J Clin Aesthet Dermatol. 2025;18(9–10 Suppl 1):S10–S11.
by Mahnoor Mukarram, DO, MS; Zaina Rashid, DO, FAAD; and Sarah Shuker, PA-C
Dr. Mukarram is with Abrazo Health Network in Goodyear, Arizona. Dr. Rashid and Ms. Shuker are with La Peau Dermatology in Mesa, Arizona.
Funding: No funding was provided for this article.
Disclosures: The authors report no conflicts of interest relevant to the contents of this article.
Abstract: Squamous cell carcinoma (SCC) is the second most common type of skin cancer following basal cell carcinoma (BCC). Risk factors for the development of SCC include exposure to ultraviolet light (UV) and non-UV-related risk factors, such as chronic wounds, Marjolin ulcers, and human papillomavirus (HPV) infection. In this case report, we report an interesting case of the development of SCC in the palm of a patient with an extensive history of Lyme disease. Keywords: Squamous cell carcinoma, palmar SCC, cutaneous malignancy, Lyme disease
Introduction
Squamous cell carcinoma (SCC) is the second most common type of nonmelanoma skin cancer, accounting for approximately 20 percent of all skin malignancies.1 The presence of SCC on the hand is often linked to environmental exposures, immunosuppression, or genetic syndromes.2 Additionally, non-UV-related risk factors, such as chronic wounds, Marjolin ulcers, and human papillomavirus (HPV) infection, have been implicated in its pathogenesis.2 While SCC can develop anywhere on the body, it predominantly affects sun-exposed areas, such as the face, neck, and dorsal surfaces of the hands.
Among SCC cases of the upper extremities, SCC of the palm is rare. Unlike the dorsal aspect of the hand, which is frequently exposed to UV radiation, the palm has a thick stratum corneum and lacks direct sun exposure, making SCC in this location unusual. When SCC does arise on the palm, it is often associated with nontraditional risk factors, such as chronic inflammation, previous trauma, scarring, arsenic exposure, or immunosuppression.3 Due to its rarity, SCC of the palm is at risk for delayed diagnosis and misidentification, potentially leading to more aggressive progression and poorer outcomes. In this case report, we present an unusual case of SCC of the palm, highlighting its clinical presentation and diagnostic challenges.
Case Presentation
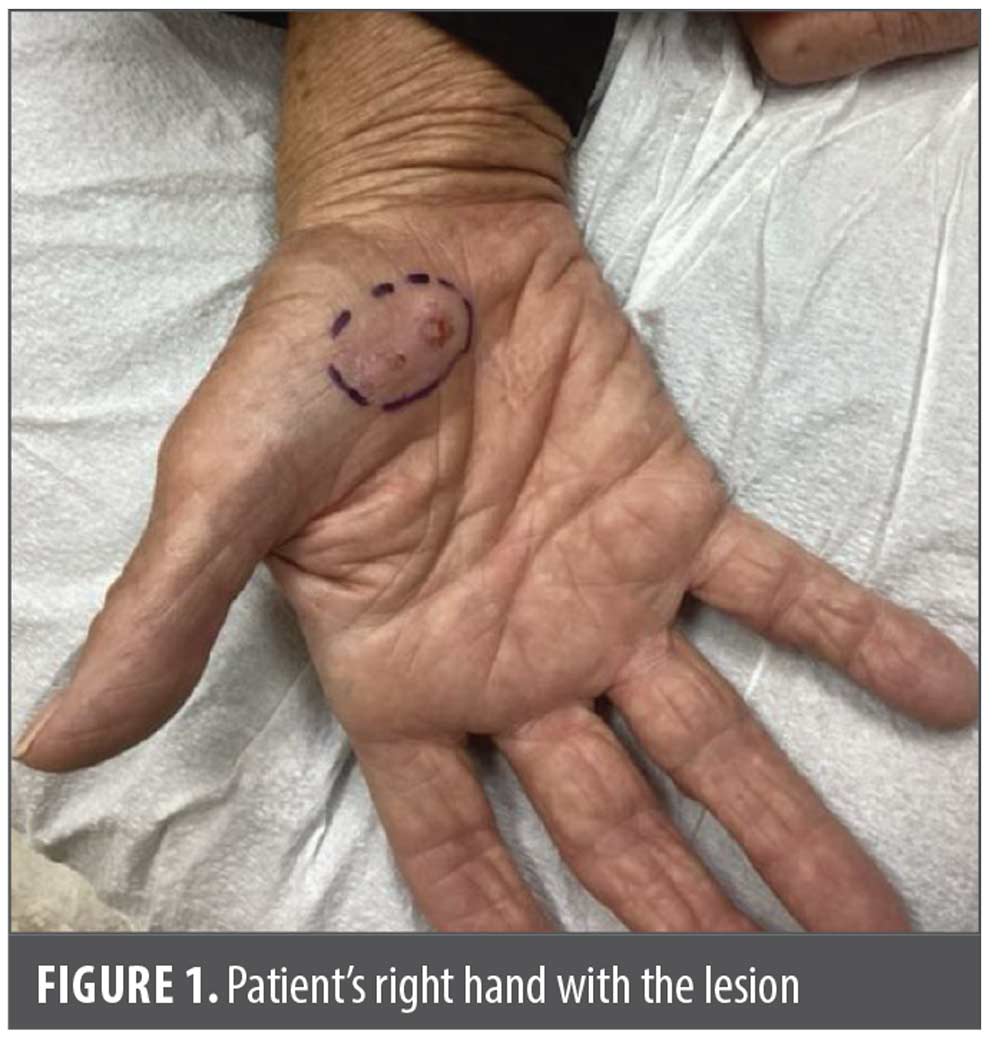
A 73-year-old female patient with a greater than 10-year history of Lyme disease presented in September 2023 due to the sudden onset of a large erythematous nodule on her right palm (Figure 1). The patient had no prior history of burns, trauma, or skin cancer. However, the patient stated an extensive history of tanning bed use, undergoing tanning sessions monthly. The patient was also taking multiple naturopathic medications prescribed by her naturopath to treat her Lyme disease. Upon exam, one large 2.6×2.1cm erythematous nodule was present on her right palm. Biopsy was performed during her visit and demonstrated well-differentiated SCC. She was immediately referred to a hand surgeon due to concern of the lesion involving muscle and tendon. She was scheduled for surgery at the end of March.
Discussion
SCC of the hand, though less common than facial or scalp lesions, presents unique clinical challenges due to the functional importance of the affected area and the potential for delayed diagnosis. Given its potential for delayed diagnosis and functional impact, early detection and targeted intervention are crucial for optimal outcomes in palmar SCC.
There is scarce literature documenting the presence of SCC on the palm of the hand. One report by Valk et al4 discusses a case of SCC, specifically a verrucous carcinoma, a well-differentiated, wart-like form of SCC, that occurred on the palm of a 53-year-old male patient. This patient’s cancer spread extensively through the joints, muscles, and ligaments, necessitating a complete recession involving removing the entire finger along with its metacarpal. González-Sosa et al5 also reported on a male patient who presented with SCC on his left palm and clinically positive axillary lymphadenopathy. This patient had been incorrectly diagnosed prior to his definitive diagnosis of palmar SCC.5 Although palmar SCC is rarely reported, the available cases reveal the potential of aggressive local spread that necessitates radical surgical resection and might be prone to initial misdiagnosis.6 Additionally, metastases from palmar SCC can result in other complications, including small bowel obstruction.7 Although highly unusual, such occurrences have been reported and must be taken into consideration.
Interestingly, a case documenting the presence of SCC on both palms in a 70-year-old patient was reported.8 Lesions emerged concurrently on both palms, and no direct cause was identified. Notably, the patient was exposed to battery acid at work. Histological analysis confirmed the presence of SCC on both palms. Due to the disease’s unfavorable progression, a subsequent surgery was performed to remove a metastatic tumor in the left axilla that involved the brachial plexus.8 Similarly, SCC of the palm after chronic organophosphate exposure was documented in an elderly man who, over a two-year period, regularly handled chemicals with his bare hands.9 Another article discussed multiple pigmented SCC in situ on the palmar hands after chronic use of topical tacrolimus in a 55-year-old man with skin of color.10 Such incidences of SCC represent the potential role of certain chemicals and substances in the development of cutaneous malignancies.
As our patient had an extensive history of Lyme disease, another area of interest is the potential link between Lyme disease and SCC, particularly through its late-stage cutaneous manifestation, acrodermatitis chronica atrophicans (ACA). ACA, caused by chronic Borrelia burgdorferi infection, results in progressive skin atrophy, fibrosis, and dermal inflammation, primarily affecting the hands and feet.11 Studies have suggested that chronic inflammatory conditions and repeated tissue damage can create a microenvironment conducive to malignant transformation, thereby increasing the risk of SCC.2 Although a direct causal relationship between Lyme disease and SCC has not been firmly established, cases of SCC arising in ACA-affected skin have been reported, indicating the need for further research on this potential association. Given that ACA primarily occurs in Europe, this link might be underrecognized in North American populations.
Due to its rarity and atypical presentation, SCC of the palm is often misdiagnosed as a benign lesion, such as a wart, callus, chronic ulcer, or fungal infection, leading to delayed treatment. Unlike SCC in UV-exposed regions, palmar SCC can exhibit more aggressive behavior, with a higher risk of spreading to the lymph nodes. Furthermore, histological variants, such as verrucous carcinoma, desmoplastic SCC, and keratoacanthoma-type SCC, can further complicate diagnosis. Molecular differences between SCC in sun-exposed and non-sun-exposed areas suggest that tumors arising from chronic inflammation or chemical exposure might have distinct genetic alterations, differentiating them from UV-driven SCC.12
Given the functional importance of the palm, SCC in this location presents surgical challenges, requiring consideration between complete tumor excision (via wide local excision or Mohs micrographic surgery) and preserving hand function. In cases of high-risk SCC, such as in patients with poor differentiation, perineural invasion, or a tumor depth greater than 2mm, a sentinel lymph node biopsy (SLNB) might be warranted to assess metastatic potential.13 Additionally, adjuvant therapy, including radiation or systemic immune checkpoint inhibitors, can be considered for aggressive or recurrent cases.14 For patients with locally advanced or metastatic SCC, systemic therapies such as immune checkpoint inhibitors have shown promising results, particularly in immunosuppressed individuals or those with recurrent disease.14 Overall, managing SCC on the palm requires a careful balance between complete tumor removal and maintaining limb function, often incorporating additional diagnostic and systemic therapies for high-risk or advanced cases.
Conclusion
SCC of the palm is a rare but potentially aggressive malignancy that requires heightened clinical awareness for early detection and intervention. Unlike UV-associated SCC, palmar SCC is more commonly linked to chronic irritation, scarring, occupational exposures, and possibly chronic inflammatory conditions such as ACA (a late manifestation of Lyme disease). Due to its unusual location, SCC of the palm is often misdiagnosed, leading to delays in treatment and a higher risk of invasive disease. Early clinical intervention and multidisciplinary management are essential to optimize patient outcomes. Further research into non-UV-related SCC pathogenesis, including the potential link between Lyme disease and SCC, might provide new insights into risk stratification and targeted therapies. Moreover, recognizing non-UV-related risk factors, ensuring early biopsy, and tailoring surgical and systemic treatment strategies are essential to improving patient outcomes.
References
- Fania L, Didona D, Di Pietro FR, et al. Cutaneous squamous cell carcinoma: from pathophysiology to novel therapeutic approaches. Biomedicines. 2021;9(2):171.
- Hadian Y, Howell JY, Ramsey ML, et al. Cutaneous squamous cell carcinoma. Updated 2 Jul 2024. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441939/
- Hsu LI, Chen GS, Lee CH, et al. Use of arsenic-induced palmoplantar hyperkeratosis and skin cancers to predict risk of subsequent internal malignancy. Am J Epidemiol. 2013;177(3):202–212.
- Valk J, Valk B, Caid M, et al. Ray resection for recurrent invasive squamous cell carcinoma: a case report. Spartan Med Res J. 2020;5(2):14612.
- González-Sosa D, Brea-García B, Couto-González I, et al. Moderately differentiated squamous cell carcinoma of the palm: an extremely infrequent tumour. BMJ Case Rep. 2014;2014:bcr2014206350.
- Sayed L, Deodhar AK, Agarwal R. A single centre experience of squamous cell carcinoma of the upper limb requiring digital or hand amputation and review of literature. JPRAS Open. 2019;20:43–58.
- Li R, Chen, Z, Wen Q, et al. Metastatic squamous cell carcinoma from hand skin causing small bowel obstruction: an unusual case presentation. World J Surg Onc. 2014;12:166.
- Watier E, Georgieu N, Chevrier S, et al. Squamous cell carcinoma on both palms. E J Plastic Surg. 2000;23:338–340.
- Pezas T, Cogswell L. Squamous cell carcinoma of the palm after chronic organophosphate exposure. Br J Hosp Med (Lond). 2018;79(9):530-531.
- Konisky H, Kortz A, Huho A, Gregory AN. Multiple pigmented squamous cell carcinoma in situ on the volar hands after chronic use of topical tacrolimus. JAAD Case Rep. 2024;52:66–67.
- Gade A, Matin T, Rubenstein R, et al. Acrodermatitis chronica atrophicans. Updated 2 Jan 2023. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/sites/books/NBK563289
- Lazar AD, Dinescu S, Costache M. Deciphering the molecular landscape of cutaneous squamous cell carcinoma for better diagnosis and treatment. J Clin Med. 2020;9(7):2228.
- Fox M, Brown M, Golda N, et al. Nodal staging of high-risk cutaneous squamous cell carcinoma. J Am Acad Dermatol. 2019;81(2):548–557.
- Koch Hein EC, Vilbert M, Hirsch I. Immune checkpoint inhibitors in advanced cutaneous squamous cell carcinoma: real-world experience from a Canadian comprehensive cancer centre. Cancers (Basel). 2023;15(17):4312.