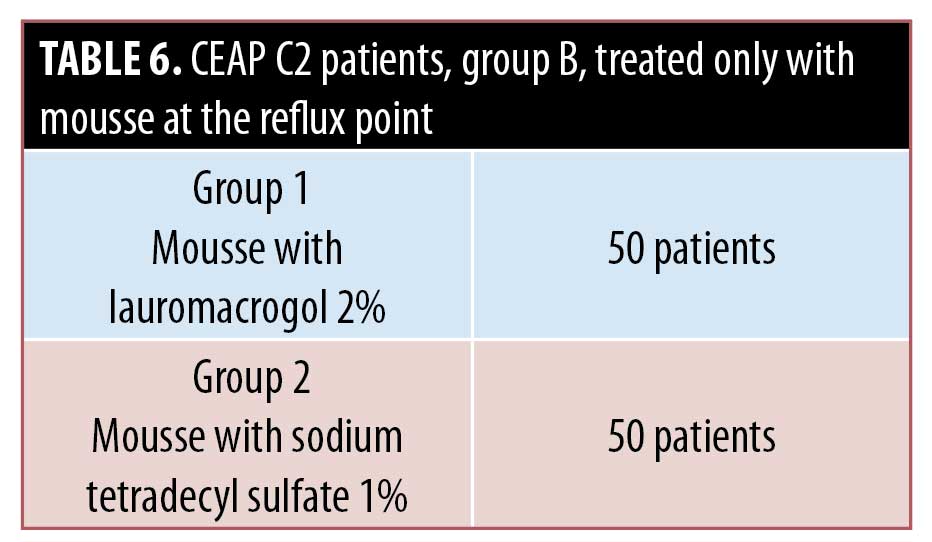
The C2 patients (N=1,680) were divided into three groups. Group A comprised patients with continent terminal valve and preterminal valve reflux. These patients were treated only with shrinkage. Group B comprised patients with incontinent terminal valve with reflux and were treated only with scleromousse at the reflux point. Group C comprised patients with incontinent valve who were treated first with shrinkage (Step 1) and then with a small amount of scleromousse at the reflux point.
An average number of three sessions of the Triplex method was performed on each patient. Follow-up assessments were performed using morphofunctional evaluation, histological examination, and photographic documentation after one, three, six, and 12 months, and once a year after treatment completion.
This study was carried out in compliance with the most up-to-date version of the Helsinki Declaration and was approved by an ethical committee in accordance with the International Council for Harmonization of Technical Requirements for Pharmaceuticals for Human Use ICH Good Clinical Practice regulations. The present study was submitted to the Ethic, Scientific and Medical Committee of International Radio Medical Center Foundation (C.I.R.M.) that approved it (Approval No. 01/2016 of January 31, 2016). In order to participate in the trial, each patient had to sign an informed consent form.
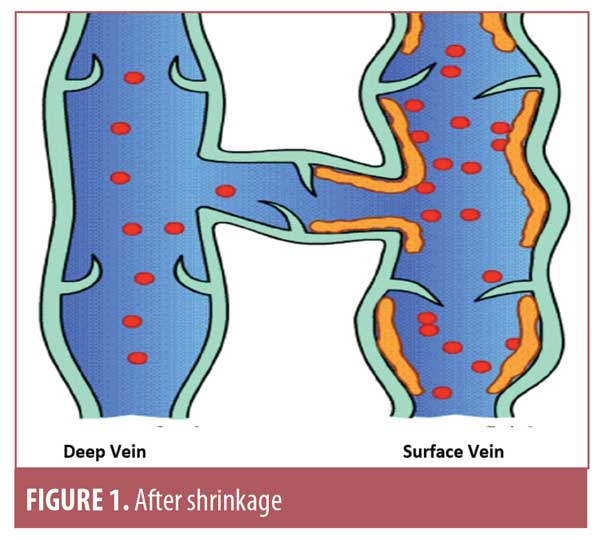
The Triplex approach starts with injections of a shrinkage solution, and, if insufficient narrowing occurs, is completed with ultrasonography-guided foam injection in the reflux points. The first step in the Triplex method entails narrowing the entire wall of varicose veins. Subsequently, there should be a decrease in the caliber of vessels, which is observable using Doppler ultrasonography or a histological examination, reducing or eliminating telangiectasias associated with the insufficiency of the saphenous tributaries.
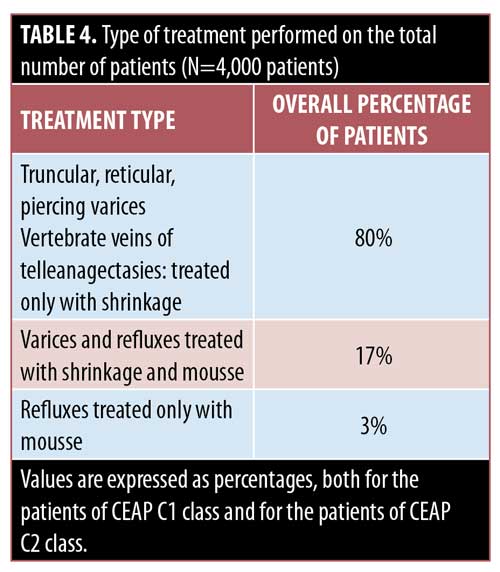
Step I: Shrinkage. In a 10mL syringe, 3.2mL of 12% sodium salicylate and 1mL of 2% lidocaine are combined, and brought to 10mL with physiological solution with 10% glycerol. In the case of an allergy to lidocaine, the administration is avoided. Generally, the solution is administrated slowly. To achieve an occlusion of small and medium vessels, sodium salicylate must have a concentration of 20 percent, while, for telangiectasias, a concentration of 8 to 10 percent is warranted. The physiological solution with glycerol increases the contact time with the varicose wall. Needles ranging from 27 gauge (.42mm) and 30 gauge (.16mm) are used. Each session includes a dose ranging between 11 to 33mL, depending on the extent of the vascular disorder. The treatment should be performed weekly, with an average of three sessions per limb. In our study, one treatment per week was performed for each limb for a total of three weeks. In six years, 4,000 patients were given this treatment, of which 2,320 were in CEAP class C1 and 1,680 were in class C2.
The preliminary procedure involves a morphofunctional Doppler ultrasonography examination that can be performed with assistance from a transilluminator—this allows identification of the saphenous path, evaluation of crosses and refluxes, the varicose path, perforations with reflux, return punches, areas with capillaries, and nourishing veins. Only the varicose veins, the perforating veins at the level of the foot, the insufficient tributaries of the saphenous, the reticular varices, and the nourishing veins of the telangiectasia are treated.
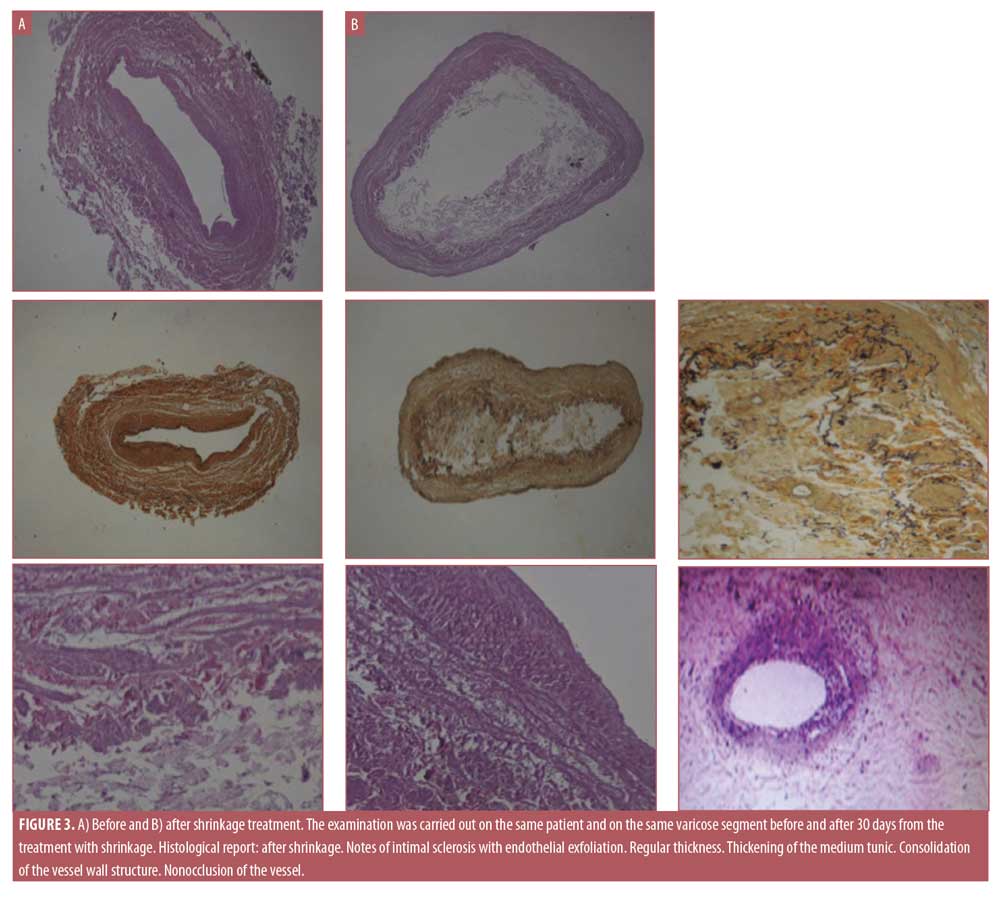
The injection of the shrinkage solution in the varices triggers an inflammatory process affecting the tunica intima, causing exfoliation of the endothelium. This results in nonocclusive fibrosis, with a thickening of the tunica media and consequent reduction of the vessel lumen. Consequently, the treated varices are pervaded and are no longer visible. With this first step, many telangiectasia and telangiectatic spots disappear without sclerotization. If the first step successfully narrows the affected veins, the patient does not need to undergo Step 2 and goes directly to the third step. Among the 1,680 CEAP C2 class patients, 1,200 did not undergo Step 2. Only 480 CEAP C2 patients underwent the second step.
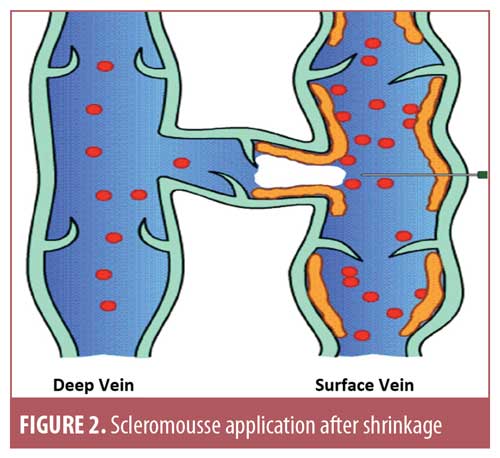
Step II: Ultrasound-guided foam sclerotherapy, or scleromousse. This step is performed when the targeted vessels are not sufficienty narrowed in Step 1. The foam, or mousse, is prepared with a three-way tap and two syringes containing a ratio of 1mL of 1% sodium tetradecyl sulfate (STS) and 4mL of air. Scleromousse is echoguided using a needle or catheter to treat only the reflux point and not the whole varicose vein. The scleromousse is removed 15 days after the second session. Only the reflux at the origin was treated in was treated in 20 patients belonging to the CEAP C2EpAs+pPr category.
Step III: Sclerosis of residual telangiectasia. Usually, low concentrations of STS 0.2% to 0.50% or lauromacrogol 0.25% were administered to the patients. This step is performed if telangiectasias remain after Step 1 and Step 2. Post-treatment compression using elastic stockings of a first or second class (first class compression grade: 18–21mmHg; second class compression grade: 22–32mmHg) was used. Patients in CEAP C1 group achieved stable results in narrowing of the affected veins.
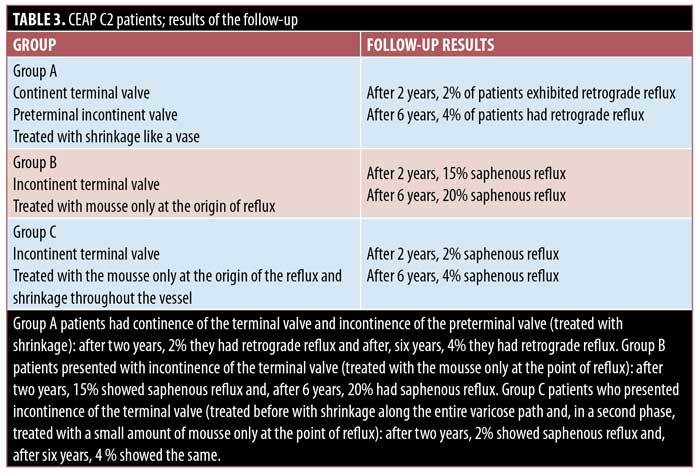
In a sample of 300 patients classified as CEAP C2, we analyzed cross-negative incidence in three groups (Table 1, section B). Group A (n=100) had mild reflux of the preterminal valve (retrograde reflux in the saphenous vein 0.5–1 second) and were treated only with the Step 1. After two years, 98 percent of these patients were reflux-free, and two percent of patients showed retrograde reflux in the saphenous vein. After six years, only four percent of these patients presented retrograde saphenous flow. These patients underwent Step 1 again.
Group B contained 100 patients with incontinence of the terminal valve (>1 second) who were treated only with the scleromousse (upper one-third of the thigh), saving the rest of the varicose vessel. After two years, only 15 percent of patients had reflux, with the presence of varices that were evident before treatment. In these patients, we proceeded with the first step along the varicose path and applied scleromousse to the upper one-third of the thigh , which resulted in resolution. After six years, only about 20 percent of the patients presented with hemodynamically significant reflux and evidences of viscosity. They were administered Step 1 along the entire varicose path and then Step 2, which was applied to the origin of the reflux.
In Group C, 100 patients with incontinence of the terminal valve (>1 second) were treated with Steps 1 and 2 immediately. After two years, only two percent of the patients had reflux, which was not hemodynamically significant. After six years, four percent of the patients presented with reflux that was hemodynamically significant. These patients were only administered the first step again.
No significant differences were observed egarding the use of lauromacrogol or STS in Step 3. No adverse effects were reported concerning the solution of sodium salicylate and lidocaine in a physiological solution with 10% glycerol, which was used to shrink vessels in Step 1.
Conclusion
The Triplex method effectively achieves vessel narrowing, attaining restoration of the functionality of the superficial venous system and saving the venous heritage. During the six-year follow-up, we observed 1) greater duration of the narrowing of the vessel’s caliber, 2) reduction in the amount of scleromousse required to treat the reflux point, 3) insignificant incidence of hemodynamic reflux in cases of recanalization in which we administered Steps 1 and 2.
References
1. Porter JM, Coin GL. Reporting standards in venous disease: an update. International Consensus Committee on Chronic Venous Disease. J Vasc Surg. 1995;21(4):635–645.
2. Christenson JT, Gueddi S, Gemayel G, Bounameaux H. Prospective randomized trial comparing endovenous laser ablation and surgery for treatment of primarygreatsaphenous varicose veins with a two-year follow-up. J Vasc Surg. J Vasc Surg. 2010;52(5):1234–1241.
3. Janne d’Othée B, Walker TG, Kalva SP, et al. Endovenous laser ablation of the small saphenousveinsparing the saphenopoplitealjunction. Cardiovasc Intervent Radiol. 2010; 33(4):766-771.
4. Mordon SR, Wassmer B, Zemmouri J. Mathematical modeling of 980-nm and 1320-nm endovenous laser treatment. Lasers Surg Med. 2007;39(3):256-265.
5. Luebke T, Brunkwall J. Systematic review and metanalysis of endovenous radiofrequency obliteration, endo-venous laser therapy, and foamsclerotherapy for primaryvaricosis. J Cardiovasc Surg (Torino). 2008;49(2):2013–2033.
6. Fan CM, Rox-Anderson R. Endovenous laser ablation: mechanism of action. Phlebology. 2008;23(5):206–213.
7. Cavallini A. [Combined phlebological treatments in the varices of the lower limbs associated with pelvic shunts and segmental saphenous incompetence]. Presented at the XXIX National Congress of the Italian Society of Phlebology; October 13–15, 2016; Pisa, Italy.
8. Proebstle TM, Alm J, Göckeritz O, et al. Three-year European follow-up of endovenous radiofrequency-powered segmental thermal ablation of the great saphenous vein with or without treatment of calfvaricosities. J Vasc Surg. 2011; 54(1):146–152.
9. Genovese. “Conservative hemodynamic sclerosis (E.S.E.C.) of large truncularverices” su International Angiology (Official Journal of the International Union of Angiology – 14th World Congress Union Internationale de Phlebologie – Roma 2001.
10. Cavezzi A, Frullini A Experencia de 3 anos con la espuma esclerosante en le escleroterapia eco-guiada de las venas safenas y de las varices recidivas. Flebologia Atlas Anatomico. 2007. 31–34.