 J Clin Aesthet Dermatol. 2023;16(3):41–43.
J Clin Aesthet Dermatol. 2023;16(3):41–43.
by Baklouti Massara, MD; Khadija Sellami, MD; Soumaya Graja, MD; Ons Boudaouara, MD; Sana Miladi, MD; Fatma Hammami, MD; Emna Bahloul, MD; Tahia Boudaouara, MD; Hamida Turki, MD
Drs. Massara, Khadija, Sana, Fatma, Emna, and Hamida are with the Dermatology Department at Hedi Chaker Hospital at the University of Sfax in Sfax, Tunisia. Drs. Soumaya, Ons, and Tahia are with the Pathology Department at Habib Bourguiba Hospital at the University of Sfax in Sfax, Tunisia.
FUNDING: No funding was provided for this article
DISCLOSURES: The authors report no conflicts on interest relevant to the content of this article.
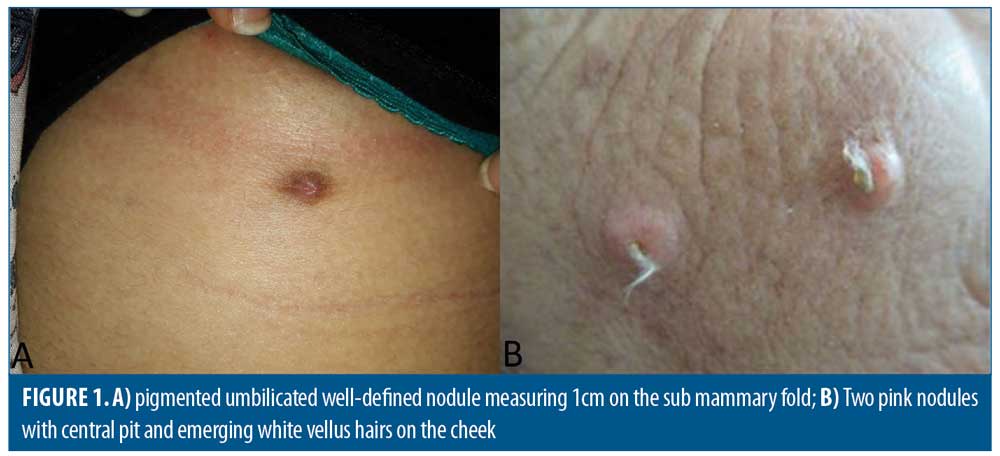
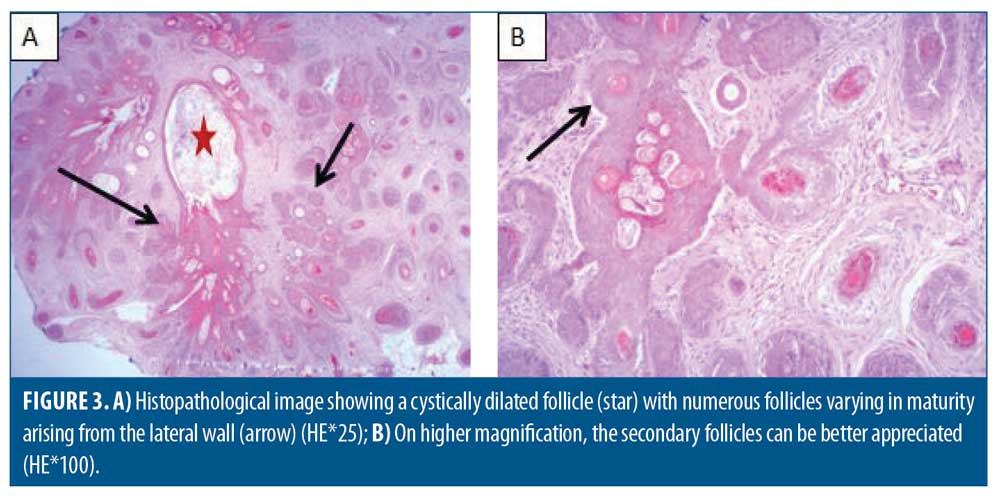
ABSTRACT: Trichofolliculoma (TF) is a rare benign adnexal follicular tumor, described as hamartoma with follicular differentiation according to some authors. It typically appears during adulthood on the face or scalp as an isolated nodule with protrusion of central tufted hairs. We present a retrospective series of eleven patients with histologically confirmed TF to evaluate epidemiological, clinical, and histopathologic characteristics. The mean age at excision was 46 years with extremes ranging from 20 to 75 years. The sex ratio M/F was 0.37. Clinical presentation was a papule or nodule with an average diameter of 6,7mm (2-15 mm), firm with central pit in 54 percent and visible emerging vellus hairs in 18 percent of cases only. The localization was on the face in seven cases (63.6%) and only four cases were located outside the face (scalp [n=2], sub mammary fold [n=1] and shoulder [n=1]). Histologically, a cystically dilated hair follicle containing keratinous material with several mature and immature branched follicular structures is described in all cases. According to our series, TF occurs predominantly in women without age predilection, in the face. Central tufted hairs are only found in a minority of cases corresponding histologically to many secondary vellus hair follicles. In fact, histopathological examination is the gold standard for the diagnosis because clinical diagnosis could be challenging. Histology and dermoscopy may vary according to the age of the lesion. To date, only few case series have been published.
KEYWORDS: Trichofolliculoma, adnexal tumor, dermatoscopy
Trichofolliculoma (TF) is a rare benign adnexal follicular tumor.1 According to some authors, TF is described as hamartoma with follicular differentiation. It typically appears during adulthood on the face or scalp as an isolated, skin-colored papule or nodule with protrusion of tufted hairs from a central pore.1 Atypical presentations may be misdiagnosed as cysts and even some carcinomas. Histopathology confirms the diagnosis when revealing a central dilated follicle, containing keratin and hair shafts with multiple hair follicles in different stages of development.1
Methods
We report a retrospective case series 11 patients with TF seen over eleven years (2011–2020) at Hedi Chaker Hospital of Sfax in the south of Tunisia to evaluate the epidemiological, clinical, dermoscopic, and histopathologic characteristics of TF. All cases were histologically confirmed. We evaluated all cases in which lesion removal was performed and histologically confirmed at the pathology department of Habib Bourguiba Hospital. Clinical data were collected on patient age, sex, clinical diagnosis, and location. Data were also collected on histopathologic finding.
Case Descriptions
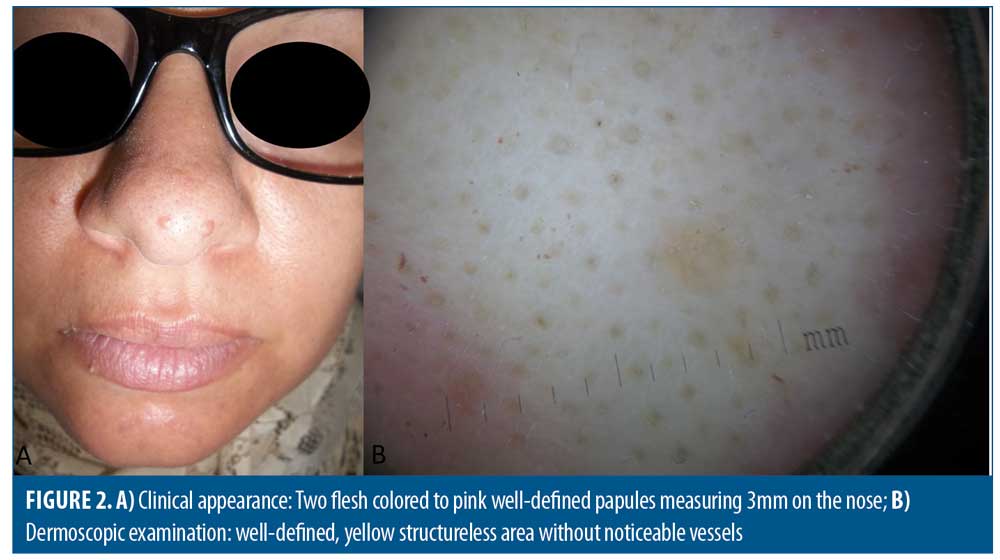
Eleven cases of TF were collected. The mean age at excision was 46 years (extremes: 20–75 years). Three patients were younger than 30 years of age. Seventy-three percent of the patients were female and 27 percent were male. Lesions were evolving for approximately one year in six patients. In one case, the lesion was congenital. The lesion was asymptomatic in all cases, except an occasional whitish discharge in two patients. Clinical presentation was a papule or nodule of average diameter 6.7mm (2–15 mm), relatively firm, and fixed with central pitting in 54 percent and visible emerging vellus hairs in 18 percent of cases only (Figure 1B). The size of the lesion was less than 5mm in six patients, and between 6 and 15mm in five patients. The lesion was pink in four cases, flesh-colored in four cases, whitish in one case, brown in one case (Figure 1A) and red in one case. The lesions were located on the face in seven cases (63.6%; cheek [n=4], forehead [n=1], nose [n=1, Figure 2A], and inferior lip [n=1]). Four cases were located elsewhere on the body (scalp [n=2], sub mammary fold [n=1)], and shoulder[n=1]). The evolution was constantly benign as no cases recurred after complete excision. Preoperative diagnoses were: epidermal cyst (n=3), basal cell carcinoma, nevus, pilomatrixoma, trichoepithelioma, dermatofibroma, angiofibroma, mucoid cyst, supernumerary breast. TF was evoked before excision in only two cases with emerging tufted hairs. Dermatoscopic examination was performed in only one case, showing a well-defined, yellow structureless area without noticeable vessels (Figure 2B). Histologically, all lesions were compatible with TF, with cystically dilated hair follicles containing keratinous material. Several mature and immature follicular structures in all stages were branched on the large central dilated follicle and radiated into the surrounding dermis and sebaceous glands in 45 percent of cases (Figure 3). The stroma was composed of lymphocytic and histiocytic inflammation in most cases with frequent granulomas in two cases (18%). All cases are summarized in Table 1.
Discussion
Many authors have considered TF as a hamartoma rather than a tumor as it is composed of normal hair follicle in an aberrant distribution.1 It is common in adulthood with no definitive racial or sex predilection. Some series described an equal sex distribution.2 The female predominance in our series can be explained by a more frequent consultation of women due to the aesthetic concerns prompted by the lesions. We report three cases that developed in patients younger than thirty, and a female predominance. Onset is usually spontaneous; however, a history of previous trauma has been described in some cases and not in our series.
First reported by Miescher in 1944, TF might be recognized when it is a papule or nodule with central dilated pore through which an immature hair protrudes. A large lobulated mass is rarely reported. It manifests mostly on the face especially around the nose and occasionally on the scalp and more rarely the neck.2 Locations on the lip, external auditory canal, intranasal area, genital area, vulva, eyelid margin and upper extremities have also been reported.3–5
Our series confirm the face localization predominance especially on the cheek. We also describe rare localization on the trunk and the lip. Lesions are mostly solitary but numerous TF on the extremities with varying size and age was also described.4 We report two cases presenting two adjacent lesions which is a rare condition.
In the absence of these characteristics, clinical diagnosis may include epidermal cyst, dilated pore of Winer, trichoepithelioma, molluscum contagiosum, sebaceous hyperplasia, dermal nevus and basal cell carcinoma. We have also evoked other diagnoses such as mucoid cyst on the lip and a supernumerary breast when the lesion was located on the submammary fold.
There is a limited dermoscopic description of TF in the literature. One previous report showed a “firework” pattern consisting of a central brown zone and multiple radial dark brown projections peripherally in a four-month-old lesion.6 Another case showed a bluish nodule with a central white-pink area, shiny white structures, dotted vessels and a central scale.7 The third aspect consists of structureless pinkish white area with a central sluice and a fine peripheral radial serpiginous vascularization.8 Recently, the dermoscopic features of a well-defined, yellow macule with a central white hair plug described as “troll hair” sign surrounded by dilated capillaries were reported.9 However, the number of dermatoscopic observations is too small to draw any conclusions. Dermatoscopy is mainly useful to eliminate other diagnoses whose dermatoscopic aspects are better known.
Central tufted hairs are only found in a minority of cases such as those reported in our series corresponding histologically to a central primary follicle and many secondary vellus hair follicles. The diagnosis is generally histological. We observe a central dilated cavity with an infundibular keratinization that is continuous with the epidermis. The cavity usually contains keratin. Numerous vellus hair follicles, in different stages of development, radiate from the wall of this central cavity. These follicles may in turn give rise to secondary or even tertiary follicles. Rupture of the cystic space in the surrounding dermis can lead to a granulomatous reaction.1 Sebaceous differentiation may be seen within the follicles or the rudimentary structures. Histopathology may vary according to the maturation stage of TF resulting in an increased number of vellus hair secondary follicles.10 TF express CK15, CK17 intensely, as well as BerEP4, markers expressed in normal follicles and in certain follicular tumors but there are no specific markers for TF.10,11 We did not perform immunohistochemistry for our patients since the diagnosis was histologically evident.
Although folliculosebaceous cystic hamartoma contains sebaceous glands converging into a central cyst, it has neither secondary follicles nor hair shaft and there is no reason to believe it is a very late-stage TF. Fibrofolliculoma and cystic trichoblastoma have a different architecture and also lack hair shafts.11
The treatment of choice for TF is surgical excision. The prognosis is good and recurrence after excision has been rarely reported.3 Perineural invasion was described by Stern and Stout in 1979.12 It requires long-term follow-up even if it has no significant malignant potential. There are no reported systemic or skin abnormalities associated with TF. Larger series may better clarify his clinical, histologic and prognostic characteristics.
References
- El-Komy MH, Abdelkader HA. Congenital trichofolliculoma: a very rare presentation. Dermatol Online J. 2020 Jul 15;26(7):13030/qt4g69d9zc.
- Bharti JN, Dey B, Gautam P et al. Trichofolliculoma presenting as lobulated mass: a rare presentation. Int J Trichology. 2014 Jan;6(1):19–20.
- Lee HY, Kim EK, Choi HS, et al. Trichofolliculoma in the Auricle. Ear Nose Throat J. 2021 Feb 15:145561321995599.
- Choi CM, Lew BL, Sim WY. Multiple trichofolliculomas on unusual sites: a case report and review of the literature. Int J Dermatol. 2013 Jan;52(1):87–89.
- Al-Ghadeer H, Edward DP. Congenital Sebaceous Trichofolliculoma of the Upper Eyelid. Ophthalmic Plast Reconstr Surg. 2017 May/Jun;33(3S Suppl 1):S60–S61.
- Panasiti V, Roberti V, Lieto P et al. The “firework” pattern in dermoscopy. Int J Dermatol. 2013; 52: 1158–1159.
- Garcia-Garcia SC, Villarreal-Martinez A, Guerrero-Gonzalez GA, et al. Dermoscopy of trichofolliculoma: a rare hair follicle hamartoma. J Eur Acad Dermatol Venereol. 2017 Feb;31(2):e123–e124.
- Jégou-Penouil MH, Bourseau-Quetier C, Cajanus S et al. [Trichofolliculoma: a retrospective review of 8 cases]. Ann Dermatol Venereol. 2015 Mar;142(3):183–188.
- Shah KM, Der Sarkissian SA, Cheung K et al. Trichofolliculoma – ‘troll hair’ dermoscopy. Australas J Dermatol. 2021 Feb;62(1):90–92.
- Misago N, Kimura T, Toda S et al. A revaluation of trichofolliculoma: the histopathological and immunohistochemical features. Am J Dermatopathol. 2010 Feb;32(1):35–43.
- Romero-Pérez D, García-Bustinduy M, Cribier B. Clinicopathologic study of 90 cases of trichofolliculoma. J Eur Acad Dermatol Venereol. 2017 Mar;31(3):e141–e142.
- Stern JB, Stout DA. Trichofolliculoma showing perineural invasion.Trichofolliculocarcinoma? Arch Dermatol. 1979;115(8):1003–1004.

