Dear Editor:
Hemangioma is a common term to describe a benign proliferative lesion of vascular tissue origin that can be present either at birth or appear during childhood.1 Hemangiomas are developmental vascular abnormalities characterized by a proliferative growth phase and a very slow, inevitable regression (involutive phase). They are histologically classified into capillary and cavernous forms.2 Capillary hemangiomas are composed of many small capillaries lined by a single layer of endothelial cells supported in a connective tissue stroma of varying densities, while cavernous hemangiomas are formed by large, thin-walled vessels or sinusoids lined by epithelial cells and separated by a thin layer of connective tissue septa.2 In cases of hemangiomatous lesions, even partial manipulation of the lesion can cause significant bleeding.
Cryotherapy, also known as cryosurgery, is a treatment modality involving the destruction of tissue by the application of extremely low temperatures. This causes rapid tissue destruction though irreversible damage to the cellular metabolism and can be beneficial when used in diseased tissues. Cryotherapy provides many advantages, including easy operation, the absence of intraoperative bleeding, and a low infection rate.3
Here, we report the case of a patient with a hemangiomatous lesion over the face who was treated with a combination of cryotherapy, lasers, and dermatosurgery, with successful results apparent at 12 months of follow up.
Case report. A 60-year-old man presented with red-colored lesions located over the left side of his face that had been present since birth. Due to an increased chance of excessive bleeding, surgery had not been recommended to him at birth. Over time, these lesions had slowly extended to the scalp, supraorbital ridge, eyelid, nasal bridge, upper and lower lips, cheek, and chin on the left side of the face (Figure 1). The patient reported a gradual loss of vision in the left eye from birth. A substantial psychological impact was present that often resulted in foregoing attendance to social gatherings. Past medical, dental, and family histories were noncontributory and, during physical examination, he appeared to be healthy, with all vital signs within standard limits. Following the examination of the lesion, it was revealed that he had an erythematous, highly vascular plaque with irregular nodularity extending from the left scalp to the chin, which caused distorted facial features, obstruction of the left eye, and difficulty in opening the mouth. Hematological testing reported all findings were within standard limits and a routine urine examination was unremarkable. A provisional diagnosis of cavernous hemangioma was made based on its clinical appearance and growth. Based on the findings, a combination of cryotherapy, laser, and dermatosurgery was planned in the following order: cryotherapy, debulking with the UltaPulse® CO? laser (Lumenis Ltd., Yokneam, Israel), surgical excision, and fractional CO? laser treatment.

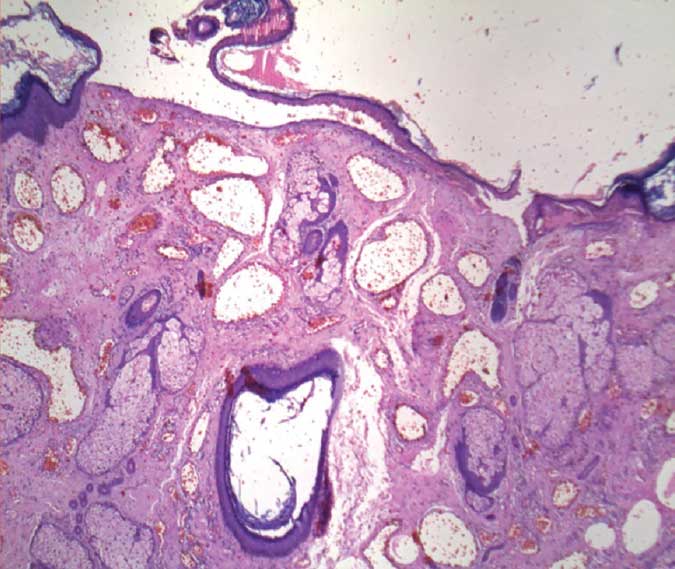
First, the lesion was treated with cryotherapy using liquid nitrogen to make the tissue less vascular. Here, we used our own modified cryoapplicator for convenience. For this, we prepared a cotton ball with four-inch dimensions and dipped it into liquid nitrogen, then applied it to the lesions using forceps for 3 to 5 minutes. After, the frozen lesion was removed using a 10,600-nm CO? laser with aggressive parameters (continuous and a coagulation mode, 30 watts). The excised growth was transferred to histopathology examination (Figure 2) and indicated the definite diagnosis of a cavernous hemangioma (Figure 3). Next, a full-thickness skin graft using a general anesthesia was applied (Figures 4A and 4B). The graft was rejected during the first week after surgery due to excessive tissue necrosis and decreased vascularity, so another procedure for a thin-skin graft was planned after another week. Surgery was conducted three times due to poor wound healing. Finally, the face was treated with fractional CO? laser (10,600nm) once a month for six months to improve the texture and tone of the skin after involution. For the fractional CO? laser, the pulse duration, beam diameter, and laser energy were 500?m, 150?m, and 60mJ, respectively. The patient received a total of six sessions. Satisfactory healing was reported five months later (Figure 5). At the patient’s 12-month follow up, he was observed for any reccurrence of a similar lesion (Figure 6). To date, there are no reports of postoperative infection, difficulty breathing, or allergic reactions following cryosurgery using liquid nitrogen. Our patient reported mild pain, which was managed with peripherally acting analgesics.





Hemangiomas are considered to be benign tumors of the vascular endothelium, but are able to cause serious injuries, functional impairment, and life-threatening complications. Any type of tumor, whether benign or malignant, requires early detection and diagnosis to avoid later complications. This case report demonstrated the successful removal of a facial hemangioma using a combined treatment approach involving cryotherapy, laser therapy, and dermatosurgery, with no lesion recurrence after treatment. Additionally, the patient was relieved from his breathing and swallowing difficulties and experienced an improvement in his appearance and quality of life.
With regard,
Jagdish Sakhiya, MD; Dhruv Sakhiya J, MBBS; Neha Virmani, MD, DNB; Arvind Patel, MS, MCh; Feral Daruwala, mPharm; and Nimish Dudhatra, MSc, CR
Affiliations. Drs. J. Sakhiya, Virmani, and Patel and Daruwala and Dudhatra are with Sakhiya Skin Clinic Pvt. Ltd. in Surat, India. Dr. D. Sakhiya is with the B.J. Medical College at New Civil Hospital Asarwa in Gujarat, India.
Funding. No funding was provided.
Disclosures. The authors have no conflicts of interest relevant to the content of this article.
Correspondence. Feral Daruwala, M.Pharm; Email: feral.modi@gmail.com
References
- Purkait SK. Essentials of Oral Pathology. 3rd ed. New Delhi, India: Jaypee Brothers Medical Publishers Pvt. Ltd.; 2011:120–121.
- KA Kamala, L Ashok, GP Sujatha. Cavernous hemangioma of the tongue: A rare case report. Contemp Clin Dent. 2014; 5(1): 95–98.
- Nogueira et al. Cryosurgery as an option for the treatment of vascularlesions of the oral cavity. Case Rep Otolaryngol. 2017;8529016.

