 J Clin Aesthet Dermatol. 2021;14(3):17–21.
J Clin Aesthet Dermatol. 2021;14(3):17–21.
by Saurabh Sharma, MD, DNB, MNAMS; Kajal Vinay, MD; and Roopam Bassi, MD
Drs. Sharma and Vinay are with the Department of Dermatology, Venereology, and Leprosy at the Sri Guru Ram Das Institute of Medical Sciences & Research in Amritsar, Punjab, India. Dr. Bassi is with the Department of Physiology at the Sri Guru Ram Das Institute of Medical Sciences & Research in Amritsar, Punjab, India.
FUNDING: No funding was provided for this article.
DISCLOSURES: The authors report no conflicts of interest relevant to the content of this article.
ABSTRACT: Background. The aberration of wound healing leads to scar formation in the form of hypertrophic scars and keloids. Various modalities with variable results have been used in the treatment of keloids.
Objective. We sought to evaluate outcomes in the treatment of small keloids with the combination of intralesional 5-fluorouracil (5-FU) and triamcinolone acetonide versus intralesional bleomycin and triamcinolone acetonide.
Design. Sixty clinically diagnosed keloid lesions in 40 patients aged 18 to 60 years were divided equally into Groups A (n=30) and B (n=30). The combination of intralesional 5-FU and triamcinolone acetonide (TAC) was given to Group A and the combination of intralesional bleomycin and triamcinolone acetonide was given to Group B. Treatment was repeated in both groups at three-week intervals until keloid flattening was achieved or a maximum of 10 treatments were completed. Before treatment, the lesions were assessed using the Vancouver Scar Scale and their size was measured using vernier calipers.
Results. In Group A, 15 (50%) keloids showed an excellent response, 10 (33.33%) keloids showed a good response, three (10%) keloids showed a fair response, and two (6.66%) keloids showed a poor response. In Group B, 23 (76%) keloids showed an excellent response, three (10%) keloids showed a good response, two (6.66%) keloids showed a fair response, and two (6.66%) keloids showed a poor response.
Conclusion. Patient response regarding treatment duration, flattening of lesions, improvements in the Vancouver Scar Scale score, and recurrence rates were statistically significant in Group B. A greater improvement in the signs and symptoms of keloids (with respect to cosmetic problems, restriction of movement, and tenderness) was observed in the patients treated with a combination of intralesional bleomycin and triamcinolone acetonide compared to those treated with a combination of intralesional 5-FU and triamcinolone acetonide.
Keywords: Keloid, 5-fluorouracil, bleomycin, triamcinolone acetonide
Wound healing is a sophisticated, dynamic process, and the aberration of this process leads to scar formation in the form of hypertrophic scars and keloids.1 Hypertrophic scars are different from keloids, as they tend to regress over time and do not extend beyond the margins of the wound.2 The term “keloid” is derived from Greek word cheloide, meaning “crab claw-like appearance.”3 Keloids are formed following the disruption of skin integrity that follows any kind of trauma-like scratch, insect bites, piercings, surgical procedures, and thermal or chemical burns. Keloids most commonly occur on the chest, shoulders, upper back, posterior neck, and earlobes. The incidence of keloids is equal in both sexes and occurs mostly in the second and third decades of life.4 Over the decades, there has been an increase in cosmetic awareness and, hence, the presence of keloids has caused severe distress, leading to sociopsychological upset. Keloids are considered to be cosmetically unacceptable and can even contribute to functional impairment.
From time to time, various modalities with variable results have been used in the treatment of keloids. Successful management of keloids is difficult, because the current treatments far from guarantee a cure or the prevention of recurrence. Intralesional injections of corticosteroid (triamcinolone acetonide [TCA)] 10mg/40mg) has remained a first-line treatment for keloids. Steroids inhibit collagen synthesis and possess anti-inflammatory properties. Multiple injections in the keloid are required to achieve the desired effect. Very often, it is difficult to inject the drug into the lesion, although this can be overcome by softening the lesion either with cryotherapy or pulsed dye laser or by the addition of hyaluronidase or topical application of an immunomodulator, such as imiquimod.5 Adverse sequelae, such as hypo- or depigmentation, telangiectasia, and atrophy are seen in about 20 percent of cases injected with triamcinolone, as reported by Manuskiati and Fitzpatrick.6
5-fluorouracil (5-FU) is classified as an antineoplastic agent that inhibits DNA and RNA synthesis. It induces fibroblast apoptosis without necrosis.7 In addition, 5-FU also inhibits the expression of the type I collagen gene that is induced by transforming growth factor-beta. Skin erythema and ulceration are common adverse effects with 5-FU. These side effects can be overcome by injecting a combination of 5-FU and TCA.8
Bleomycin was introduced by Bodokh and Brun9 as an alternative therapy for keloids and hypertrophic scars based on its action as an inhibitor of synthesis of deoxyribonucleic acid. It has antitumor, antiviral, and antibacterial activity. From a histologic point of view, bleomycin causes the necrosis of keratinocytes. Common side effects include hyperpigmentation and pain during injection and dermal atrophy into the normal healthy surrounding skin. Bleomycin is given intralesionally in the dose of 1.5IU/mL.10
To date, no study has been conducted to compare the efficacy of intralesional 5-FU and TCA to intralesional bleomycin and TCA in the treatment of keloids. Thus, this study sought to compare the efficacy of these two combinations for the treatment of small keloids.
Methods
Study population. Sixty clinically diagnosed keloids (<5×<5×<0.5cm3 in size) were selected from 40 patients visiting the Dermatology, Venereology, and Leprosy outpatient department of the Sri Guru Ram Das Institute of Medical Sciences and Research in Amritsar, Punjab, India. Eligible patients included those aged 18 to 60 years who were willing to give written consent and return for regular follow-up assessments. No more than two lesions were selected in a single patient presenting with multiple lesions and, in such cases, each lesion was included in a different group. Those who met the following criteria were excluded: patients who had received treatment for the same keloid in the past six months; patients with active inflammation, infection, or ulcer in or around the keloid; women who were pregnant or planning a pregnancy; immunosuppressed patients; patients with chronic inflammatory diseases; and patients with a history of renal or liver failure.
Detailed history-taking and clinical examination were conducted for all participants. It was ensured that all 60 lesions selected were keloids, none showed tendency to flatten spontaneously, and all showed extension beyond the site of original injury. The 60 keloid lesions were equally divided into Groups A and B, with 30 lesions in each group. In Group A, the combination of intralesional 5-FU and TCA was administered. While, in Group B, the combination of intralesional bleomycin and TCA was administered. Perilesional sites were cleaned with betadine. No local infiltration of anesthetics was conducted.
Study protocols. In Group A, a single-use U-40, 1-mL insulin syringe was used, in which four units of TCA and 36 units of 5-FU were mixed; then, 0.1 mL of this combination was injected 1cm apart intradermally into the lesion. Separately, in Group B, bleomycin was reconstituted by mixing with 10mL of distilled water to get a concentration of 1.5 IU/mL. Ten units of insulin syringe (equivalent to 0.375 IU=0.25 mL) were injected intradermally 1cm apart followed by intradermal injection of 0.1mL of TCA (40 mg/mL)/cm.
Adverse effects at the time of injection and other complaints during the course of treatment were recorded. Analgesics and antibiotics were given orally when required. Patients were asked to return for follow-up visits every three weeks until the lesions were completely flattened or until a maximum of 10 visits had occurred. A photograph of the keloid lesion was taken before the start of the procedure and after completion of the final visit. Each time, lesions were evaluated objectively using the Vancouver Scar Scale (VSS)10 and subjectively by assessing degrees of pain and pruritus. All healed lesions were followed up on for six months to elucidate any recurrence.
At the end of the study period, the response to treatment in terms of flattening of lesions was categorized as follows: excellent (76% to 100% improvement); good (51% to 75%); fair (26% to 50%); or poor (less than 25% improvement). The results were analyzed objectively, subjectively, and photographically at each follow-up visit and statistically at the end of the study.
Results
The results were evaluated primarily on the basis of treatment duration, improvements in signs and symptoms, improvements in VSS score, flattening of lesions, and recurrence. In Group A, a greater number of treatment sessions were required for flattening of the lesions compared to Group B. Group B lesions (Figure 1) showed better improvements than Group A lesions (Figure 2) in both signs and symptoms with respect to cosmetic problems, restriction of movement, and tenderness.
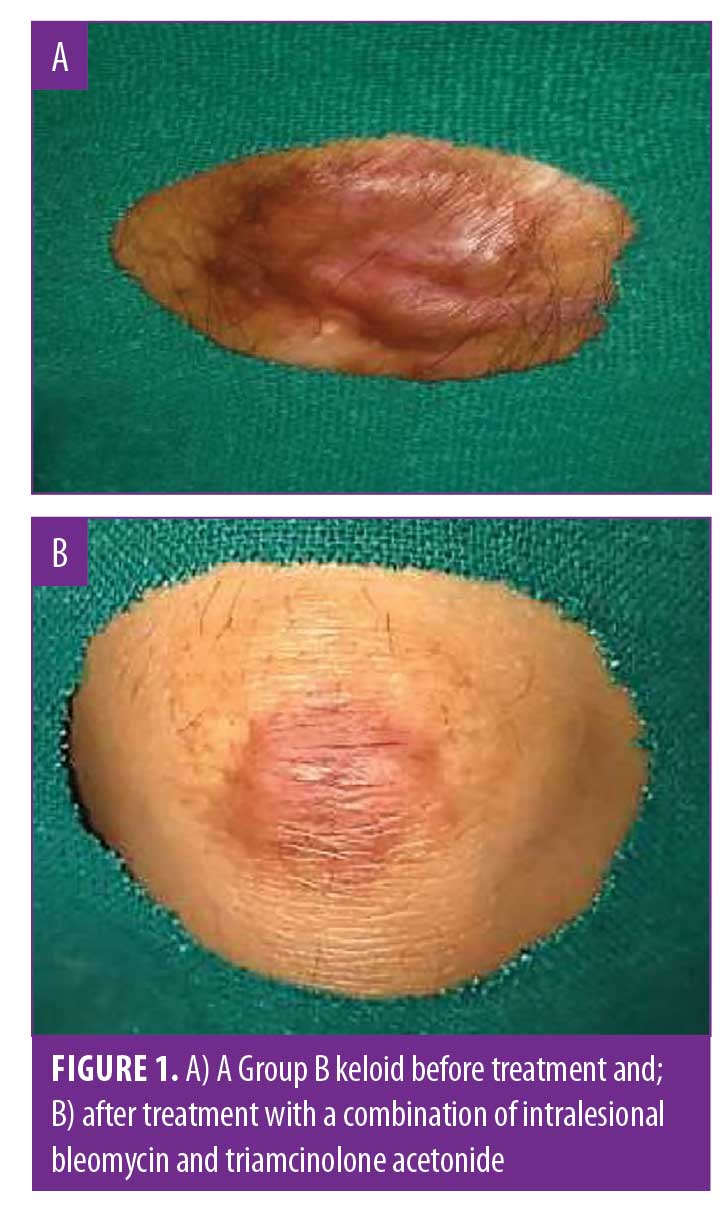
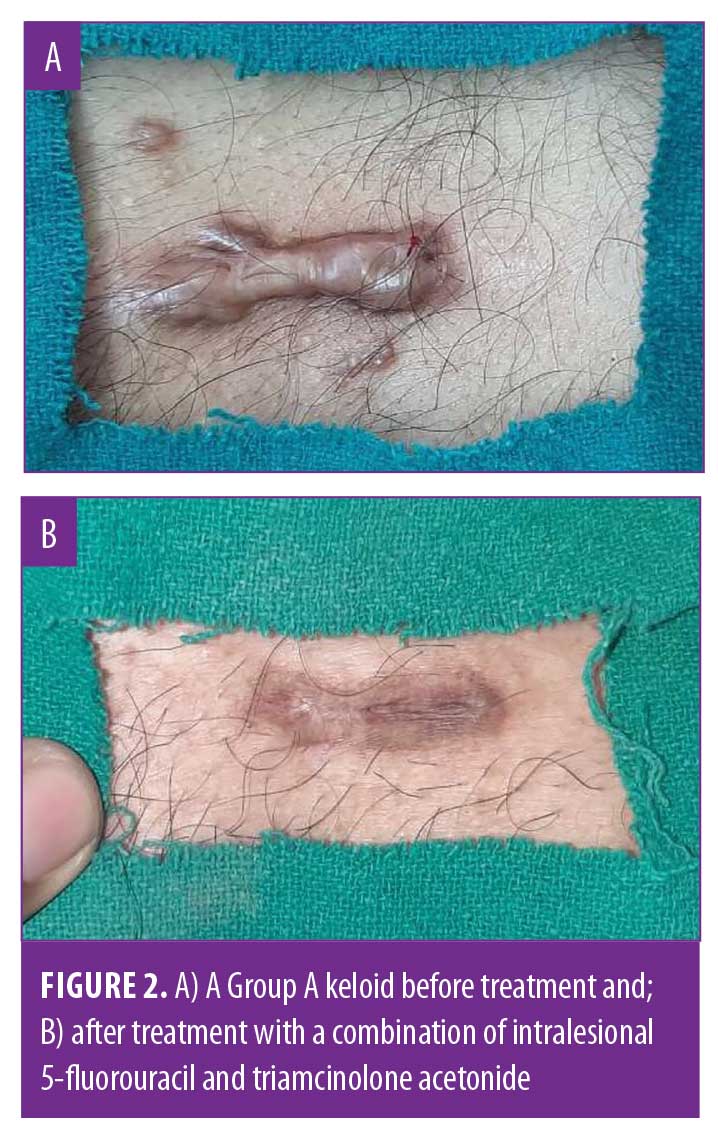
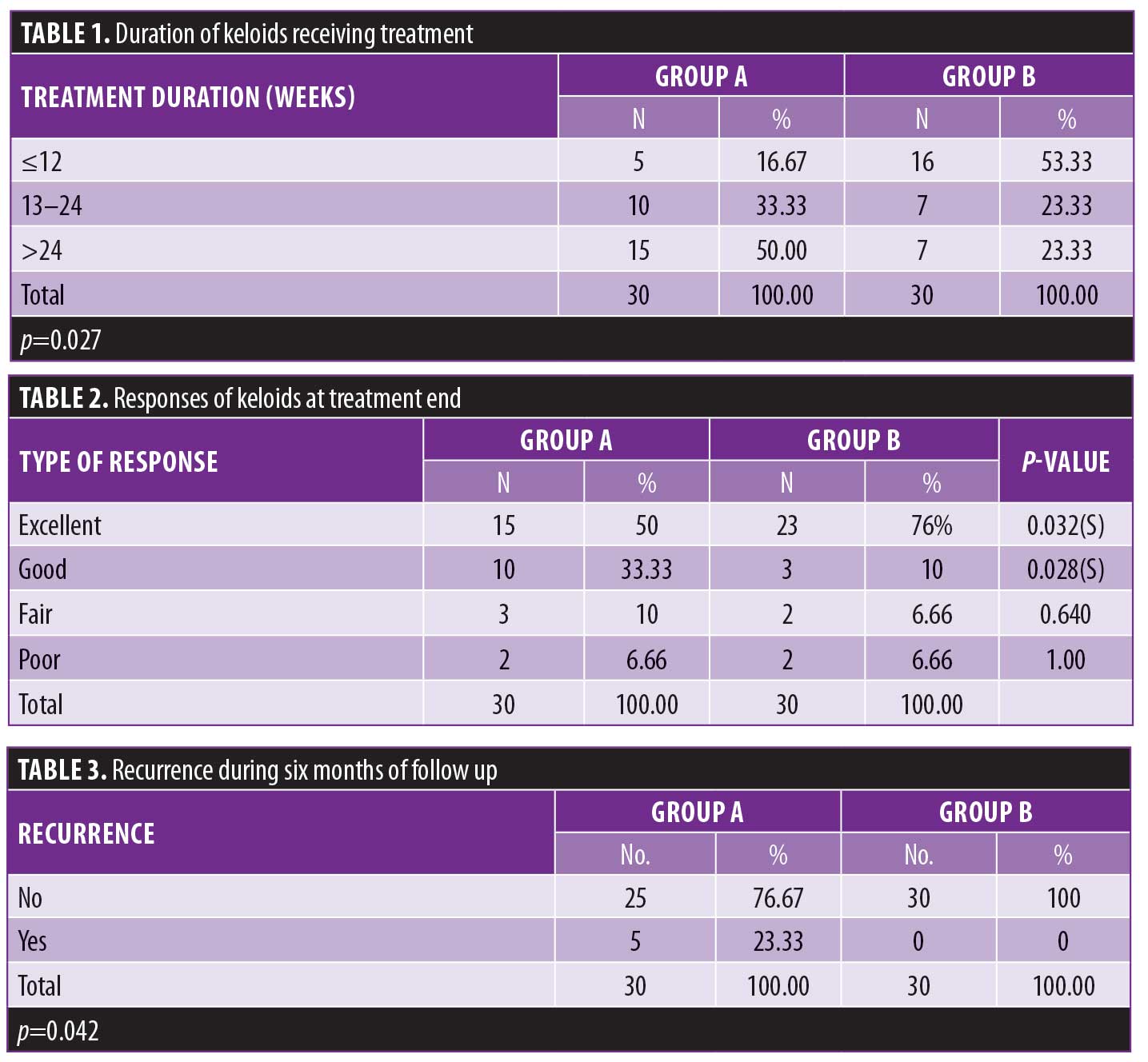
Table 1 shows that, in Group A, the duration of treatment required for flattening the keloids was longer than that in Group B. A chi-squared test revealed a significant difference between the groups. Table 2 shows that an excellent response was seen in 76 percent of lesions in Group B in contrast with 50 percent of lesions in Group A. As such, the treatment response in Group B was better than in Group A. Finally, Table 3 shows that five lesions in Group A showed recurrence at three months of follow-up, in contrast with Group B, where no recurrences were obeserved. This difference was statistically significant (p=0.042). Overall, the response to treatment in terms of flattening, treatment duration, and recurrence was better in Group B than in Group A.
Discussion
Keloids are a benign, well-demarcated area of dense, fibrous tissue overgrowth that extends beyond the borders of the original wound. Various therapeutic modalities, including drugs, compression therapy, laser therapy, 5-FU, bleomycin, radiotherapy, and intralesional steroids are available for the treatment of keloids. A combination of therapeutic modalities is often necessary to achieve optimal results in the treatment of keloids. Therefore, the effect of these drugs can be synergistic when used in combination with one another.
The present study was conducted to evaluate outcomes of small keloids treated with a combination of intralesional 5-FU and TCA versus intralesional bleomycin and TCA. In Group A, the duration of treatment was less than 12 weeks in five (16.6%), 13 to 24 weeks in 10 (33.33%), and more than 24 weeks in 15 (50%) keloids, respectively. In Group B, 16 (53.33%) keloids had a duration of treatment of 12 weeks or less, while it was 13 to 24 weeks in seven (23.3%) keloids and more than 24 weeks in seven (23.33%) keloids. Our study shows that the number of treatment sessions required for complete flattening of lesions was less in Group B, and the difference between the two groups in this regard was significant. Our observation is consistent with that of Kabel et al,12 who conducted a comparative study of the intralesional injection of bleomycin and 5-FU in the treatment of keloids and hypertrophic scars. In this study, the number of intralesional injections of bleomycin required for flattening ranged from 2 to 6, while the number of intralesional injections of 5-FU+TCA ranged from 5 to 6. Khan et al13 conducted a study on the treatment of keloids with the combination of 5-FU+TCA and reported the need for an average of eight sessions. Manuskiatti and Fitzpatrick13 observed in their study that an average of 10 sessions were required to treat keloids with 5-FU +TCA. In an open study by Kontochristopoulos et al,14 20 keloid lesions were treated once weekly with intralesional 5-FU an average of seven times. In our study, we administered 5-FU+TCA and the number of sessions required ranged from 4 to 9, comparable to the number of sessions required for the treatment of keloids with 5-FU alone. Saray et al15 showed similar results in the treatment of keloids and hypertrophic scars with dermojet injections of bleomycin, in that the number of sessions required to successfully treat the lesions ranged from 2 to 6. In another study conducted by Camacho-Martínez et al,16 who treated large keloids with bleomycin ranging in size from 4.0×2.1cm2 to 8.2×3.3 cm2, it was observed that 50 percent of keloids responded excellently within three sessions.
In Group A in our study, the mean VSS scores before and after treatment were 9.07±1.47 and 4.25±1.33 points, respectively, with a 53-percent improvement, while those in Group B were 9.57±1.35 and 2.6±0.86 points, with 74-percent improvement. The intralesional injection of the combination of 5-FU+TCA resulted in improvement in vascularity, pliability, and height. Multiple injections of bleomycin+TCA produced a significant improvement in vascularity, pliability, and height, yet worsening pigmentation relative to the injection of 5-FU+ TCA. The difference between the improvement in VSS scores in the two groups was statistically significant and confirmed that bleomycin+TCA yields a greater improvement. Our observation is consistent with that of Kabel et al,12 who reported a 55-percent improvement in VSS scores following the injection of 5-FU+TCA and a 73-percent improvement in VSS scores after the injection of bleomycin. In a study by Srivastava et al,17 it was observed that 5-FU+TCA led to the lowest survival curves for pliability and pigmentation. A decrease in pigmentation was seen more quickly with TCA+FU than with TCA or 5-FU alone and was highly statistically significant. In another study conducted by Nghi Dinhuu et al18 assessing the treatment of keloids with bleomycin, it was observed that the vascular status was improved by 70.6 percent after treatment and the mean VSS scores for stiffness were reduced by 89.3 percent. Our study showed similar observations, as the improvements in VSS scores were better with bleomycin+TCA, although a worsening of pigmentation was seen in Group B.
In Group A, 15 (50%) keloids showed an excellent response (76%–100% flattening), 10 (33.33%) keloids showed a good response (51%–75% flattening), three (10%) keloids showed a fair response (26%–50% flattening), and two (6.66%) keloids showed a poor response (< 25% flattening). In Group B, 23 (76%) keloids showed an excellent response (76%–100% flattening), three (10%) keloids showed a good response (51%–75% flattening), two (6.66%) keloids showed a fair response (26%–50% flattening), and two (6.66%) keloids showed a poor response(<25% flattening). The results in the two groups were statistically significant in terms of good and excellent responses. In a study conducted by Davison et al,19 it was seen that patients who received 5-FU+TCA without excision had an average lesion size reduction of 81 percent. In another study conducted by Nanda and Reddy,20 a good to excellent response was seen among 72 percent of lesions treated with 5-FU compared to 83 percent of lesions treated with 5-FU+TCA in our study. This was because we combined 5-FU and TCA for a synergistic effect. Our observation is comparable to that of Sreekar et al,20 who conducted a study on the role of bleomycin in the management of hypertrophic scars and keloids. He concluded in his study that 65 percent achieved an excellent response, 15 percent showed a good response, and 10 percent displayed a fair or poor response. In our study, an excellent response was seen in 76 percent of lesions. The better response rate in our study can be attributed to the synergistic effect of TCA combined with bleomycin. Our observations are also similar to those in a study of keloid treatment with intralesional bleomycin conducted by Huu et al,18 who reported that 70.8 percent of lesions showed an excellent response, 17.5 percent of lesions showed a good response, 8.3 percent of lesions showed a fair response, and 3.3 percent of lesions showed a poor response.
In Group A, 16 of 30 (54%) keloids experienced an improvement in cosmetics, 27 of 27(100%) keloids showed an improvement in pruritus, nine of 22 (45%) keloids exhibited an improvement in movement restrictions, six of six (100%) keloids experienced an improvement in pain, and seven of 10 (77%) keloids attained an improvement in tenderness. In Group B, 19 of 30 (65%) keloids showed an improvement in cosmetics, 19 of 19 (100%) keloids experienced an improvement in pruritus, 12 of 15 (80%) keloids had an improvement in movement restrictions, two of two (100%) keloids had an improvement in pain, and seven of nine (80%) keloids demonstrated an improvement in tenderness. The recorded improvements in signs and symptoms were comparable in both groups, although the reduction in the restriction of movement was significantly better in Group B. In a study by Srivastava et al,17 it was observed that pain and pruritus were consistently reduced at every successive session of keloid treatment using 5-FU+TCA. In a different study, Espana et al21 injected 1.5U/mL of bleomycin into keloids and hypertrophic scars of 13 patients using a multiple needle-puncture approach. Patients received between one and five treatments, with each session held 1 to 4 months apart. All patients were relieved of pruritus after the first session. In a study conducted by Saray et al,15 who treated keloids with bleomycin, it was observed that the mean scores for pruritus and pain were improved significantly. In our study, all patients in Group B were relieved from pain and pruritus at the end of the study. This variation in findings among these studies is probably due to the injection of triamcinolone following the injection of bleomycin.
In Group A, atrophy was seen in three (10%) keloids, hyperpigmentation was seen in one (3.33%) keloid, ulceration was seen in 16 (56%) keloids, hypopigmentation was seen in three (10%) keloids, and telangiectasia was seen in one (3.33%) keloid. In Group B, atrophy was seen in one (3.33%) keloid, hyperpigmentation was seen in 17 (56%) keloids, and ulceration was seen in eight (25%) keloids, while hypopigmentation and telangiectasia were not seen in any of the lesions. Patients in both groups who presented with ulcerations in between treatment sessions were advised to perform regular wound cleaning with a betadine solution and their ulcers typically healed in 10 to 12 days. Our observations in Group A are comparable with the findings of research performed by Saurabh et al22 in which atrophy was seen in 12 percent of lesions, hyperpigmentation was seen in four percent of lesions, hypopigmentation was seen in eight percent of lesions, and telangiectasia was seen in four persent of lesions. In another study conducted by Srivastava et al,17 it was observed that, when keloids were treated with 5-FU+TCA, there was telangiectasia in five percent of keloids, atrophy in 10 percent of keloids, and ulceration in 20 percent of keloids. This incidence of atrophy is consistent with that in our study, while the incidence rates of other side effects were in contrast with our findings. In our Group B, atrophy was seen in one (3.33%) keloid, while Kittisak et al23 did not find atrophy in any of their cases. In our study, atrophy might be an adverse effect of TCA, which was used together with bleomycin. In Group B, hyperpigmentation was seen in 17 (56%) lesions, consistent with the findings of both Kittisak el al23 (60%) and Huu et al18 (58%). Ulceration in Group B was noted in eight (25%) lesions, comparable to in the study of Kabel et al,12 who found that ulceration was present in 21 percent of lesions following intralesional bleomycin injection. Telangiectasia and hypopigmentation were not seen in any of the Group B lesions in our study, while hyperpigmentation was significantly present in Group B lesions. In a study by Reddy et al,20 hyperpigmentation resolved after one year of follow-up. In our study, the period of follow-up was only six months, so the patients were reassured regarding the hyperpigmentation.
In our study, five keloids (23.33%) in Group A showed recurrence at three months of follow up, which persisted throughout six months of follow-up. In Group B, no recurrence was seen during the follow-up period of six months. Differences between the two groups in our study were statistically significant. In a study comparing the efficacy and safety of intralesional triamcinolone and the combination of triamcinolone with 5-FU in the treatment of keloids,24 it was seen that 17.5 percent of lesions receiving the combination of 5-FU+TCA experienced recurrence during a follow-up period of 22 months. Our observation is nearly in agreement with this result. Meanwhile, Kabel et al12 did not report any recurrence in lesions of keloids treated with intralesional bleomycin alone. In another study conducted by Saray et al,15 who treated keloids with bleomycin alone, no recurrence occurred during a follow-up period of 19 months.
Limitations. Our study consisted of only 60 keloid lesions measuring less than 5cm by less than 5cm by less than 0.5cm. More randomized clinical trials with a greater sample size that include keloids of all sizes are necessary to confirm our results. The follow-up period should also be longer to better assess for recurrence in all treated lesions.
Conclusion
Given the aforementioned findings, we believe that the type of response—in terms of the number of procedures required and the flattening of lesions, improvement in VSS scores, and the absence of recurrence—was significant in Group B. Improvements in signs and symptoms—in terms of cosmetic problems, the restriction of movement, and tenderness—were also greater in Group B. Ulceration was more commonly seen in Group A, while hyperpigmentation was seen more often in Group B. We also observed a correlation between keloid size and the duration of treatment in our study: smaller keloids with a shorter duration responded better than did larger, longer-term lesions.
References
- Mari W, Alsabri SG, Tabal N, et al. Novel insights on understanding of keloid scar: article review. J Am Coll Clin Wound Spec. 2015;7(1–3):1–7.
- Peacock EE, Jr, Madden JW, Trier WC. Biologic basis for the treatment of keloids and hypertrophic scars. South Med J. 1970;63(7):755–760.
- Son D, Harijan A. Overview of surgical scar prevention and management. J Korean Med Sci. 2014;29(6):751–757.
- Robles DT, Berg D. Abnormal wound healing: keloids. Clin Dermatol. 2007;25(1):26–32.
- Jacob SE, Berman B, Nassiri M, et al. Topical application of Imiquimod 5% cream to keloids alters expression of genes associated with apoptosis. Br J Dermatol. 2003;149 Suppl 66:62–65.
- Manuskiati W, Fitzpatrick RE. Treatment response of keloidal and hypertrophic sternotomy scars: comparison among intralesional corticosteroid, 5-fluorouracil, and 585-nm flashlamp-pumped pulsed-dye laser treatments. Arch Dermatol. 2002;138(9):1149–1155.
- Apikian M, Goodman G. Intralesional 5-fluorouracil in the treatment of keloid scars. Aust J Dermatol. 2004;45(2):140–143.
- Coppola MM, Salzillo R, Segreto F, et al. Triamcinolone acetonide intralesional injection for the treatment of keloid scars: patient selection and perspectives. Clin Cosmet Investig Dermatol. 2018;11:387–396.
- Bodokh I, Brun P. [Treatment of keloid with intralesional bleomycin]. Ann Dermatol Venereol. 1996;123(12):791–794. [Article in French].
- Jones CD, Guiot L, Samy M, et al. The use of chemotherapeutics for the treatment of keloid scars. Dermatol Reports. 2015;7(2):5880.
- Thompson CM, Sood RF, Honari S,et al. What score on the Vancouver Scar Scale constitutes a hypertrophic scar? Results from a survey of North American burn-care providers. Burns. 2015 ;41(7):1442–1448.
- Kabel AM, Sabry HH, Sorour NE,et al. Comparative study between intralesional injection of bleomycin and 5-fluorouracil in the treatment of keloids and hypertrophic scars. J Dermatol Dermatol Surg. 2016;20(1):32–38.
- Khan MA, Bashir MM, Khan FA. Intralesional triamcinolone alone and in combination with 5-fluorouracil for the treatment of keloid and hypertrophic scars. J Pak Med Assoc. 2014;64(9):1003–1007.
- Kontochristopoulos G, Stefanaki C, Panagiotopoulos A, et al. Intralesional 5-fluorouracil in the treatment of keloids: an open clinical and histopathologic study. J Am Acad Dermatol. 2005;52(3):474–479.
- Saray Y, Güleç AT. Treatment of keloids and hypertrophic scars with dermojet injections of bleomycin: a preliminary study. Int J Dermatol. 2005;44(9):777–784.
- Camacho-Martínez FM, Rey ER, Serrano FC, et al. Results of a combination of bleomycin and triamcinolone acetonide in the treatment of keloids and hypertrophic scars. An Bras Dermatol. 2013;88(3):387–394.
- Srivastava S, Patil AN, Prakash C, Kumari H. Comparison of intralesional triamcinolone acetonide, 5-fluorouracil, and their combination for the treatment of keloids. Adv Wound Care. 2017;6(11):393–400.
- Huu ND, Huu SN, Le Thi X, et al. Successful treatment of intralesional bleomycin in keloids of Vietnamese population. Open Access Maced J Med Sci. 2019;7(2):298–299.
- Davison SP, Dayan JH, Clemens MW, et al. Efficacy of intralesional 5-fluorouracil and triamcinolone in the treatment of keloids. Aesthet Surg. 2009;29(1):40–46.
- Reddy R, Harinatha S, Raghunath N. The role of Bleomycin in management of hypertrophic scars and keloids—a clinical trial. Our Dermatol Online. 2015;6(4):404–406.
- España A, Solano T, Quintanilla E. Bleomycin in the treatment of keloids and hypertrophic scars by multiple needle punctures. Dermatol Surg. 2001;27(1):23–27.
- Sharma S, Bassi R, Gupta A. Treatment of small keloids with intralesional 5-fluorouracil alone vs. intralesional triamcinolone acetonide with 5-fluorouracil. J Pak Dermatol. 2017;22(1): 35–40.
- Payapvipapong K, Niumpradit N, Piriyanand C, et al. The treatment of keloids and hypertrophic scars with intralesional bleomycin in skin of color. J Cosmet Dermatol. 2015;14(1):83–90.
- Khalid, FA, Mehrose MY, Saleem M, et al. Comparison of efficacy and safety of intralesional triamcinolone and combination of triamcinolone with 5-fluorouracil in the treatment of keloids and hypertrophic scars: randomised control trial. Burns. 2019;45(1):69–75.

