J Clin Aesthet Dermatol. 2025;18(8):30–33.
by Hana I. Nazir, MD; Kathleen E. Daly, MSc; Elizabeth V. Seiverling, MD; Cristian Navarrete-Dechent, MD; and Kendall L. Buchanan, MD
Dr. Nazir, Ms. Daly, and Dr. Buchanan are with the Department of Dermatology at the Medical College of Georgia at Augusta University in Augusta, Georgia. Dr. Seiverling is with the Department of Dermatology at the University of Pittsburgh School of Medicine in Pittsburgh, Pennsylvania. Dr. Navarrete-Dechent is with the Department of Dermatology at the Escuela de Medicina, Pontificia Universidad Catolica de Chile in Santiago, Chile.
FUNDING: No funding was provided for this article.
DISCLOSURES: The authors declare no conflicts of interest relevant to the content of this article.
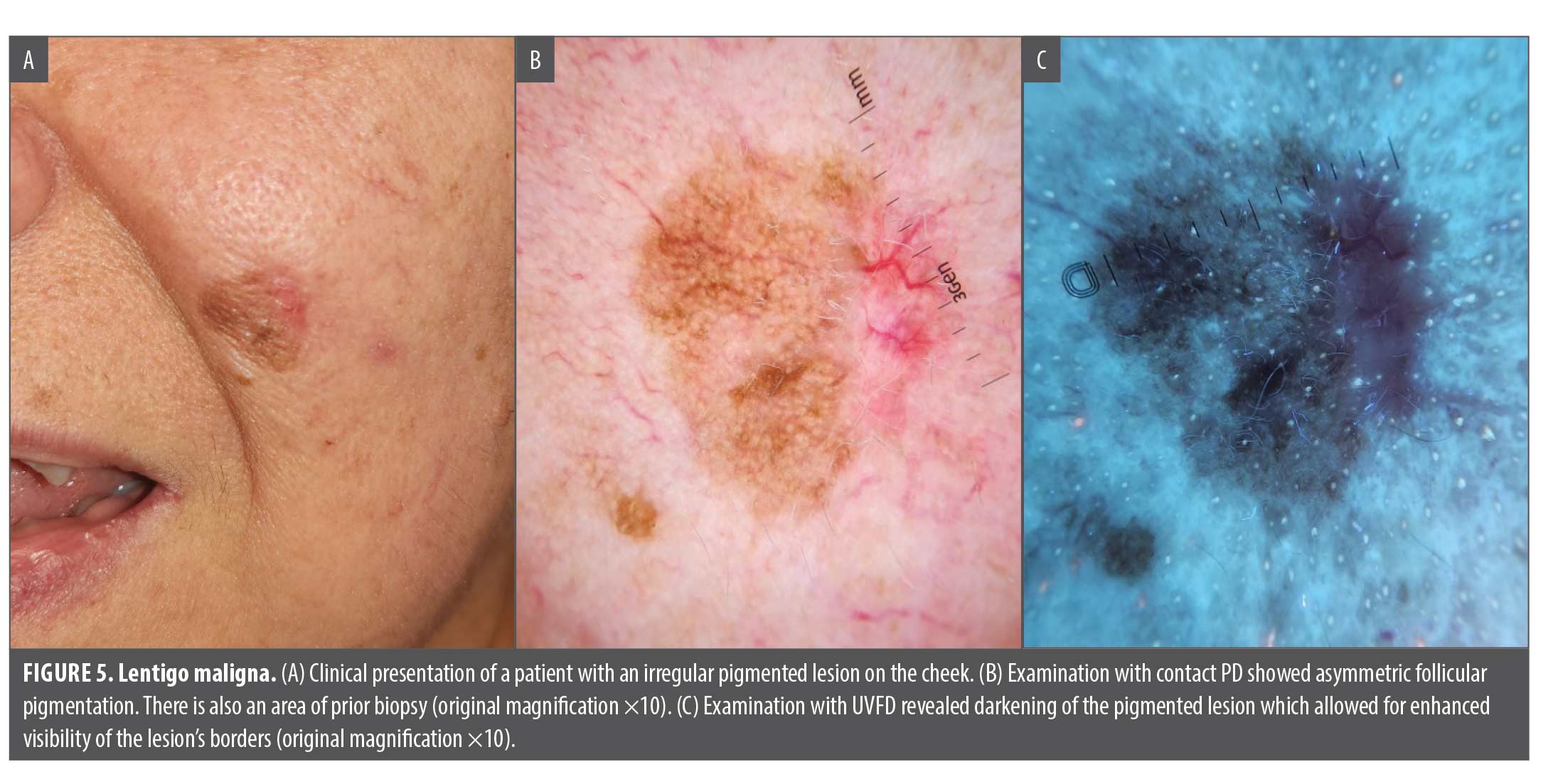
Abstract: Ultraviolet-induced fluorescence dermoscopy (UVFD) is a novel diagnostic and visualization technique that enhances visualization of skin dermatoses with ultraviolet (UV) light. UVFD has been used to diagnose dermatoses including bacterial and fungal infections, pigmentary disorders, and skin neoplasms. We present five cases—pitted keratolysis, porokeratosis, molluscum, biopsy site identification, and lentigo maligna—where UVFD alone, compared to traditional polarized dermoscopy (PD) or the unaided clinical exam, served as a “game-changer” in diagnosis and management. Polarized and UV images were captured using a DL5 dermatoscope coupled to a smartphone. In the cases of pitted keratolysis, porokeratosis, and molluscum, we highlight distinct patterns of fluorescence that were readily visualized with UVFD and aided efficient diagnosis, in contrast with more subtle features that were seen under PD. We also demonstrate the utility of UVFD in identification and confirmation of a prior biopsy site in a patient who presented for excision of a skin cancer. Finally, we describe the advantage of UVFD in presurgical margin delineation in a patient with lentigo maligna. In these cases, we show that UVFD facilitates prompt and accurate diagnosis, streamlines appropriate treatment, and has the capacity to reduce the need for unnecessary biopsies. Given the convenience and practicality of a dermatoscope equipped with a UV light, we propose that clinicians would benefit from the use of UVFD as a supplementary tool alongside conventional dermoscopy, rather than as a substitute. Keywords: Dermoscopy, ultraviolet-induced fluorescence dermoscopy, biopsy, skin cancer, diagnosis, surgery
Introduction
Ultraviolet-induced fluorescence dermoscopy (UVFD) is a novel diagnostic and visualization technique.1–13 Building upon the advantages of traditional polarized dermoscopy (PD), UVFD enhances visualization of skin dermatoses with ultraviolet (UV) light in a handheld, portable format. Similar to the conventional Wood’s lamp, which emits light at wavelengths ranging from 320 to 400nm, UVFD utilizes high-energy, short-wavelength light emitting diodes (peak wavelength 365nm, 10mW/cm2), to stimulate skin chromophores.1,2 The accumulated energy, eventually emitted as a photon in the visible light spectrum, is then detectable by the human eye due to the Stokes shift effect.1
The Wood’s lamp has long been used for diagnosis of several dermatoses, including bacterial and fungal infections, pigmentary disorders, and cutaneous porphyrias, as well as for identification of skin neoplasm margins.2 Thus, its integration with dermoscopy might prove an invaluable supplement to traditional dermoscopic evaluation. Recent literature elucidates the advantages of UVFD for diagnosing and monitoring scabies, vitiligo, alopecia, seborrheic keratoses, pityriasis versicolor, and melanoma.3–10
We present five cases where UVFD alone, compared to traditional PD or the unaided clinical exam, served as a “game-changer” in diagnosis and management. In these cases, a commercially available UVFD dermatoscope (DermLite DL5; DermLite, LLC) coupled to a smartphone was utilized to produce and capture the fluorescent images. All patients provided informed consent and photoconsent.
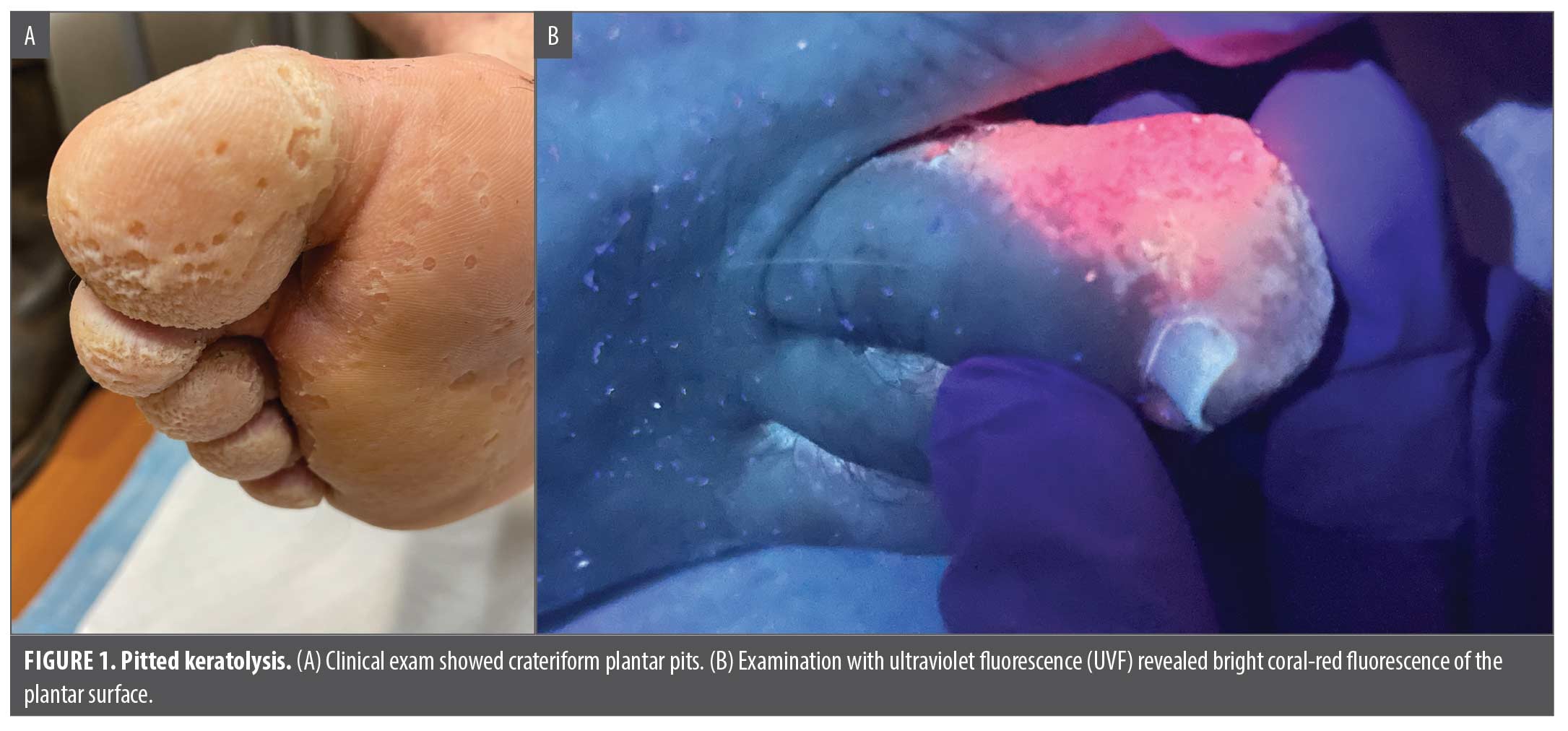
Pitted keratolysis. A 23-year-old male patient presented with concern regarding years of malodorous feet. He was previously treated with oral terbinafine without improvement. Physical examination revealed multiple punctate, crateriform pits on the right plantar foot and maceration in the interdigital spaces (Figure 1A). Ultraviolet fluorescence (UVF) revealed a coral-red color (Figure 1B), consistent with Corynebacterium spp. pitted keratolysis. In this case, the responsible fluorochrome is Coproporphyrin III, which appears as an orange-red color under UVF. As a result, he was properly diagnosed and treated with topical clindamycin gel and oral doxycycline.
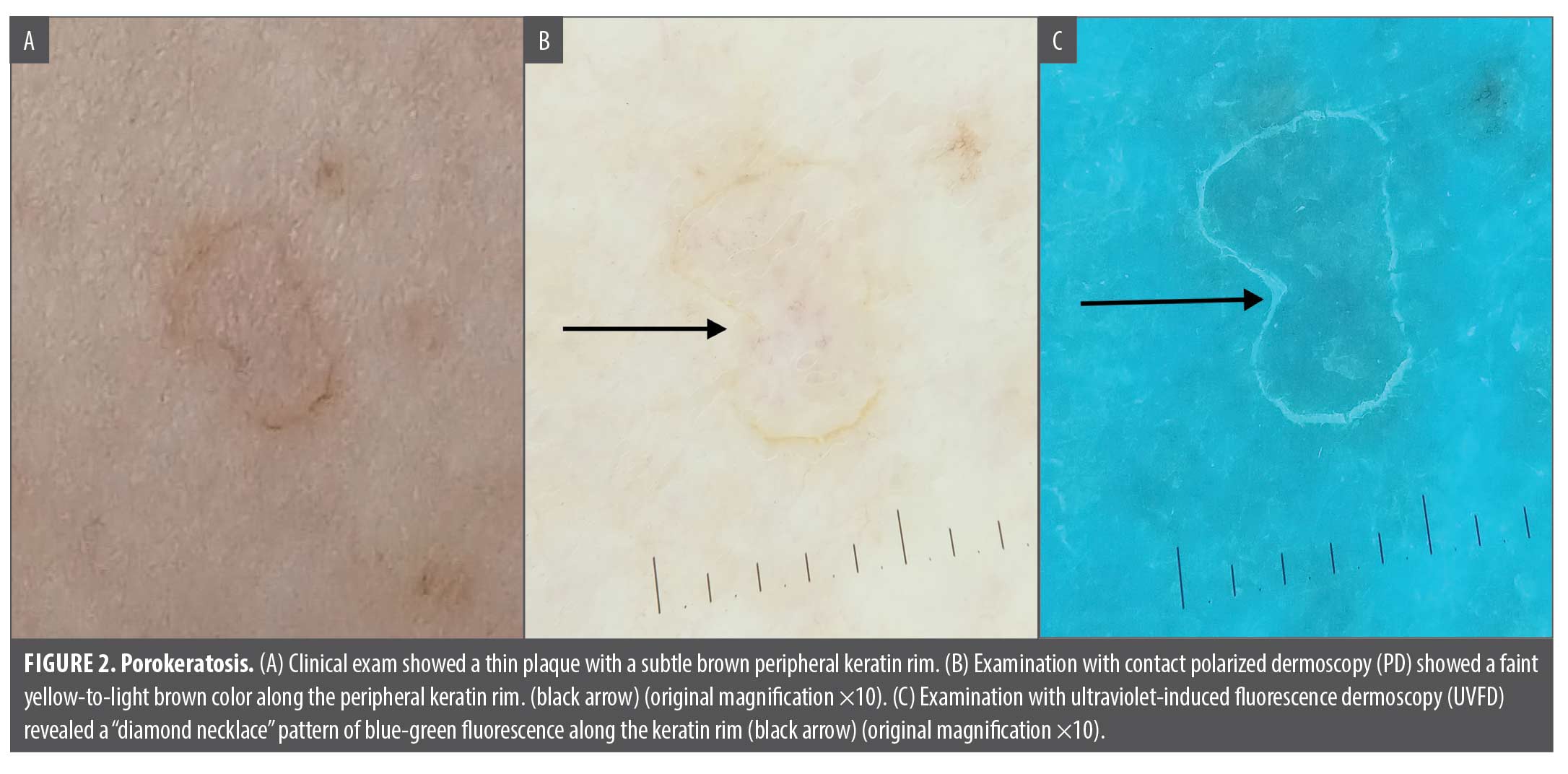
Porokeratosis. A 62-year-old female patient with history of basal cell carcinoma (BCC) and actinic damage presented to clinic for a full-body skin exam. A 0.5cm tan, scaly thin plaque on her right lateral thigh was seen (Figure 2A). PD showed a subtle yellow-to-light brown peripheral keratin rim (black arrow, Figure 2B) on an otherwise unremarkable image. Under UVFD, the keratin rim (coronoid lamella) showed a bright blue-green fluorescence (black arrow, Figure 2C), revealing a “diamond necklace” appearance.12,14 While an ink test would also enhance this feature, the use of UVFD minimizes the additional time and effort needed to confirm the diagnosis.
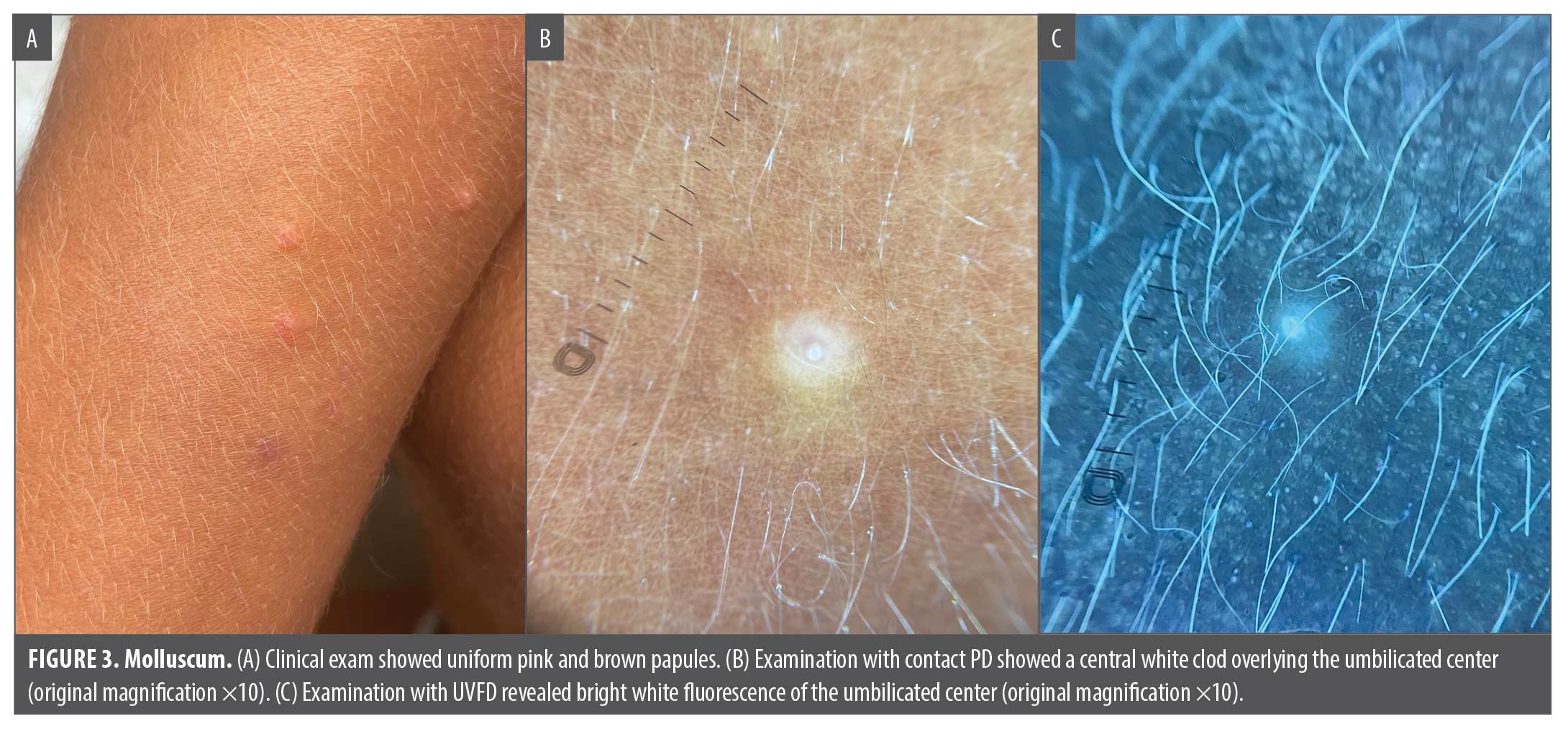
Molluscum. A 16-year-old male patient presented with several small, pink and brown monomorphous papules on the arms and legs (Figure 3A). PD showed a central white clod (keratotic papule) superimposed on a white-yellow homogeneous background (Figure 3B). While traditional PD did not readily display the characteristic central umbilication with polylobular yellow-to-white amorphous structures, or fine, branched vessels, UVFD strikingly highlighted the bright white umbilicated center (Figure 3C).9,15–18
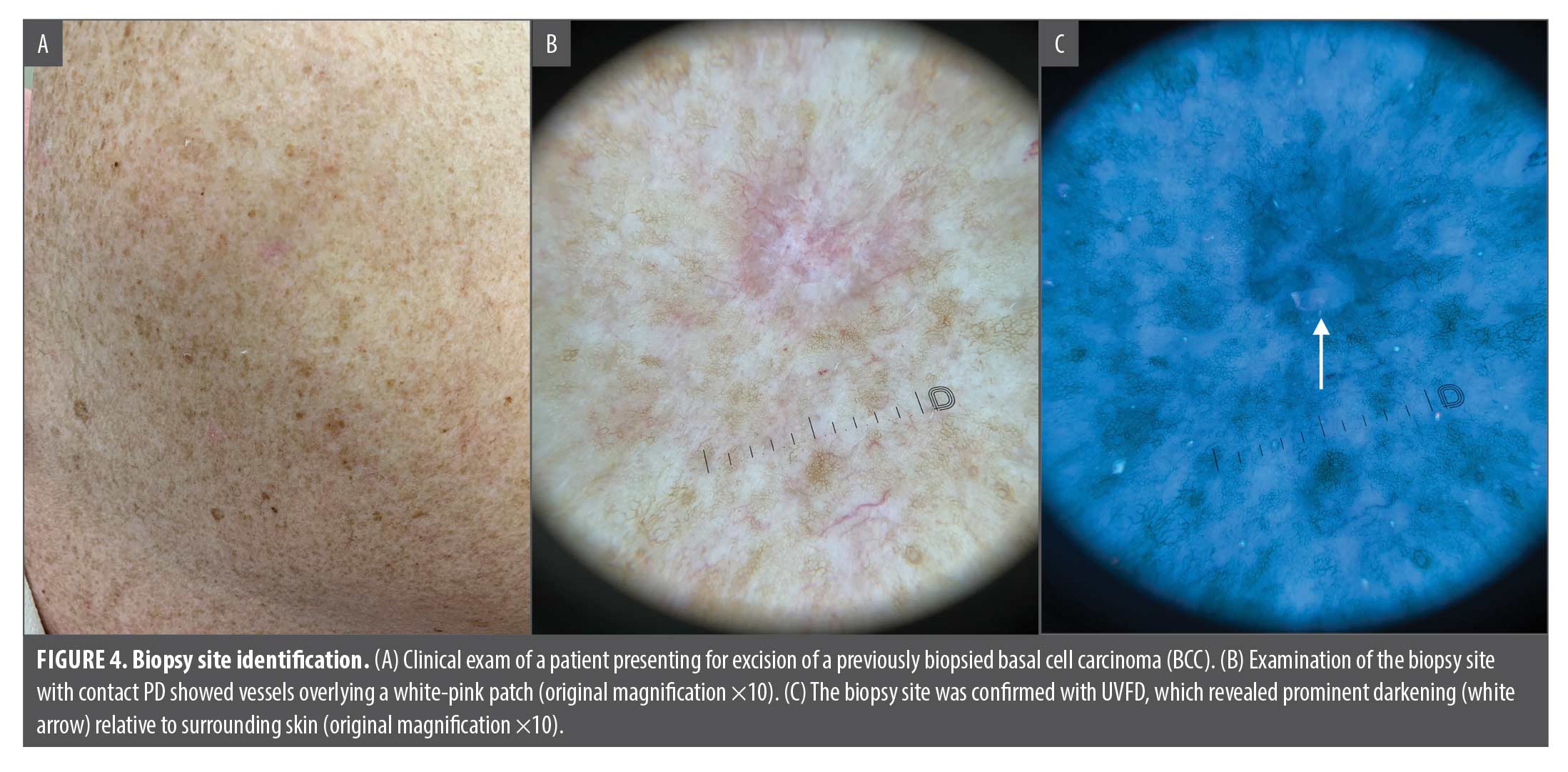
Biopsy site identification. A 68-year-old male patient presented for surgical excision of a previously biopsied BCC of his right scapular back (Figure 4A). Due to the unlabeled clinical photo, numerous lentigines, and unclear anatomic positioning for surgery, dermoscopy was utilized to confirm the biopsy site. While PD demonstrated a subtle white-pink background with overlying vessels (Figure 4B), UVFD revealed a prominent 0.8cm area of darkening compared to the patient’s surrounding skin, confirming the biopsy site (white arrow; Figure 4C). The enhanced darkening likely reflects post-biopsy scar tissue, as well as increased inflammation and hypervascularity.11
Lentigo maligna margin delineation. A 65-year-old female patient presented with an irregular pigmented patch measuring 1.3 x 1.4cm located on her left medial cheek (Figure 5A). PD showed asymmetric follicular pigmentation and arborizing vessels at the periphery that reflect scar tissue in the setting of a prior biopsy (as opposed to melanoma) (Figure 5B). UVFD revealed an overall darkening of the lesion with accentuation of the lesion borders (Figure 5C). This was signified by the contrast between the darker and light areas of absorption. As a result, UVFD served as a complement to the melanoma-specific features visualized under PD by increasing border visibility, thus allowing for better estimation of subclinical extension and presurgical margin delineation.
Discussion
The highlighted cases represent “game changers” where the use of UVFD demonstrated improved diagnostic capability over traditional PD or the unaided clinical exam. The addition of UVFD effectively and efficiently identifies diagnostic features that might be not visible when examined solely with conventional dermoscopy. Given the practicality of a dermatoscope equipped with a UV light, clinicians would benefit from the use of UVFD as a supplementary tool alongside conventional dermoscopy, rather than as a substitute. As in the aforementioned cases, there is minimal time and effort required for the incorporation of UVFD. UVFD facilitates prompt diagnosis, streamlines appropriate treatment, and has the capacity to reduce the need for unnecessary biopsies.
References
- Pietkiewicz P, Navarrete-Dechent C, Togawa Y, et al. Applications of Ultraviolet and Sub-ultraviolet Dermatoscopy in Neoplastic and Non-neoplastic Dermatoses: A Systematic Review. Dermatol Therapy. 2024;14(2):361–390.
- Dyer JM, Foy VM. Revealing The Unseen: A Review of Wood’s Lamp in Dermatology. J Clin Aesthet Dermatol. 2022;15(6):25–30.
- Pietkiewicz P, Navarette-Dechent C. Scabies mite is bright green under UV dermatoscopy. Dermatol Pract Concept. 2023;13(2):e2023135.
- Yürekli A. A new sign with UV dermoscope in the diagnosis of scabies: Ball sign. Skin Res Technol. 2023;29(5):e13336.
- Yürekli A, Muslu İ, Pektaş SD, et al. Using ultraviolet dermoscopy in diagnosing scabies. Exp Dermatol. 2023;32(11):1996–1999.
- Yuan M, Xie Y, Zheng Y, et al. Novel ultraviolet-dermoscopy: Early diagnosis and activity evaluation of vitiligo. Skin Res Technol. 2023; 29(1):e13249.
- Rodrigues-Barata AR, Moreno-Arrones OM, Corralo DS, Galvan SV. The “Starry Night Sky Sign” Using Ultraviolet-Light-Enhanced Trichoscopy: A New Sign That May Predict Efficacy of Treatment in Frontal Fibrosing Alopecia. Int J Trichology. 2018;10(5):241–243.
- Li X, Zhou C. Ultraviolet-induced fluorescence dermoscopy aids in distinguishing scarring and nonscarring alopecia. J Am Acad Dermatol. 2024;91(1):e1–e2.
- Kaliyadan F, Jayasree P, and Ashique KT. Ultraviolet reflectance dermoscopy. Indian J Dermatol Venereol Leprol. 2024. 90(6):838–841.
- Sano T, Minagawa A, Suzuki R, et al. Dermoscopy with near-ultraviolet light highlights the demarcation of melanin distribution in cutaneous melanoma. J Am Acad Dermatol. 2021;84(1):e23–e24.
- Navarrete-Dechent C, Pietkiewicz P, Dusza SW, et al. Ultraviolet-induced fluorescent dermoscopy for biopsy site identification prior to dermatologic surgery: A retrospective study. J Am Acad Dermatol. 2023;89(4):841–843.
- Chi C, Liu J. Image Gallery: Porokeratosis under the dermoscopic furrow ink test and ultraviolet light. Br J Dermatol. 2017;177(4):e159.
- Navarrete-Dechent C, Pietkiewicz P, Astronave G, et al. The role of ultraviolet-induced fluorescence dermatoscopy for the detection of multiple aggregated yellow-white globules in basal cell carcinoma. J Am Acad Dermatol. 2024;91(6):1250–1252.
- Pietkiewicz P, Korecka K, Salwowska N, et al. Porokeratoses-A Comprehensive Review on the Genetics and Metabolomics, Imaging Methods and Management of Common Clinical Variants. Metabolites. 2023;13(12):1176.
- Morales A, Puig S, Malvehy J, Zaballos P. Dermoscopy of Molluscum Contagiosum. Arch Dermatol. 2005;141(12):1644.
- Zaballos P, Ara M, Puig S, Malvehy J. Dermoscopy of molluscum contagiosum: a useful tool for clinical diagnosis in adulthood. J Eur Acad Dermatol Venereol. 2006;20(4):482–483.
- Ianhez M, Cestari Sda C, Enokihara MY, Seize MB. Dermoscopic patterns of molluscum contagiosum: a study of 211 lesions confirmed by histopathology. An Bras Dermatol. 2011;86(1):74–79.
- Ku SH, Cho EB, Park EJ, et al. Dermoscopic features of molluscum contagiosum based on white structures and their correlation with histopathological findings. Clin Exp Dermatol. 2015;40(2):208–210.
