 by Greg Maguire, PhD
by Greg Maguire, PhD
Dr. Maguire is with NeoGenesis, Inc. in San Diego, California.
FUNDING: No funding was provided for this study.
DISCLOSURES: Dr. Maguire is a part-owner of NeoGenesis, Inc.
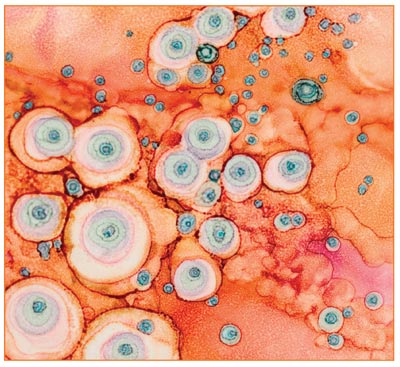
ABSTRACT: Stem cell-based products are rapidly emerging in the marketplace as topical skin care and wound care products. Confusion is prevalent among healthcare providers and end-users about these products. Adipose-derived stem cells, fibroblasts, platelets, and bone marrow-derived stem cells are the most common cells used for stem cell therapeutic development, medical procedures, and skin care products. In this review, the significant advantages of adipose-derived stem cells and fibroblasts in terms of safety and efficacy are highlighted and compared to relatively risky platelets and bone marrow stem cells.
KEYWORDS: Cancer, fibroblasts, inflammation, platelets, secretome, stem cells
J Clin Aesthet Dermatol. 2019;12(8):E57–E69
Skin care and wound healing products with varying ingredients abound in the marketplace. Stem cells and the molecules that they express or release are rapidly emerging in the skin and wound care markets, often with little or no regulatory oversight, even when injected into patients.1 Confusion exists among healthcare providers and end-users about the stem cell types, their molecules, and the use of both cells and molecules in formulating topical and injectable products.
Efficacious topical products can be a great preventative strategy for aging skin and its associated afflictions,2 while wound healing has a great need for efficacious products given the prevalence, costs, and ultimate burden to patients where even death often results from chronic diabetic ulcers.3 Wound complications can be costly. For example, infection can occur if wounds are open. Therefore, treatments that close wounds quickly and for an extended time are sought, and stem cells offer an important therapeutic strategy for achieving these goals. Therapeutic development, medical procedures, and skin care products on the market currently use a variety of cell types, and the molecules that they express and secrete offer efficacy in a number of indications, including those associated with chronological aging. The environmental, cellular, and molecular mechanisms underlying tissue repair and its failure to heal, or heal without fibrosis, are still poorly understood. Although current therapies are limited given our incomplete understanding of tissue repair, progress has nonetheless been significant for this complicated process of wound healing and a number of successful products have emerged. Stem cell types, including the recently discovered dedifferentiated somatic Gata6 cells in the epidermis,4 play critical roles in wound healing. In this review, the first of several describing different cell types used for wound healing, I describe some of the most important and widely used cells used for therapeutic development, medical procedures, and skin care products. This first review highlights the safety and efficacy advantages that adipose-derived stem cells and fibroblasts offer compared to relatively risky platelets and bone marrow-derived stem cells. I will not address in detail induced pluripotent stem cells (iPS), used by one company (RxGenesys; Miami, Florida), given that these cells are not ready for therapeutic development.5 Because of genetic and epigenetic reprogramming errors in these cells,6,7 a number of resulting abnormalities occur, including their secretomes inducing cancer and fibrosis.8 While this review specifically highlights stem cell-based therapies for skin, much of what is reviewed here will pertain to healing other tissues.
Fibroblasts
Mesenchymal stem cells and fibroblasts produce extracellular matrix (ECM), regulate inflammation and the immune system, mediate reparative processes, and serve as pluripotent mesenchymal cells for the generation of multiple cell types in the skin during maintenance and healing processes. Fibroblasts are responsible for expressing, releasing, and depositing ECM molecules, such as several types of collagen, allowing for other cells to migrate along a three-dimensional ECM scaffold to generate the architecture of the skin. Simple ECM topology constructed by the fibroblasts is important because mesenchymal stem cells residing in the ECM will likely alter their paracrine secretion profile depending on the topology; some topologies, presumably ones associated with deregulated ECM, can elicit proinflammatory cytokines such as interleukin (IL)-6.9 Further, breakdown products of the ECM, including hyaluronic acid (HA) fragments below 800 kDa (with some exceptions) will lead to classically activated macrophages, whereas larger HA molecules induce the anti-inflammatory M2 macrophage phenotype,10 with maximal specific binding at the CD44 receptor occurring at about 1,000 kDa.11 Fibroblasts release HA that is attached to exosomes, part of a glycocalyx that surrounds the exosome,12 and incorporates into and helps to build the ECM.13 Additionally, fibroblasts produce bioactive molecules that are involved in several physiological processes, including angiogenesis and tissue repair.14 Clinical trials have demonstrated the effectiveness of fibroblasts to heal chronic venous leg ulcers15 and dystrophic epidermolysis bullosa,16 while the secretome from fibroblasts has been used in an acellular collagen hydrogel to heal full-thickness skin wounds in a mouse model.17 Fibroblasts have been shown to heal an animal model of epidermolysis bullosa, whereas bone marrow stem cells (BMSCs) failed to do so.18 The secretome from fibroblasts has long been studied and used in the market to successfully treat aged and photodamaged skin as a daily use topical product.19
Although the principal cells of connective tissue are called fibroblasts, this is a classification for many cell phenotypes.20 Tissue-specific environments are generated by stromal cells21 and differing phenotypes of the fibroblasts can produce either regeneration or fibrosis depending on the need of the tissue that has been wounded. The phenotype of fibroblasts is under the control of many parameters, including mesenchymal stem cells that direct the fibroblast’s secretion and placement of ECM.22 Indeed, this is likely a key mechanism in the ability of adipose-derived mesenchymal stem cells (AMSCs) to induce scar-free wound healing.22,23 When fibroblasts are cultured with the exosomes from adipose-derived stem cells (ADSCs), the concentration of exosomes was shown to be proportional to the proliferation rate of fibroblasts and the expression of N-cadherin (cyclin-1; PCNA). Further, at an exosome concentration of 50ug/mL, the expressions of collagen III and collagen I were enhanced in the fibroblasts, suggesting an important mechanism by which exosomes secreted from ADSCs optimize a fibroblast phenotype for wound healing.24 As another phenotype capable of sensing adipokines released by adipocytes, dermal fibroblasts that express receptors for adiponectin and leptin will significantly increase their production of HA and collagen, major ECM components of the dermis. Other phenotypes of dermal fibroblasts secrete matrix metalloproteinases (MMPs) and might therefore exert an antifibrotic effect.25
Tissue resident fibroblasts represent a discrete proportion of cells that reside in a given organ and are mostly quiescent or resting cells that are capable of responding to extrinsic cues, including growth factors, cytokines, and mechanical stress, to become activated.26 The parenchymal injury associated with a nascent and growing tumor is an example of such a cue that can lead to the activation of normal fibroblasts, thereby giving rise, at least in part, to the cancer-associated fibroblasts (CAF) expanding in the tumor.27 The conversion of normal fibroblasts to the CAF phenotype has been shown to be induced by the secretome of BMSCs.28 However, even in CAF cells, the outcome of the secretome might limit cancer progression, especially if the tumor environment is normalized.29 In aged skin, protein secretion by papillary fibroblasts was significantly altered by aging,30 and a senescent fibroblast phenotype, called the senescence-associated secretory phenotype (SASP), develops that is associated with epithelial proliferation and tumorigenesis31 and with melasma pathophysiology.32 Aged fibroblasts, exacerbated by a high-fat diet for example, not only reduce their expression of genes involved in ECM formation, but also gain traits similar to neonatal proadipogenic fibroblasts.33 To remediate the aberrant secretome from fibroblasts in aging skin, the topical use of a secretome from fibroblasts with a nonsenescent phenotype has been successfully used to treat aged skin and reduce hyperpigmentation.34
Platelet-rich Plasma (PRP)
In-vitro mesenchymal stem cell (MSC) expansion media can affect the cell’s phenotype. Platelet lysate supplemented media, as used in PRP procedures, favors a proinflammatory MSC phenotype and the secretion of granulocyte macrophage-colony stimulating factor (GM-CSF), which might enhance immune cell recruitment and the maintenance of macrophages in an M1, prototypical inflammatory phenotype.35 Classically activated M1 macrophages are considered the proinflammatory subtype, whereas alternatively activated, M2 macrophages are known to possess anti-inflammatory properties.36 Although most platelet interactions with other cell types are restricted to within the blood vessels, outside of the blood vessels, platelets colocalize with macrophages in several models for cutaneous inflammation, where they suppress the expression of anti-inflammatory markers and enhance the synthesis of proinflammatory mediators in the macrophages with which they interact.37 Therefore, as a proinflammatory procedure, PRP is not generally recommended for therapeutic development. However, if PRP is used for a procedure, follow-on treatment with the secretome from ADSCs can be used because of its proresolving effects (see below).
BMSCs
Blood enters a tissue because of a significant need to close the wound quickly and fight foreign invaders, with BMSCs entering the wound to facilitate the initial phase of wound healing by accelerating rapid closure of the wound38; a proinflammatory response also ensues.39 The recruitment of blood, including BMSCs40,41 and monocytes, to build a cellular and chemically mediated cytotoxic wall, is distinctly different from the M2-mediated anti-inflammatory response mediated locally in the skin and used to build a cellular wall against foreign invasion.39 Neutrophils are usually the first leukocytes to arrive at the site of inflammation.42 Recruited neutrophils mediate acute inflammation through the release of lytic enzymes from their granules, producing reactive oxygen intermediates that are critical for the clearance of invading bacteria. BMSCs help to maintain the viability and activity of neutrophils by prolonging their survival and function, thus prolonging and enhancing the inflammation.43
Macrophages are innate immune cells resident in the skin and are an important part of the early inflammatory response,44,45 where hypoxia decreases macrophage polarization from the proinflammatory M1 to the anti-inflammatory M2 phenotype by BMSCs, needed to promote wound healing. Toll-like receptor 4 (TLR4)-primed BMSCs mostly secrete proinflammatory mediators (BMSC1 phenotype), while Toll-like receptor 3 (TLR3)-primed BMSCs (BMSC2 phenotype) express mostly immunosuppressive molecules.46 Hypoxia is known to trigger TLR-4 signaling and induce inflammation.47 Thus, the local injury environment, where blood-borne BMSCs infiltrate a wound in hypoxic conditions, must be taken into account when evaluating the therapeutic potential of BMSCs, where, in skin injuries, they will not induce an anti-inflammatory M2 macrophage phenotype. Likewise, BMSCs cultured in hypoxic conditions (BMSC1 phenotype) will secrete proinflammatory molecules,45 and the BMSC2 phenotype is procancerous in both in-vitro and in-vivo models.48 The alarmin HMGB-1 that stimulates inflammation through the RAGE receptor is an important factor in generating scars49 and has also been shown to be highly upregulated by culturing BMSCs in hypoxic conditions.50 Whether HMGB-1 is released in the secretome of BMSCs is not known. However, some data support the notion given that, in bone marrow cells cultured in hypoxic conditions, HMGB-1 is released.51 Other factors, such as fatty acid exposure, can also induce a proinflammatory phenotype in BMSCs.52 When comparing BMSCs to ADSCs, Sukho et al53 showed that conditioned media from ADSCs induced a more anti-inflammatory M2 state than did the conditioned media from BMSCs. Therefore, when considering BMSCs for therapeutic development, the secretome of BMSCs cultured in hypoxic conditions might be more proinflammatory than that from BMSCs cultured in normoxic conditions and, regardless of the culture conditions, the conditioned media from ADSCs promotes a noninflammatory M2 state better than does the conditioned media from BMSCs. In comparison with BMSCs, hypoxic culture conditions for the ADSCs had little effect on a cell’s phenotype or the contents of its secretome.54 BMSCs become activated and home in on the inflamed tissue through inflammatory cytokines that prime MSCs for chemotaxis.55 During the inflamed state with blood infiltration, invading BMSCs will express high levels of the Wnt family member 5A (WNT5A) protein,56 shown to be associated with cancer development and progression,57 and release proangiogenic and immunosuppressive factors that increase the immunosuppressive and angiogenic capacities of tumors, thus rendering the cancer cells more aggressive and more prone to metastasis.58 BMSC transplants are associated with an increased risk for cancer,59 including melanoma.60 Conditioned media from BMSCs, acting through a cytokine network,61 has been shown to upregulate antiapoptotic and proliferative genes in cocultured breast tumor cells that correlate with tumor progression and poor prognosis62 and also promote angiogensis in prostate and breast cancer cells63 as well as in colorectal cancer.64 In-vivo studies have shown that the conditioned media from human BMSCs induced gastric cancer growth,65 while other studies revealed that the in-vivo effects of induced cancer growth can be mediated by the exosomes of BMSCs.66 One mechanism by which BMSCs might induce cancer is through the conversion of the normal fibroblast phenotype to the CAF phenotype by the BMSC secretome.28 BMSCs also secrete chemokine (C-C motif) ligand 5 (CCL5) protein, observed to mediate BMSC actions in promoting breast cancer metastasis67 and to mediate the proliferation of prostate cancer cells by the BMSC secretome.68 BMSCs have also been demonstrated to promote breast cancer metastasis through the activation of neutrophils. Tumor necrosis factor alpha (TNF-alpha) is part of the inflammatory response and is released by macrophages and other cells. TNF-alpha-activated BMSCs expressed high levels of CXCR2 ligand, which activates a G-protein-coupled receptor and triggers a variety of intracellular signaling cascades that mediate numerous pathological processes in cancer.69 When coinjected with mammary tumor cells in mouse mammary glands, TNF-alpha–activated BMSCs recruited more neutrophils to the tumor. In turn, the recruited neutrophils dramatically promoted the invasion and migration of tumors cells and promoted their metastasis in lung colonization.70 The conditional medium of human BMSCs promoted the proliferation, migration, and invasion of PC-3 prostate cancer cells, and the expressions of MMP-2 and MMP-9 in PC-3 were upregulated.71 Vallabhaneni et al72 demonstrated that the microRNA and protein composition of secretome from BMSCs is tumor-supportive, and more than 30 percent of proteins are antiapoptotic and cell-proliferative. In another study, BMSCs induced platelet activation, and the platelets then enhanced the effects of BMSCs on tumor proliferation and metastasis,73 suggesting that the use of PRP and the secretome of BMSCs in conjunction with one another might have very procancerous effects. In contradistinction to the procancerous effects of BMSCs in both in-vivo and in-vitro models, ADSCs suppressed cancer growth in vivo.74
Chen et al75 showed that BMSCs secreted differential levels of numerous cytokines compared to dermal fibroblasts, such as significantly greater amounts of epidermal growth factor, keratinocyte growth factor, insulin-like growth factor 1 (IGF-1), vascular endothelial growth factor alpha, platelet-derived growth factor with two B subunits, erythropoietin, and thrombopoietin but significantly lower amounts of IL-6 and osteoprotegerin. Although IGF-1 plays a role in wound healing, the expression of IGF-1 in BMSCs is extremely high—49-fold higher at the messenger RNA (mRNA) level and 22-fold higher at the protein level in the conditioned medium compared to dermal fibroblasts—and might pose health risks when the exposure is high and constant. For example, many studies have shown that IGF-1 is a primary mediator of the effects of growth hormone (GH) and increases the probability of cancer,76 including breast cancer.77,78 The exosomes released from BMSCs also contain mRNA that can promote a state of dormancy in breast cancer cells,79 which is a state that can protect cancer cells from chemotherapy for years.80 BMSCs also recruit macrophages, part of the inflammatory response that further induces proliferation of cells.81 Interestingly, when the skin is wounded where macrophages and other immune cells infiltrate the skin and interact with epithelial stem cells (EpSCs), the EpSCs present an epigenetic memory of the wounding event that elicits a more proliferative phenotype.82 Given that BMSC secretome recruits macrophages,75 the BMSCs might be contributing to the epigenetic memory in EpSCs that induces the more proliferative phenotype. Macrophage recruitment also means that more IL-4, secreted by a number of immune cells, including T-cells and macrophages,83,84 will be present in the tissue, with a resulting propensity for the development of scleroderma.85
Further, BMSCs seem to induce proliferation, migration, and chemotaxis,86 as well as differentiation of resident stem cells to somatic cells87 by releasing factors such as GDF11.88 Not only will frequent cycling of stem cells lead to depletion (exhaustion) of local stem cell populations,89 but we can also think of cancer as wounds that do not heal,90 with the wounds characteristic of constant cell cycling. Wounds have long been known to promote cancer,91 and the recruitment of BMSCs,81 normally not present in skin in significant numbers, during wounding might thus play a role in developing the cancerous phenotype through the aforementioned mechanisms involving IGF-1 and macrophages. BMSC transplants are known to be associated with recurring cancer,59,92 whereas ADSC transplants have not been associated with cancer,93,94 and ADSC exosomes have even been shown to suppress cancer growth.95 Like most cell types, BMSCs exist as a number of phenotypes, with one major phenotype resulting in collagen deposition, expression of proinflammatory mediators, and a reversal of the MSC-established suppressive mechanisms of T-cell activation. The mechanism of fibrosis are similar in all tissues, and one phenotype of BMSCs is fibrogenic, expressing glioma-associated oncogene homolog 1 identified in the human and mouse bone marrow, where it plays an important role in bone marrow fibrosis.96 That BMSCs induce a rapid inflammatory and healing response for initial wound closure and infection control is illustrated by recent results where the administration of BMSCs to patients with lower-extremity chronic wounds only works to reduce the wounds for the initial two weeks of treatment, whereas, at 12 weeks, there are no effects.97 For complete wound healing beyond the initial M1, profibrotic, and proinflammatory responses induced by BMSCs, the secretome of ADSCs is required to promote the M2 anti-inflammatory phase of wound healing.53,98 Furthermore, transplantation of BMSCs leads to an aging effect in the tissue as measured by the p16 biomarker.99 How this is related to the exhaustion of the endogenous stem cell pool and whether the secretome from BMSCs also induces the increased p16 aging effect is not known. BMSC transplants have been reported in several studies to induce toxic epidermal necrolysis,100,101 an extreme inflammatory response. Toxic epidermal necrolysis (TEN) involves inflammatory natural killer (NK) cells,102 and the mechanism by which BMSCs induce TEN might include the enhancement of interferon-gamma (IFN-gamma) release. In this regard, coculture of BMSCs and NK cells, even without cell-cell contact and therefore acting through the BMSC secretome, was shown to enhance IFN-gamma production in NK cells.103
Unlike ADSCs, experimental data have provided evidence that some fibroblasts in fibroblast foci (fibroblast clusters in fibrotic tissue) can be derived from BMSCs. The circulating peripheral blood-derived fibroblasts derived from BMSCs (called “fibrocytes”) have fibroblast-like properties and express CD45+ collagen I+ CXCR4+.104 BMSC-derived fibrocytes can be chemotactically gathered to damaged lung tissue sites and play a key role in the establishment of fibrosis at the injured sites.105
We must also consider that tumor cells and mesenchymal stem cells migrate from the primary tumor site to the bone marrow,106 and therefore, using BMSCs and their secretome for therapeutic development or for skin care products (AnteAGE®; Irvine, California) might be compromised by a cancer phenotype, as well as the likelihood of inducing inflammation, overproliferation, fibrosis, and replicative stress.88
ADSCs
In a seminal study, ADSCs and their exosomes derived from cancer patients are safe and of therapeutic benefit, indicating that expanded ADSCs donated by cancer patients remain unaffected by patient condition, including cancer.107 This is in contrast with BMSCs, which present a number of potential dangers to the patient.108 Although ADSCs serve as a precursor for many cell types, their most important function is signaling to surrounding cells, inducing the cells to differentiate into specialized cells, including dermal fibroblasts and keratinocytes.109 Signaling from ADSCs in the skin is so important that it is even necessary for the activation of epidermal stem cells,110 including those in the hair follicle.111 ADSCs from the dermis are able to differentiate into multiple cells types, including adipocytes112 that are required for wound healing.113 Adipocytes themselves, differentiated from ADSCs, have been successfully used to treat soft-tissue diseases when injected subcutaneously. In a study, treated patients were followed for one year without adverse events.114 In an animal model of diabetic ulcer, nanofat-containing ADSCs, implantation was used to successfully close the wounds115 and treat facial wrinkles in human patients.116 Interestingly, under identical culture conditions, BMSCs are more inclined than ADSCs are to differentiate into adipocytes.117 Dermal adipocytes are necessary for maintenance and healing of the skin given that they secrete a number of cytokines and growth factors and recruit fibroblasts to wounds.113 Skin-derived adipose mesenchymal stem cells (SMSCs) mediate potent anti-inflammatory effects in the surrounding tissue, including the immunomodulation of macrophages into an anti-inflammatory phenotype,118 exhibiting M2 anti-inflammatory characteristics.119 SMSCs also inhibited the induction of pathogenic T-helper type 1 (Th1) and Th17 cells and markedly suppressed the development of experimental allergic encephalomyelitis in a mouse model of multiple sclerosis.120 SMSCs have also been shown to be superior to BMSCs in healing spinal cord injuries in an in vivo rat model.121 ADSCs have been shown to heal skin,122 including the chronically irradiated skin of cancer patients,123 pressure ulcers, even if derived from diabetic patients,124 acid burns,125 atopic dermatitis,126 and many other organs, including the lungs and liver,127 and have additionally been found to inhibit B-cell proliferation, thereby shifting the cytokine profile of B-cells toward an anti-inflammatory profile.98 In diabetic patients, the wound healing of ulcers might be augmented with the inhibition of advanced glycation end-products (AGE) given that Gong et al128 showed that AGE inhibited the proliferation of ADSCs, leading to human ADSC apoptosis, and inhibited endothelial cell-directed differentiation. In a rabbit model of skin wounds, ADSCs exhibited better epithelial regeneration and collagen deposition into the wound and better forming of normal, nonscarring skin tissue with normal architecture compared to BMSCs.129 The wound healing effects of the secretome from ADSCs appears to be mediated, in part, by the large fraction of molecules in the secretome that are devoted to ECM regulation and remodeling,130 reepithelialization, collagen deposition, and neovascularization.131 Although hypoxic culture conditions for the ADSCs have little overall effect on the secretome,54 a number of proteins involved in ECM regulation and scar-free healing are upregulated, including collagen III.130 Part of the wound healing effects of ADSCs might be mediated by their paracrine actions by enhancing the proliferation of fibroblasts and keratinocytes.132 In chronic wounds, the healing phases are all prolonged, with significant infiltration by neutrophil granulocytes.133 The secretome of ADSCs can interrupt this cycle and allow wound healing to occur by decreasing the inflammatory state, promoting cell migration and proliferation, as well as by the induction of angiogenesis and by controlling fibroblast migration and proliferation. This has been demonstrated in digital wounds treated with occlusive dressings that maintain a moist wound environment with preservation of the endogenous ADSC and fibroblast secretome within the wound site.134 ADSC secrete macrophage migration inhibitory factor, one of the proteins that has been identified to inhibit fibrosis.135 In liver fibrosis, similar to in skin, an overproduction of collagen by fibroblasts during the damaged state leads to scar tissue. The therapeutic effect of ADSCs on the symptoms of cirrhosis and liver fibrosis is based on ADSC-secreted growth factors, anti-inflammatory effects on stellate cells (a type of pericyte), and the antifibrotic and angiogenic effects of ADSC-secreted proteins.136 In a murine model, ADSCs prevented fibrosis in steatohepatitis by suppressing IL-17-mediated inflammation.137 The ADSC secretome has been used to reduce the scarring (involving fibrosis) following acne lesions in an animal model.138 The secretome from ADSCs is also critical to the development and maintenance of hair follicles.111 In humans treated with fractional carbon dioxide laser, the recovery phase was augmented with the conditioned media from ADSCs, where erythema, melanin, and transepidermal water loss were reduced, while mRNA for procollagen III was enhanced 2.6 times compared to the control.139
Punch grafts from human patients containing ADSCs have been used to successfully treat chronic ulcer wounds in a randomized, controlled study.140 ADSCs also can switch activated-M1-like inflammatory macrophages to a M2-like phenotype,141 an anti-inflammatory phenotype142–145 able to reduce adipose tissue inflammation and reduce insulin resistance.146 The ability of the secretome from ADSCs to drive the M2 anti-inflammatory state is superior to that of the secretome from BMSCs.53 The ADSC secretome has also been shown to decrease the lipopolysaccharide-induced increases in M1 marker expression by inhibiting both the mitogen-activated protein kinase and nuclear factor k B pathways, and increased the expression of M2 markers by activating the signal transducer and activator of the transcription 3 pathway.147 AMSCs, acting through the molecules they release, also reduce MMP-1 expression in ultraviolet-irradiated human dermal fibroblasts,148 have antioxidant effects,149 reduce the histological and immunochemical consequences of photoaging,150 and significantly reduce ultraviolet-induced skin wrinkles.109 ADSCs also regulate dermal fibroblasts to secrete more collagen type III,151 known to be involved in scarless instead of fibrotic wound healing as mediated by the exosomes released by ADSCs.21 Antiaging effects of ADSCs in the skin have also been observed through the reduction of AGE levels110 and the regulation of melanocyte proliferation, melanin content, tyrosinase activity, and tyrosinase mRNA levels through low levels of IL-6 in the conditioned media.152
Several proteins released more abundantly or exclusively by ADSCs—namely, AXL, CCL2, CLU, CRLF1, LGMN, and PCSK9153—were found to be significantly associated with the regulation of neuronal death and apoptosis. These bioactive factors might contribute to the modulation of neuroinflammation exerted by the secretome of ADSCs in preclinical models of neuropathic pain by activating different mechanisms. AXL is a receptor tyrosine kinase that regulates the innate immune system activation and which controls the phagocytosis of dead neurons. Furthermore, in a model of neurodegeneration, Maguire et al154 showed that the secretome from four cell types, including ADSCs and FBs, was able to rescue neurons and other cells from oxidative stress that would have otherwise killed the cells.
The results of ADSCs are sometimes confused with those from whole-fat tissue. While whole-fat-tissue transfer has been successfully used to heal digital ulcers in patients with systemic sclerosis,155 oncological follow-up for up to 10 years following fat transfer has suggested no increased risk for cancer to the patient.156 A meta-analysis of 1,453 patients with a mean follow-up period of 16.3 months (range: 1–156 months) in fat grafts for breast reconstruction showed no increased incidence of breast cancer.157 In-vitro and in-vivo studies have indicated that AMSCs inhibit cancer growth,92 as would be expected given that they are known to build the ECM, and a normal ECM is important to inhibiting cancer growth through a process of dynamic reciprocity.158 In human cells,159 in-vitro studies show that fat tissue but not fat-derived stem cells increases breast cancer xenograft growth rates significantly. In-vitro, three-dimensional culture studies of ADSCs further suggest their safety in breast tissue, as the ADSCs formed acinar-like structures and showed characteristics of epithelial differentiation when stimulated by the breast epithelial cell line HBL-100.160 The safety profile in ADSCs is relatively well characterized, including nuclear stability as they proliferate,161 making these cells a valuable tool for cancer therapeutics,162 including the delivery of paclitaxel to cancer patients.163 A one-year follow up of patients with an average age of about 50 years who were receiving injections of autologous ADSCs for osteoarthritis observed no adverse events together with improved pain levels and diminished disease progression.164 In a Phase II clinical trial, patients were followed for six months following the injection of allogeneic ADSCs for the treatment of perianal fistulas. No related adverse events were observed and closure of the fistula was realized in most patients.165 In another Phase II clinical trial, patients were followed for two years following the injection of allogenic ADSCs for Chron’s fistula without adverse side effects and with complete healing observed in 80 percent of the patients.166 In a Phase IIb double-blinded, randomized, placebo-controlled study of ADSCs injected for osteoarthritis, significant improvement and no adverse events were seen in a six-month follow-up.167 Thus, the safety profile of ADSCs and their secretome, even when injected, is well established in humans.
Indeed, using in-vitro and in-vivo methods, Lee et al168 showed that the secretome from ADSC attenuates the proliferation and migration of B16 melanoma cells in culture and in a mouse xenograft model, suggesting that the secretome of ADSC might be useful for anticancer therapeutic development. Also, one study indicated that ADSCs inhibit the proliferation and induce apoptosis of hepatic cancer cells,169 while Ko et al94 demonstrated that the exosome fraction of the secretome derived from AMSCs suppressed hepatocellular carcinoma growth. In comparison, the secretome from BMSCs promotes the metastasis of hepatocellular carcinoma growths.170 Xie et al171 showed that the conditioned media from ADSCs was able to suppress liver cancer cell growth through the downregulation of epithelial mesenchymal transition signaling, and Yu et al172 found that the conditioned media from ADSCs reduced cancer cell viability by an induction of cell apoptosis and S-phase-arrest in bladder tumor cells. In a melanoma mouse model, the conditioned media of ADSCs was shown to have an antiproliferative effect on melanoma cells and shown to occur through cell-cycle arrest and apoptosis of tumor cells, and ADSCs themselves were suggested to have an inhibitory effect on the growth of A375SM cell-derived tumors in vivo.173 In a breast cancer model, Ryu et al174 demonstrated that ADSCs inhibit proliferation and induce apoptosis of MCF-7 breast cancer cells. ADSCs have been revealed to have an inhibitory effect on the proliferation of androgen-responsive (LNCaP) and androgen-nonresponsive (PC3) human prostate cancer cells.175 Another possible mechanism through which the secretome of ADSCs can suppress cancer is through the inhibition of the mammalian target of rapamycin,176 a powerful activator of proliferation of cells that is upregulated in cancer.177
ADSCs have also been shown to modulate immune function in a number of favorable ways, reflected in the ability of the secretome from ADSCs to enhance the survival of skin allografts.178 A number of studies have revealed that ADSCs were able to inhibit activated T-cell proliferation with or without direct ADSC-T cell contact,179 and the secretome alone from ADSCs can suppress T-cell proliferation, differentiation, and activation.180,181 Coculture of peripheral blood mononuclear cells with ADSCs resulted in the inhibition of proinflammatory T-cells and the induction of T-cells with a regulatory phenotype, characteristic of an anti-inflammatory response.182 Also, in a 32-month follow up of a human case study where ADSCs were derived from liposuction of the patient, bone reconstruction was demonstrated without any inflammation for the duration of the 32-month study.183 Autologous ADSCs were also used for erectile dysfunction in a Phase I, three-month follow up with significant results and no adverse events.184 The lack of expression of MHC-II proteins in ADSCs that have been shown to be present in the secreted exosomes of BMSCs is another reason for the successful allogeneic administration of the ADSC secretome and not the BMSC secretome.185 In a murine model of phorbol-12-myristate-13-acetate-induced dermatitis, administration of mouse ADSCs at the site of dermatitis significantly dampened the neutrophil oxidative burst, protecting the tissue from damage by releasing antioxidants.186 Similarly, using exosomes from ADSCs, motoneurons were protected from oxidative stress.187
Tissue sources for the collection of ADSCs might be important to the ADSC phenotype, where the tissue depot, skin versus abdomen, and health status of the donor can impart some variation to the ADSCs and their secretome. For example, ADSCs sourced from humans with obesity compared to those from normal-weight individuals secrete a more proinflammatory cytokine profile.188 Peng et al189 showed that ADSCs directly interact with dendritic cells, inducing a dendritic cell phenotype that allows immune tolerance and inhibits the polarization of naïve T-cells into proinflammatory Th1 cells. Furthermore, Ivanova-Todorova et al190 discovered that ADSCs are more potent suppressors of dendritic cell differentiation than BMSCs. Ribeiro et al191 compared the ability of ADSCs and BMSCs to suppress peripheral blood B-, T- and NK cells. Their results showed that ADSCs had a stronger inhibitory effect than did BMSCs, yielding a greater proportion of T-cells in the nonactivated state. Regulation of the T-cell phenotype in the skin is important beyond just consideration of inflammation because, for example, Ali et al192 found that Treg cells are involved in stem cell activation in the hair follicle, making them important for hair growth and wound healing.193 Rybalko et al194 showed that dual injections of macrophages and ADSCs can be used as an intervention in the treatment of critical ischemia. Local injection of both cell types leads to accelerated recovery of muscle function and histopathology, reduced inflammation, and improved perfusion of the regenerating ischemic limb. They also presented evidence that ADSCs are powerful modulators of macrophage functional status as evidenced by the upregulation of CD206 and gene profiling, useful as an endogenous or exogenous anti-inflammatory macrophage phenotype for regenerative medicine.195 Given the ability of ADSCs to drive the M2 macrophage phenotype, shown to downregulate proinflammatory stimulation by releasing anti-inflammatory cytokines and antagonizing M1 macrophage responses in wounds,196 ADSCs are considered to be proresolving in their actions during an inflammatory state.197 The proresolving mechanisms of ADSCs include inducing M2 macrophages to secrete growth factors that activate epithelial cells and facilitate fibroblast differentiation into myofibroblasts.198 M2 macrophages also promote extracellular matrix turnover, clear apoptotic/necrotic cells, debris, and tissue-damaging extracellular matrix components and orchestrate TH2- and regulatory T-cell migration to the wound side,199 thus controlling, for example, autoimmunity. Systemic administration of ADSC-conditioned media significantly attenuated lipopolysaccharide-induced bone loss by reducing serum levels of proinflammatory cytokines. The beneficial effect of ADSC-conditioned media was partly mediated by regulating the function of macrophages during inflammatory processes.200 ADSCs can also fight infection by the release of antimicrobial peptides (AMPs), such as cathelicidin, that control chronic bacterial infections.201 ADSCs have been shown to provide superior antibacterial effectiveness than do BMSCs, an effect found to be at least partially mediated by the LL-37 AMP.202 AMPs are an effective and safe means to fight bacterial, viral, and fungal infections because they are not toxic to the host’s cells203 and can block proinflammatory macrophage responses.204
Another important quality of ADSCs is their robustness as they age compared to BMSCs. ADSC cultures retained their normal diploid (2n) karyotype better than did BMSCs, up to passage 20 for human BMSCs and passage 30 for human ADSCs.205 Further, as MSCs double in culture, ADSCs are less inclined to express the senescent phenotype than BMSCs.117 Subcutaneous native adipose tissue was not affected by the donor’s age in terms of cellular senescence and yield of ADSCs from donors. Also, a constant mRNA level of osteocalcin and alkaline phosphatase with a similar level of matrix mineralization of ADSCs remained unaffected by donor age after osteogenic differentiation. The secretome of ADSCs was similarly unaffected by age when used to promote angiogenesis.206 Further, measuring the senescent state in BMSCs versus ADSCs from the same donors, Wu et al207 showed that ADSCs were less senescent, an aged phenotype, and were better able to restore cardiac function and induce angiogenesis than matched BMSCs from older patients were able to. However, in the laboratory setting, cultured ADSCs that have reached replicative senescence and have been preconditioned with IL-2 might have been induced into a phenotype not warranted for therapeutic use.208 In a within-subjects comparison of human ADSCs, there was no reduction in tridifferentiation viability when measured at ages 12 years apart.209 In contrast, BMSCs lose viability as they age,210 with, for example, a significantly reduced ability to repair ischemic tissue as they age.211 Likewise, cryopreserved BMSCs have more limited expansion capability and are more senescent than are cryopreserved ADSCs.212 The exosomes contained in the secretome of BMSCs have significant age-dependent differences in their immune profiles, including more proinflammatory microRNAs.213 Thus, although phenotypic variation, including age of the stem cells, is important for therapeutic development in all stem cells, BMSCs are more negatively affected by age, doubling number, and other factors than are ADSCs.
We must also remember that the bone marrow is a site of great stem cell homing, both from the bone marrow to other regions of the body and from other parts of the body back to the bone marrow, including cancerous stem cells that return to the bone marrow and engraft there.214 Not only can BMSCs and their secreted molecules induce cancer,215 including melanoma,60 but they can also transfer cancer from the donor to the recipient,216 including by the exosomes of the BMSCs.217 This happens despite careful screening of BMSCs, because cancerous BMSCs and other cancer stem cells recirculate to the bone marrow and engraft there,214 remaining dormant and undetected for years.218 Therefore, migration of adult stem cells, including cancerous phenotypes, occurs not only to and from the bone marrow, but also within the bone marrow.219 Thus, if BMSCs are being used to generate cytokines for the development of skin care products, the use of cytokines from cancerous BMSCs is a possibility. Moreover, because stem cells from many parts of the body home to bone marrow and engraft there,220 stem cells carrying any sort of injury signal incurred in that part of the body suffering injury, where a state of repurposing of fetal development genetic programs might be switched on in adult stems cells,221 might be present in the bone marrow. Such cells in the bone marrow might possess the proliferative, cancer-like phenotype,82 potentially leading to cancer in the body as the BMSCs are recruited to fight infection and regenerate tissue at sites of injury.222 Malignant cells in the bone marrow alter the phenotype of surrounding stromal cells to express key niche factors such as CXCL12 and Jagged1 that, in turn, promote malignant hematopoietic cell growth.223 The cytokines released from the BMSC cancer phenotype might contribute to the pathogenesis of cancer, as demonstrated in chronic myelomonocytic leukemia patients224 and acute myeloid leukemia,225 through altered cytokine secretion.
Furthermore, because T-cells from various areas of the body migrate to the bone marrow, cytotoxic CD8+ T-cell phenotypes generated during infection can induce BMSCs to release a proinflammatory set of cytokines, including IL-6.226 Thus, using the cytokines from BMSCs in a skin care product might include proinflammatory cytokines that have been sourced from BMSCs stimulated by cytotoxic CD8+ T cells, therefore inducing inflammation when applied to the skin. IL-6 is associated with chronic inflammatory states and is a direct regulator of breast cancer stem cell self-renewal,227 additionally promoting metastasis of hepatocellular carcinoma.170
Conclusion
Considering the many molecular components of the secretome and the actions of those many molecules within defined biochemical pathways in a number of target cells in the skin, the secretome from ADSCs and fibroblasts provide a safe and efficacious means for therapeutic development. In contrast, significant health problems can result from using blood-derived cells and their secretome, namely platelets and BMSCs. Therefore, although the secretome from BMSCs is efficacious in driving a classic M1 inflammatory response and cellular proliferation, the BMSCs and their secretome might only have a place in the development of products for short-term use in treating the initial healing phase of wounds with severe infection. Given the many risks posed in the use of BMSCs, including for the approved treatment of blood diseases,108 and that ADSCs have been shown as safe107 and effective in ameliorating some of the adverse events associated with bone marrow transplants for blood diseases228 and given the potential of ADSCs to differentiate into blood cells229 or aid in the differentiation of BMSCs into blood cells,230 ADSCS might one day even supplant the transplant of BMSCs for leukemia and other blood diseases, in addition to their optimal use in developing skin care products and in performing dermatological procedures.
References
- United States Food and Drug Administration. Surgical biologics—untitled letter. Available at https://www.fda.gov/BiologicsBloodVaccines/GuidanceComplianceRegulatoryInformation/ComplianceActivities/Enforcement/UntitledLetters/ucm367184.htm. Accessed July 31, 2019.
- Proksch E. Altershaut und Hautpflege. Zeitschrift für Gerontologie und Geriatrie. 2015;48:325–330.
- Sen CK, Gordillo GM, Roy S, et al. Human skin wounds: a major and snowballing threat to public health and the economy. Wound Repair Regen. 2009;17(6):763–771.
- Donati G, Rognoni E, Hiratsuka T, et al. Wounding induces dedifferentiation of epidermal Gata6+ cells and acquisition of stem cell properties’. Nat Cell Biol. 2017;19(6):603-613.
- Tapia N, Scholer HR. Molecular obstacles to clinical translation of iPSCs. Cell Stem Cell. 2016;19(3):298–309.
- Liang G, Zhang Y. Genetic and epigenetic variations in iPSCs: potential causes and implications for application. Cell Stem Cell. 2013;13(2):149–159.
- Lister R, Pelizzola M, Kida YS et al. Hotspots of aberrant epigenomic reprogramming in human induced pluripotent stem cells. Nature. 2011;471(7336):68–73.
- Rosner M, Pham HTT, Moriggl R, Hengstschläger M, et al. Human stem cells alter the invasive properties of somatic cells via paracrine activation of mTORC1. Nat Commun. 2017;8(1):595.
- Leuning DG, Beijer NRM, du Fossé NA, et al. The cytokine secretion profile of mesenchymal stromal cells is determined by surface structure of the microenvironment. Sci Rep. 2018;8(1):7716.
- Rayahin JE, Buhrman JS, Zhang Y, et al. High and low molecular weight hyaluronic acid differentially influence macrophage activation. ACS Biomater Sci Eng. 2015;1(7):481–493
- Jiang L, Liu G, Liu H, et al. Molecular weight impact on the mechanical forces between hyaluronan and its receptor. Carbohydr Polym. 2018;97:326–336.
- Rilla K, Mustonen AM, Arasu UT, et al. Extracellular vesicles are integral and functional components of the extracellular matrix. Matrix Biology. 2017;75–76:201–219.
- Huleihel L, Hussey GS, Naranjo JD, et al. Matrix-bound nanovesicles within ECM bioscaffolds. Sci Adv. 2016;2(6):e1600502.
- Costa-Almeida R, Soares R, Granja PL. Fibroblasts as maestros orchestrating tissue regeneration. J Tissue Eng Regen Med. 2018;12(1):240–251.
- Kirsner RS, Marston WA, Snyder RJ, et al. Spray-applied cell therapy with human allogeneic fibroblasts and keratinocytes for the treatment of chronic venous leg ulcers: a phase 2, multicentre, double-blind, randomised, placebo-controlled trial. Lancet. 2012;380(9846):977–985.
- Wong T, Gammon L, Liu L, et al. Potential of fibroblast cell therapy for recessive dystrophic epidermolysis bullosa. J Invest Dermatol. 2008;128(9):2179–2189.
- Maarof M, Mh Busra MF, Lokanathan Y, et al. Safety and efficacy of dermal fibroblast conditioned medium (DFCM) fortified collagen hydrogel as acellular 3D skin patch. Drug Deliv Transl Res. 2019;9(1):144–161.
- Hunefeld C, Mezger M, Müller-Hermelink E, et al. Bone marrow-derived stem cells migrate into intraepidermal skin defects of a desmoglein-3 knockout mouse model but preserve their mesodermal differentiation. J Invest Dermatol. 2018;138(5):1157–1165.
- Mehta RC, Smith SR, Grove GL, et al. Reduction in facial photodamage by a topical growth factor product. J Drugs Dermatol. 2008;7(9):864–871.
- Chang HY, Chi JT, Dudoit S, et al. Diversity, topographic differentiation, and positional memory in human fibroblasts. Proc Natl Acad Sci U S A. 2002;99(20):12877–12882.
- Wang L, Hu L, Zhou X, et al. Exosomes secreted by human adipose mesenchymal stem cells promote scarless cutaneous repair by regulating extracellular matrix remodeling. Sci Rep. 2017;7:13321.
- Fry CS, Kirby TJ, Kosmac K, et al. Myogenic progenitor cells control extracellular matrix production by fibroblasts during skeletal muscle hypertrophy. Cell Stem Cell. 2017;20(1):56–69.
- Chicharro D, Carrillo JM, Rubio M, et al. Combined plasma rich in growth factors and adipose-derived mesenchymal stem cells promotes the cutaneous wound healing in rabbits. BMC Vet Res. 2018;14(1):288.
- Hu L, Wang J, Zhou X, et al. Exosomes derived from human adipose mensenchymal stem cells accelerates cutaneous wound healing via optimizing the characteristics of fibroblasts. Sci Rep. 2015;6:32993.
- Jun JI, Lau F. The matricellular protein CCN1 induces fibroblast senescence and restricts fibrosis in cutaneous wound healing. Nat Cell Biol. 2010:12(7):676–685.
- Kalluri R. The biology and function of fibroblasts in cancer. Nat Rev Cancer. 2016;16(9):582–598.
- Alexander J, Cukierman E. Stromal dynamic reciprocity in cancer: intricacies of fibroblastic-ECM interactions. Curr Opin Cell Biol. 2016;42:80–93.
- Wen S, Niu Y, Yeh S, Chang C. BM-MSCs promote prostate cancer progression via the conversion of normal fibroblasts to cancer-associated fibroblasts. Int J Oncol. 2015;47(2):719–727.
- Augsten M. Cancer-associated fibroblasts as another polarized cell type of the tumor microenvironment. Front Oncol. 2014;4:62.
- Mine S, Fortunel NO, Pageon H, Asselineau D. Aging alters functionally human dermal papillary fibroblasts but not reticular fibroblasts: a new view of skin morphogenesis and aging. PLoS One. 2008;3(12):e4066.
- Coppe JP, Patil CK, Rodier F, et al. A human-like senescence-associated secretory phenotype is conserved in mouse cells dependent on physiological oxygen. PLoS One. 2010;5(2):e9188.
- Kim M, Kim SM, Kwon S, et al. Senescent fibroblasts in melasma pathophysiology. Exp Dermatol. 2019;28(6):719–722.
- Salzar MC, Lafzi A, Berenguer-Llergo A, et al. Identity noise and adipogenic traits characterize dermal fibroblast aging. Cell. 2018;175(6): 1575–1590.
- Aldag C, Teixeira DN, Leventhal PS. Skin rejuvenation using cosmetic products containing growth factors, cytokines, and matrikines: a review of the literature. Clin Cosmet Investig Dermatol. 2016;9:411–419.
- Ulivi V Tasso R, Cancedda R, Descalzi F. Mesenchymal stem cell paracrine activity is modulated by platelet lysate: induction of an inflammatory response and secretion of factors maintaining macrophages in a proinflammatory phenotype. Stem Cells Dev. 2014;23(16): 1858–1869.
- Shook BA, Wasko RR, Rivera-Gonzalez GC, et al. Myofibroblast proliferation and heterogeneity are supported by macrophages during skin repair. Science. 2018;362(6417). pii: eaar2971.
- Pierre S, Linke B, Jing S, et al. GPVI and thromboxane receptor on platelets promote proinflammatory macrophage phenotypes during cutaneous inflammation. J Invest Dermatol. 2017;137(3):686–695.
- Wang Y, Sun Y, Yang XY, et al. Mobilised bone marrow-derived cells accelerate wound healing. Int Wound J. 2013;10(4):473–479.
- Jenkins SJ, Ruckerl D, Cook PC, et al. Local macrophage proliferation, rather than recruitment from the blood, is a signature of TH2 inflammation. Science. 2011;332(6035): 1284–1288.
- Badiavas EV, Abedi M, Butmarc J, et al. Participation of bone marrow derived cells in cutaneous wound healing. J Cell Physiol. 2003;196(2):245–250.
- Sasaki M, Abe R, Fujita Y, et al. Mesenchymal stem cells are recruited into wounded skin and contribute to wound repair by transdifferentiation into multiple skin cell type. J Immunol. 2008;180(4):2581–2587.
- de Oliveira S, Rosowski EE, Huttenlocher A. Neutrophil migration in infection and wound repair: going forward in reverse. Nat Rev Immunol. 2016;16(6):378–391.
- Casatella MA, Mosna F, Micheletti A, et al. Toll-like receptor-3-activated human mesenchymal stromal cells significantly prolong the survival and function of neutrophils. Stem Cells. 2011;29(6):1001–1011.
- Davies LC, Jenkins SJ, Allen JE, Taylor PR. Tissue-resident macrophages. Nat Immunol. 2013;14(10):986–995.
- Faulknor RA, Olekson MA, Ekwueme EC, et al. Hypoxia impairs mesenchymal stromal cell-induced macrophage M1 to M2 transition. Technology (Singap World Sci). 2017;5(2):81–86.
- Waterman RS, Tomchuck SL, Henkle SL, Betancourt AM. A new mesenchymal stem cell (MSC) paradigm: polarization into a proinflammatory MSC1 or an immunosuppressive MSC2 phenotype. PLoS ONE. 2010;5(4):e10088.
- Zeng X, Guo R, Dong M, et al. Contribution of TLR4 signaling in intermittent hypoxia-mediated atherosclerosis progression. J Transl Med. 2018;16(1):106.
- Waterman RS, Henkle SL, Betancourt AM. Mesenchymal stem cell 1 (MSC1)-based therapy attenuates tumor growth whereas MSC2-treatment promotes tumor growth and metastasis. PLoS One. 2012;7(9):e45590.
- Dardenne AD, Wulff, BC, Wilgus TA. The alarmin HMGB-1 influences healing outcomes in fetal skin wounds. Wound Repair Regen. 2013;21(2): 282–291.
- Tan MY, Zhang CD, Xia B, et al. The expression of HMGB1 in bone marrow MSCs Is upregulated by hypoxia with regulatory effects on the apoptosis and adhesion. Biomed Res Int. 2016;2016:4598927.
- Yasinska IM, Gonçalves Silva I, Sakhnevych SS, et al. High mobility group box 1 (HMGB1) acts as an “alarmin” to promote acute myeloid leukaemia progression. Oncoimmunology. 2018;7(6):e1438109.
- Yaghooti H, Mohammadtaghvaei N, Mahboobnia K. Effects of palmitate and astaxanthin on cell viability and proinflammatory characteristics of mesenchymal stem cells. Int Immunopharmacol. 2019;68:164–170.
- Sukho P, Hesselink JW, Kops N, et al. Human mesenchymal stromal cell sheets induce macrophages predominantly to an anti-inflammatory phenotype. Stem Cells Dev. 2018;27(13):922–934.
- Kalinina N, Kharlampieva D, Loguinova M, et al. Characterization of secretomes provides evidence for adipose-derived mesenchymal stromal cells subtypes. Stem Cell Res Ther. 2015;6:221.
- Ponte AL, Marais E, Gallay N, et al. The in vitro migration capacity of human bone marrow mesenchymal stem cells: comparison of chemokine and growth factor chemotactic activities. Stem Cells. 2007;25(7):1737.
- Rauner M, Stein N, Winzer M, et al. WNT5A is induced by inflammatory mediators in bone marrow stromal cells and regulates cytokine and chemokine production. J Bone Miner Res. 2012;27(3):575–585.
- Asem MS, Buechler S, Wates RB, et al. Wnt5a signaling in cancer. Cancers (Basel). 2016;8(9). pii: E79.
- Ekstrom EJ, Bergenfelz C , von Bülow V, et al. WNT5A induces release of exosomes containing pro-angiogenic and immunosuppressive factors from malignant melanoma cells. Mol Cancer. 2014;13:88.
- Christopher MJ, Petti AA, Rettig MP, et al. Immune escape of relapsed AML cells after allogeneic transplantation. N Engl J Med. 2018;379(24):2330–2341.
- Omland SH, Gniadecki R, Hædersdal M et al. Skin cancer risk in hematopoietic stem-cell transplant recipients compared with background population and renal transplant recipients: a population-based cohort study. JAMA Dermatol. 2016;152(2):177–183.
- Liu S, Ginestier C, Ou SJ, et al. Breast cancer stem cells are regulated by mesenchymal stem cells through cytokine networks. Cancer Res. 2011;71(2):614–624.
- Farahmand L, Esmaeili R, Eini L, Majidzadeh AK. The effect of mesenchymal stem cell-conditioned medium on proliferation and apoptosis of breast cancer cell line. J Cancer Res Ther. 2018;14(2): 341–344.
- Zhang T, Lee YW, Rui YF, et al. Bone marrow-derived mesenchymal stem cells promote growth and angiogenesis of breast and prostate tumors. Stem Cell Res Ther. 2013;4(3):70.
- Chen B, Yu J, Wang Q, et al. Human bone marrow mesenchymal stem cells promote gastric cancer growth via regulating c-Myc. Stem Cells Int. 2018;2018:9501747.
- Zhu W, Huang L, Li Y, et al. Exosomes derived from human bone marrow mesenchymal stem cells promote tumor growth in vivo. Cancer Lett. 2012;315(1):28–37.
- Karnoub AE, Dash AB, Vo AP, Sullivan A, et al. Mesenchymal stem cells within tumour stroma promote breast cancer metastasis. Nature. 2007;449(7162):557–563.
- Luo J, Ok Lee S, Liang L, et al. Infiltrating bone marrow mesenchymal stem cells increase prostate cancer stem cell population and metastatic ability via secreting cytokines to suppress androgen receptor signaling. Oncogene. 2014;33(21): 2768–2778.
- Ruffini PA. The CXCL8-CXCR1/2 Axis as a therapeutic target in breast cancer stem-like cells. Front Oncol. 2019;9:40.
- Yu PF, Huang Y, Han YY, et al. TNF-alpha-activated mesenchymal stromal cells promote breast cancer metastasis by recruiting CXCR2+ neutrophils. Oncogene. 2016;36(4):482–490.
- Ye H, Cheng J, Tang Y, et al. Human bone marrow-derived mesenchymal stem cells produced TGFbeta contributes to progression and metastasis of prostate cancer. Cancer Invest. 2012;30(7): 513–518.
- Vallabhaneni KC, Penfornis P, Dhule S, et al. Extracellular vesicles from bone marrow mesenchymal stem/stromal cells transport tumor regulatory microRNA, proteins, and metabolites. Oncotarget. 2015;6(7):4953–4967.
- Wang Q, Li Z, Sun L et al. Platelets enhance the ability of bone-marrow mesenchymal stem cells to promote cancer metastasis. Onco Targets Ther. 2018;11:8251–8263.
- Sun B, Roh KH, Park JR, et al. Therapeutic potential of mesenchymal stromal cells in a mouse breast cancer metastasis model. Cytotherapy. 2009;11(3):289–298.
- Chen L, Tredget EE, Wu PY, Wu Y. Paracrine factors of mesenchymal stem cells recruit macrophages and endothelial lineage cells and enhance wound healing. PLoS One. 2008;3(4):e1886.
- Renehan AG, Zwahlen M, Minder C, O’Dwyer ST. Insulin-like growth factor (IGF)-I, IGF binding protein-3, and cancer risk: systematic review and meta-regression analysis. Lancet. 2004;363(9418):1346–1347.
- Kaaks R, Johnson T, Tikk K, et al. Insulin-like growth factor I and risk of breast cancer by age and hormone receptor status—a prospective study within the EPIC cohort. Int J Cancer. 2014;134(11):2683–2690.
- Key TJ, Appleby PN, Reeves GK, Roddam AW. Insulin-like growth factor 1 (IGF1), IGF binding protein 3 (IGFBP3), and breast cancer risk: pooled individual data analysis of 17 prospective studies. Lancet Oncol. 2010;11(6):530–542.
- Ono M, Kosaka N, Tominaga N, et al. Exosomes from bone marrow mesenchymal stem cells contain a microRNA that promotes dormancy in metastatic breast cancer cells. Sci Signal. 2014;7(332):ra63.
- Marx V. How to pull the blanket off dormant cancer cells. Nat Methods. 2018;15(4):249–252.
- Seppanen E, Roy E, Ellis R, Bou-Gharios G, et al. Distant mesenchymal progenitors contribute to skin wound healing and produce collagen: evidence from a murine fetal microchimerism model. PLoS ONE. 2013;8(5):e62662.
- Naik S, Larsen SB, Gomez NC et al. Inflammatory memory sensitizes skin epithelial stem cells to tissue damage. Nature. 2017;550(7677):475–480.
- Mukherjee S, Chen LY, Papadimos TJ, et al. Lipopolysaccharide-driven Th2 cytokine production in macrophages is regulated by both MyD88 and TRAM. J Biol Chem. 2009;284(43):29391–29398.
- Van Dyken SJ, Locksley RM. Interleukin-4- and interleukin-13-mediated alternatively activated macrophages: roles in homeostasis and disease. Annu Rev Immunol. 2013;31:317–343.
- Kodera T, McGaha TL, Phelps R, et al. Disrupting the IL-4 gene rescues mice homozygous for the tight-skin mutation from embryonic death and diminishes TGF-alpha production by fibroblasts. Proc Natl Acad Sci U S A. 2002;99(6):3800–3805.
- Smith AN, Willis E, Chan VT, et al. Mesenchymal stem cells induce dermal fibroblast responses to injury. Exp Cell Res. 2010;316(1):48–54.
- Maguire G, Friedman P. Systems biology approach to developing S(2)RM-based “systems therapeutics” and naturally induced pluripotent stem cells. World J Stem Cells. 2015;7(4):745–756.
- Williams G, Zentar MP, Gajendra S, et al. Transcriptional basis for the inhibition of neural stem cell proliferation and migration by the TGF-alpha-family member GDF11. PLoS One. 2013;8(11):e78478.
- Flach J, Bakker ST, Mohrin M, et al. Replication stress is a potent driver of functional decline in ageing haematopoietic stem cells. Nature. 2014;512(7513):198–202.
- Dvorak HF. Tumors: wounds that do not heal. Similarities between tumor stroma generation and wound healing. N Engl J Med. 1985;315(26):1650–1659.
- DerHagopian RP, Sugarbaker EV, Ketcham A. Inflammatory oncotaxis. JAMA. 1978;240(4): 374–375.
- Cooley LD, Sears DA, Udden MA et al. Donor cell leukemia: report of a case occurring 11 years after allogeneic bone marrow transplantation and review of the literature. Am J Hematol. 2000;63(1):46–53.
- Cousin B, Ravet E, Poglio S, et al. Adult stromal cells derived from human adipose tissue provoke pancreatic cancer cell death both in vitro and in vivo. PLoS One. 2009;4(7):e6278.
- Illouz YG. Breast cancer treatment by adipose-derived stem cells: an experimental study. J Stem Cells. 2014;9(4):211–217.
- Ko SF, Yip HK, Zhen YY, et al. Adipose-derived mesenchymal stem cell exosomes suppress hepatocellular carcinoma growth in a rat model: apparent diffusion coefficient, natural killer T-cell responses, and histopathological features. Stem Cells Int. 2015;2015:853506.
- Wang J. Bone marrow-derived mesenchymal stem cell-secreted IL-8 promotes the angiogenesis and growth of colorectal cancer. Oncotarget. 2015;6(40):42825–42837.
- Schneider RK, Mullally A, Dugourd A, et al. Gli1+ mesenchymal stromal cells are a key driver of bone marrow fibrosis and an important cellular therapeutic target. Cell Stem Cell. 2017;20(6):785–800.e8.
- Jain P, Perakath B, Jesudason MR, Nayak S. The effects of bone marrow derived cells on healing chronic lower extremity wounds: results of a randomized control study. Ostomy Wound Manage. 2011;57(7):38–44.
- Mehdipour F, Razmkhah M, Rezaeifard S, et al. Mesenchymal stem cells induced anti-inflammatory features in B cells from breast tumor draining lymph nodes. Cell Biol Int. 2018;42(12):1658–1669.
- Wood WA, Krishnamurthy J, Mitin N, et al. Chemotherapy and stem cell transplantation increase p16INK4a expression, a biomarker of T-cell aging. EBioMedicine. 2016;11:227–238.
- Villada G, Roujeau JC, Cordonnier C, et al. Toxic epidermal necrolysis after bone marrow transplantation: study of nine cases. J Am Acad Dermatol. 1990;23(5):870–875.
- Macedo FI, Faris J, Lum LG, et al. Extensive toxic epidermal necrolysis versus acute graft versus host disease after allogenic hematopoietic stem-cell transplantation: challenges in diagnosis and management. J Burn Care Res. 2014;35(6): e431–e435.
- Kinoshita Y, Saeki H. A review of the pathogenesis of toxic epidermal necrolysis. J Nippon Med Sch. 2016;83(6):216–222.
- Thomas H, Jäger M, Mauel K, et al. Interaction with mesenchymal stem cells provokes natural killer cells for enhanced IL-12/IL-18-induced interferon-gamma secretion. Mediators Inflamm. 2014;2014:143463.
- Hashimoto N, Jin H, Liu T, et al. Bone marrow-derived progenitor cells in pulmonary fibrosis. J Clin Invest. 2004;113(2):243–252.
- Andersson-Sjöland A, de Alba CG, Nihlberg K, et al. Fibrocytes are a potential source of lung fibroblasts in idiopathic pulmonary fibrosis. Int J Biochem Cell Biol. 2008;40(10):2129–2140.
- Kuo MC Kothari AN, Kuo PC, Mi Z. Cancer stemness in bone marrow micrometastases of human breast cancer. Surgery. 2018;163(2):330–335.
- García-Contreras M, Vera-Donoso CD, Hernández-Andreu JM, et al. Therapeutic potential of human adipose-derived stem cells (ADSCs) from cancer patients: a pilot study. PLoS One. 2014;9(11):e113288.
- Maguire G. Transplanted stem cells survive a long time—do they make you sick?. J Roy Soc Med. In Press.
- Kim WS, Park BS, Park SH, et al. Antiwrinkle effect of adipose-derived stem cell: activation of dermal fibroblast by secretory factors. J Dermatol Sci. 2009;53(2):96–102.
- Zhang S, Dong Z, Peng Z, Lu F. Antiaging effect of adipose-derived stem cells in a mouse model of skin aging induced by D-galactose. PLoS One. 2014;9(5):e97573.
- Tomaszewski CE, Constance E, Lemke MM, et al. Adipose-derived stem cell-secreted factors promote early stage follicle development in a biomimetic matrix. Biomater Sci. 2019;7(2): 571–580.
- Chu GY, Chen YF, Chen HY, et al. Stem cell therapy on skin: mechanisms, recent advances and drug reviewing issues. J Food Drug Anal. 2018;26(1):14–20.
- Schmidt BA, Horsley V. Intradermal adipocytes mediate fibroblast recruitment during skin wound healing. Development. 2013;140(7):1517–1527.
- Kim M, Kim I, Lee SK, et al. Clinical trial of autologous differentiated adipocytes from stem cells derived from human adipose tissue. Dermatol Surg. 2011;37(6):750–759.
- Chen L, Wang ZC, Ma JJ, et al. Autologous nanofat transplantation accelerates foot wound healing in diabetic rats. Regen Med. 2019;14(3):231–241.
- Tonnard P, Verpaele A, Peeters G, et al. Nanofat grafting: basic research and clinical applications. Plast Reconstr Surg. 2013;132(4):1017–1026.
- Kern S, Eichler H, Stoeve J, et al. Comparative analysis of mesenchymal stem cells from bone marrow, umbilical cord blood, or adipose tissue. Stem Cells. 24(5):1294–301.
- Li Q, Sun W, Wang X, et al. Skin-derived mesenchymal stem cells alleviate atherosclerosis via modulating macrophage function. Stem Cells Transl Med. 2015;4(11):1294–301.
- Li M, Xu J, Mei X et al. Regulatory effects of dermal papillary pluripotent stem cells on polarization of macrophages from M1 to M2 phenotype in vitro. Transpl Immunol. 2019;52:57–67.
- Ke F, Zhang L, Liu Z, et al. Autocrine interleukin-6 drives skin-derived mesenchymal stem cell trafficking via regulating voltage-gated Ca(2+) channels. Stem Cells. 2014;32(10):2799–2810.
- Li M, Mei X, Lv S, et al. Rat vibrissa dermal papilla cells promote healing of spinal cord injury following transplantation. Exp Ther Med. 2018;15(4):3929–3939.
- Rodrigues C, de Assis AM, Moura DJ, et al. New therapy of skin repair combining adipose-derived mesenchymal stem cells with sodium carboxymethylcellulose scaffold in a pre-clinical rat model. PLoS One. 2014;9(5):e96241.
- Akita S, Akino K, Hirano A, et al. Noncultured autologous adipose-derived stem cells therapy for chronic radiation injury. Stem Cells Int. 2010;2010:532704.
- Xiao S, Liu Z, Yao Y, et al. Diabetic human adipose-derived stem cells accelerate pressure ulcer-healing by inducing angiogenesis and neurogenesis. Stem Cells Dev. 2019;28(5): 319–328.
- Muhammad G, Xu J, Bulte JWM, et al. Transplanted adipose-derived stem cells can be short-lived yet accelerate healing of acid-burn skin wounds: a multimodal imaging study. Sci Rep. 2017;7(1):4644.
- Park HS, Son HY, Choi MH, et al. Adipose-derived stem cells attenuate atopic dermatitis-like skin lesions in NC/Nga mice. Exp Dermatol. 2019;28(3):300–307.
- Mei S, Wang S, Jin S, et al. Human adipose tissue-derived stromal cells attenuate the multiple organ injuries induced by sepsis and mechanical ventilation in mice. Inflammation. 2019;42(2):485–495.
- Gong JH Dong JY, Xie T, Lu SL. The Influence of AGEs environment on proliferation, apoptosis, homeostasis, and endothelial cell differentiation of human adipose stem cells. Int J Low Extrem Wounds. 2017;16(2):94–103.
- Pelizzo G, Avanzini MA, Icaro Cornaglia A, et al. Mesenchymal stromal cells for cutaneous wound healing in a rabbit model: pre-clinical study applicable in the pediatric surgical setting. J Transl Med. 2015;13(1):219.
- Riis S, Stensballe A, Emmersen J, et al. Mass spectrometry analysis of adipose-derived stem cells reveals a significant effect of hypoxia on pathways regulating extracellular matrix. Stem Cell Res Ther. 2016;7(1):52.
- Ren S, Chen J, Duscher D, et al. Microvesicles from human adipose stem cells promote wound healing by optimizing cellular functions via AKT and ERK signaling pathways. Stem Cell Res Ther. 2019;10(1):47.
- Lee SH, Jin SY, Song JS, et al. Paracrine effects of adipose-derived stem cells on keratinocytes and dermal fibroblasts. Ann Dermatol. 2012;24(2):136–143.
- Diegelmann RF, Evans MC. Wound healing: an overview of acute, fibrotic and delayed healing. Front Biosci. 2004;9:283–289.
- Cerny MK, Hopfner U, Kirsch M, et al. Occlusive dressing-induced secretomes influence the migration and proliferation of mesenchymal stem cells and fibroblasts differently. Eur J Med Res. 2018;23(1):60.
- Heinrichs D, Knauel M, Offermanns C, et al. Macrophage migration inhibitory factor (MIF) exerts antifibrotic effects in experimental liver fibrosis via CD74. Proc Natl Acad Sci U S A. 2011;108(42):17444–17449.
- Nahar S, Nakashima Y, Miyagi-Shiohira C, et al. Cytokines in adipose-derived mesenchymal stem cells promote the healing of liver disease. World J Stem Cells. 2018;10(11):146–159.
- Yamato M, Sakai Y, Mochida H et al. Adipose tissue-derived stem cells prevent fibrosis in murine steatohepatitis by suppressing IL-17-mediated inflammation. J Gastroenterol Hepatol. 2019 Mar 3. [Epub ahead of print].
- Shan X, Choi JH, Kim KJ, et al. Adipose stem cells with conditioned media for treatment of acne vulgaris scar. Tissue Eng Regen Med. 2018;15(1):49–61.
- Zhou BR, Xu Y, Guo SL, et al. The effect of conditioned media of adipose-derived stem cells on wound healing after ablative fractional carbon dioxide laser resurfacing. Biomed Res Int. 2013;2013:519126.
- Martínez ML, Escario E, Poblet E, et al. Hair follicle–containing punch grafts accelerate chronic ulcer healing: a randomized controlled trial. J Am Acad Dermatol. 2016;75(5):1007–1014.
- Manferdini C, Paolella F, Gabusi E, et al. Adipose stromal cells mediated switching of the proinflammatory profile of M1-like macrophages is facilitated by PGE2: in vitro evaluation. Osteoarthritis Cartilage. 2017;25(7):1161–1171.
- Mosser, DM, Edwards, JP. Exploring the full spectrum of macrophage activation. Nat Rev Immunol. 2008;8(12):958–969.
- Ylostalo JH, Bartosh TJ, Coble K, Prockop DJ. Human mesenchymal stem/stromal cells cultured as spheroids are self-activated to produce prostaglandin E2 that directs stimulated macrophages into an anti-inflammatory phenotype. Stem Cells. 2012;30(10):2283–2296.
- Hu Y, Qin C, Zhenget G, et al. Mesenchymal stem cell-educated macrophages ameliorate LPS-induced systemic response. Mediators Inflamm. 2016:3735452.
- Song WJ, Li Q, Ryu MO, et al. TSG-6 secreted by human adipose tissue-derived mesenchymal stem Cells ameliorates DSS-induced colitis by inducing M2 macrophage polarization in mice. Sci Rep. 2017;7(1):5187.
- Shang Q, Bai Y, Wang G, et al. Delivery of adipose-derived stem cells attenuates adipose tissue inflammation and insulin resistance in obese mice through remodeling macrophage phenotypes. Stem Cells Dev. 2015;24(17):2052–2064.
- Takafuji Y, Hori M, Mizuno T, Harada-Shiba M. Humoral factors secreted from adipose tissue-derived mesenchymal stem cells ameliorate atherosclerosis in Ldlr-/- mice. Cardiovasc Res. 2019;115(6):1041–1051.
- Son WC, Yun JW, Kim BH. Adipose-derived mesenchymal stem cells reduce MMP-1 expression in UV-irradiated human dermal fibroblasts: therapeutic potential in skin wrinkling. Biosci Biotechnol Biochem. 2015;79(6):919–925.
- Kim WS, Park BS, Sung JH. The wound-healing and antioxidant effects of adipose-derived stem cells. Expert Opin Biol Ther. 2009;9(7):879–887.
- Mohammed SA, El Salam NFA, Kalleny NK et al. Effect of adipose-derived stem cells on induced photoaging in the skin of adult Guinea pig: histological and immunohistochemical study. Egyptian J Histology. 2017;40(2):184–200.
- Wang T, Guo S, Liu X et al. Protective effects of adipose-derived stem cells secretome on human dermal fibroblasts from ageing damages. Int J Clin Exp Pathol. 2015;8(12):15739–15748.
- Kim DW, Jeon BJ, Hwang NH, et al. Adipose-derived stem cells inhibit epidermal melanocytes through an interleukin-6-mediated mechanism. Plast Reconstr Surg. 2014;134(3):470–480.
- Niada S, Giannasi C, Gualerzi A, et al. Differential proteomic analysis predicts appropriate applications for the secretome of adipose-derived mesenchymal stem/stromal cells and dermal fibroblasts. Stem Cells Int. 2018;2018:7309031.
- Maguire G, Paler L, Green L, et al. Rescue of degenerating neurons and cells by stem cell released molecules: using a physiological renormalization strategy. Physiol Rep. 2019;7(9):e14072.
- Del Papa N, Di Luca G, Sambataro D, et al. Regional grafting of autologous adipose tissue is effective in inducing prompt healing of indolent digital ulcers in patients with systemic sclerosis: results of a monocentric randomized controlled study. Arthritis Res Ther. 2019;21(1):7.
- Delay E, Garson S, Tousson G, Sinna R. Fat injection to the breast. technique, results, and indications based on 880 procedures over 10 years. Aesthet Surg J. 2009;29(5):360–376.
- Largo RD, Tchang LA, Mele V, et al. Efficacy, safety and complications of autologous fat grafting to healthy breast tissue: a systematic review. J Plast Reconstr Aesthet Surg. 2014;67(4):437–448.
- Nelson CM, Bissell MJ. Of extracellular matrix, scaffolds, and signaling: tissue architecture regulates development, homeostasis, and cancer. Annu Rev Cell Dev Biol. 2006;22:87–309.
- Orbay H Hinchcliff KM, Charvet HJ, Sahar DE. Fat graft safety after oncologic surgery: addressing the contradiction between in vitro and clinical studies. Plast Reconstr Surg. 2018;142(6): 1489–1499.
- Tong J, Mou S, Xiong L, et al. Adipose-derived mesenchymal stem cells formed acinar-like structure when stimulated with breast epithelial cells in three-dimensional culture. PLoS One. 2018;13(10):e0204077.
- Zomer HD, Roballo KC, Lessa TB, et al. Distinct features of rabbit and human adipose-derived mesenchymal stem cells: implications for biotechnology and translational research. Stem Cells Cloning. 2018;11:43–54.
- Lu JH, Peng BY, Chang CC, et al. Tumor-targeted immunotherapy by using primary adipose-derived stem cells and an antigen-specific protein vaccine. Cancers (Basel). 2018;10(11). pii: E446.
- Scioli MG, Artuso S, D’Angelo C, et al. Adipose-derived stem cell-mediated paclitaxel delivery inhibits breast cancer growth. PLoS One. 2018;13(9):e0203426.
- Freitag J, Bates D, Wickham J, et al. Adipose-derived mesenchymal stem cell therapy in the treatment of knee osteoarthritis: a randomized controlled trial. Regen Med. 2019;14(3):213–230.
- Choi S, Ryoo SB, Park KJ, et al. Autologous adipose tissue-derived stem cells for the treatment of complex perianal fistulas not associated with Crohn’s disease: a phase II clinical trial for safety and efficacy. Tech Coloproctol. 2017;21(5): 345–353.
- Cho YB, Park KJ, Yoon SN, et al. Long-term results of adipose-derived stem cell therapy for the treatment of Crohn’s fistula. Stem Cells Transl Med. 2015;4(5):532–537.
- Lee WS, Kim HJ, Kim KI, et al. Intra-articular injection of autologous adipose tissue-derived mesenchymal stem cells for the treatment of knee osteoarthritis: a phase IIb, randomized, placebo-controlled clinical trial. Stem Cells Transl Med. 2019;8(6):504–511.
- Lee JH, Park CH, Chun KH, Hong SS. Effect of adipose-derived stem cell-conditioned medium on the proliferation and migration of B16 melanoma cells. Oncology Letters. 2015;10(2):730–736.
- Zhao W, Ren G, Zhang L, et al. Efficacy of mesenchymal stem cells derived from human adipose tissue in inhibition of hepatocellular carcinoma cells in vitro. Cancer Biother Radiopharm. 2012;27(9):606–613.
- Mi F, Gong L. Secretion of interleukin-6 by bone marrow mesenchymal stem cells promotes metastasis in hepatocellular carcinoma. Biosci Rep. 2017;37(4). pii: BSR20170181.
- Xie H, Liao N, Lan F, et al. 3D-cultured adipose tissue-derived stem cells inhibit liver cancer cell migration and invasion through suppressing epithelial-mesenchymal transition. Int J Mol Med. 2018;41(3):1385–1396.
- Yu X, Su B, Ge P, et al. Human adipose derived stem cells induced cell apoptosis and s phase arrest in bladder tumor. Stem Cells Int. 2015;2015:619290.
- Ahn JO, Coh YR, Lee HW, et al. Human adipose tissue-derived mesenchymal stem cells inhibit melanoma growth in vitro and in vivo. Anticancer Res. 2015;35(1):159–168.
- Ryu H, Oh JE, Rhee KJ, et al. Adipose tissue-derived mesenchymal stem cells cultured at high density express IFN-gamma and suppress the growth of MCF-7 human breast cancer cells. Cancer Lett. 2014;352(2):220–227.
- Takahara K, Ii M, Inamoto T, et al. Adipose-derived stromal cells inhibit prostate cancer cell proliferation inducing apoptosis. Biochem Biophys Res Commun. 2014;446(4):1102–1107.
- Wei S, Xie S, Yang Z, et al. Allogeneic adipose-derived stem cells suppress mTORC1 pathway in a murine model of systemic lupus erythematosus. Lupus. 2018;28(2):199–209.
- Kim LC Cook RS, Chen J. mTORC1 and mTORC2 in cancer and the tumor microenvironment. Oncogene. 2017;36(16):2191–2201.
- Lee SM, Lee SC, Kim SJ. Contribution of human adipose tissue–derived stem cells and the secretome to the skin allograft survival in mice. J Surg Res. 2014;188(1):280–289.
- Clark KC, Fierro FA, Ko EM, et al. Human and feline adipose-derived mesenchymal stem cells have comparable phenotype, immunomodulatory functions, and transcriptome. Stem Cell Res Ther. 2017;8(1):69.
- Blazquez R, Sanchez-Margallo FM, de la Rosa O, et al. Immunomodulatory potential of human adipose mesenchymal stem cells derived exosomes on in vitro stimulated T cells. Front Immunol. 2014;5:556.
- Serejo TRT, Silva-Carvalho AÉ, Braga LDCF, et al. Assessment of the immunosuppressive potential of INF-gamma licensed adipose mesenchymal stem cells, their secretome and extracellular vesicles. Cells. 2019;8(1):22.
- Baharlou R, Rashidi N, Ahmadi-Vasmehjani A, et al. Immunomodulatory effects of human adipose tissue-derived mesenchymal stem cells on T cell subsets in patients with rheumatoid arthritis. Iran J Allergy Asthma Immunol. 2019;18(1):114–119.
- Solakoglu O, Götz W, Kiessling MC, et al. Improved guided bone regeneration by combined application of unmodified, fresh autologous adipose derived regenerative cells and plasma rich in growth factors: a first-in-human case report and literature review. World J Stem Cells. 2019;11(2):124–146.
- Protogerou V, Michalopoulos E, Mallis P, et al. Administration of adipose derived mesenchymal stem cells and platelet lysate in erectile dysfunction: a single center pilot study. Bioengineering. 2019;6(1):21.
- Zhou F, Gao S, Wang L, et al. Human adipose-derived stem cells partially rescue the stroke syndromes by promoting spatial learning and memory in mouse middle cerebral artery occlusion model. Stem Cell Res Ther. 2015;6:92.
- Jiang D, Muschhammer J, Qi Y, et al. Suppression of neutrophil-mediated tissue damage—a novel skill of mesenchymal stem cells. Stem Cells. 2016;34(9):2393–2406.
- Bonafede R, Scambi I, Peroni D, et al. Exosome derived from murine adipose-derived stromal cells: neuroprotective effect on in vitro model of amyotrophic lateral sclerosis. Exp. Cell Res. 2015;340(1):150–158.
- Perez LM, Bernal A, San Martín N, et al. Metabolic rescue of obese adipose-derived stem cells by Lin28/Let7 pathway. Diabetes. 2013;62(7): 2368–2379.
- Peng W, Gao T, Yang ZL, et al. Adipose-derived stem cells induced dendritic cells undergo tolerance and inhibit Th1 polarization. Cell Immunol. 2012;278(1–2):152–157.
- Ivanova-Todorova E, Bochev I, Mourdjeva M, et al. Adipose tissue-derived mesenchymal stem cells are more potent suppressors of dendritic cells differentiation compared to bone marrow-derived mesenchymal stem cells. Immunol Lett. 2009;126(1–2):37–42.
- Ribeiro A, Laranjeira P, Mendes S, et al. Mesenchymal stem cells from umbilical cord matrix, adipose tissue and bone marrow exhibit different capability to suppress peripheral blood B, natural killer and T cells. Stem Cell Res Ther. 2013;4(5):125.
- Ali N, Zirak B, Rodriguez RS, et al. Regulatory T cells in skin facilitate epithelial stem cell differentiation. Cell. 2017;169(6):1119–1129.
- Horsley V, Naik S. Tregs Expand the skin stem cell niche. Dev Cell. 2017;41(5):455–456.
- Rybalko V, Hsieh PL, Ricles LM, et al. Therapeutic potential of adipose-derived stem cells and macrophages for ischemic skeletal muscle repair. Regen Med. 2017;12(2):153–167.
- Adutler-Lieber S, Ben-Mordechai T, Naftali-Shani N, et al. Human macrophage regulation via interaction with cardiac adipose tissue-derived mesenchymal stromal cells. J Cardiovasc Pharmacol Ther. 2013;18(1):78–86.
- Sindrilaru A, Peters T, Wieschalka S, et al. An unrestrained proinflammatory M1 macrophage population induced by iron impairs wound healing in humans and mice. J Clin Invest. 2011;121(3):985–997.
- Roszer T. Understanding the mysterious M2 macrophage through activation markers and effector mechanisms. Mediators Inflamm. 2015;2015:816460.
- Roberts AB, Sporn MB, Assoian RK, et al. Transforming growth factor type beta: rapid induction of fibrosis and angiogenesis in vivo and stimulation of collagen formation in vitro. Proc Natl Acad Sci U S A. 1986;83(12):4167–4171.
- Murray PJ, Wynn TA. Protective and pathogenic functions of macrophage subsets. Nat Rev Immunol. 2011;11(11):723–737.
- Li Y, Gao X, Wang J. Human adipose-derived mesenchymal stem cell-conditioned media suppresses inflammatory bone loss in a lipopolysaccharide-induced murine model. Exp Ther Med. 2018;15(2):1839–1846.
- Johnson V, Webb T, Norman A, et al. Activated mesenchymal stem cells interact with antibiotics and host innate immune responses to control chronic bacterial infections. Sci Rep. 2017;7(1):9575.
- Sutton MT, Fletcher D, Ghosh SK, et al. Antimicrobial properties of mesenchymal stem cells: therapeutic potential for cystic fibrosis infection, and treatment. Stem Cells Int. 2016;2016:5303048.
- Matsuzaki K. Control of cell selectivity of antimicrobial peptides. Biochim Biophys Acta. 2009;1788(8):1687–1692.
- Brown KL, Poon GF, Birkenhead D, et al. Host defense peptide LL-37 selectively reduces proinflammatory macrophage responses. J Immunol. 2011;186(9):5497–5505.
- Izadpanah R, Kaushal D, Kriedt C, et al. Long-term in vitro expansion alters the biology of adult mesenchymal stem cells. Cancer Res. 2008;68(11):4229–4238.
- Dufrane D. Impact of age on human adipose stem cells for bone tissue engineering. Cell Transplant. 2017;26(9):1496–1504.
- Wu H, Li JZ, Xie BD, et al. Lower senescence of adipose-derived stem cells than donor-matched bone marrow stem cells for surgical ventricular restoration. Stem Cells Dev. 2018;27(9):612–623.
- Niu P, Smagul A, Wang L, et al. Transcriptional profiling of interleukin-2-primed human adipose derived mesenchymal stem cells revealed dramatic changes in stem cells response imposed by replicative senescence. Oncotarget. 2015;6(20):17938–17957.
- Kokai LE, Traktuev DO, Zhang L, et al. Adipose stem cell function maintained with age: an intra-subject study of long-term cryopreserved cells. Aesthet Surg J. 2017;37(4):454–463.
- Pan X, Chen YH, Yang YK. Relationship between senescence in macaques and bone marrow mesenchymal stem cells and the molecular mechanism. Aging. 2018;11(2):590–614.
- Zhang H, Fazel S, Tian H, et al. Increasing donor age adversely impacts beneficial effects of bone marrow but not smooth muscle myocardial cell therapy. Am J Physiology. 2005;289(5): 2089–2096.
- Ismail HD, Arif S, Pawitan J, et al. The passage effect on the senescence profile of cryopreserved bone marrow and adipose-derived mesenchymal stem cells. Annu Res Rev Biol. 2018;24(1):1–11.
- Fafian-Labora J, Lesende-Rodriguez I, Fernández-Pernas P, et al. Effect of age on proinflammatory miRNAs contained in mesenchymal stem cell-derived extracellular vesicles. Sci Rep. 2017;7:43923.
- Ishikawa F, Yoshida S, Saito Y, et al. Chemotherapy-resistant human AML stem cells home to and engraft within the bone-marrow endosteal region. Nat Biotechnol. 2007;25(11):1315–1321.
- Liu et C, Feng X, Wang B, et al. Bone marrow mesenchymal stem cells promote head and neck cancer progression through Periostin-mediated phosphoinositide 3-kinase/Akt/mammalian target of rapamycin. Cancer Sci. 2018;109(3): 688–698.
- Araf S, Wang J, Ashton-Key M, et al. Transmission of diffuse large B-cell lymphoma by an allogeneic stem-cell transplant. Haematologica. 2019;104(4):e174–e177.
- Tai YL, Chen KC, Hsieh JT, Shen TL, et al. Exosomes in cancer development and clinical applications. Cancer Sci. 2018;109(8):2364–2374.
- Roato I, Ferracini R. Cancer stem cells, bone and tumor microenvironment: key players in bone metastases. Cancers (Basel). 2018;10(2):56.
- Tokoyoda K, Egawa T, Sugiyama T, et al. Cellular niches controlling B lymphocyte behavior within bone marrow during development. Immunity. 2004;20(6):707–718.
- Erices AA, Allers CI, Conget PA, et al. Human cord blood-derived mesenchymal stem cells home and survive in the marrow of immunodeficient mice after systemic infusion. Cell Transplant. 2003;12(6):555–561.
- Nusse YM, Savage AK, Marangoni P, et al. Parasitic helminths induce fetal-like reversion in the intestinal stem cell niche. Nature. 2018;559(7712):109–113.
- Houghton JM, Stoicov C, Nomura S, et al. Gastric cancer originating from bone marrow-derived cells. Science. 2004;306(5701):1568–1571.
- Calvi LM, Link DC. The hematopoietic stem cell niche in homeostasis and disease. Blood. 2015;126(22):2443–2451.
- Shi H, Wang Y, Li R, et al. Alteration in the cytokine secretion of bone marrow stromal cells from patients with chronic myelomonocytic leukemia contribute to impaired hematopoietic supportive activity. Stem Cells Int. 2018;2018:5921392.
- Lazenby M, Ottmann OG, Wilson K, et al. Extracellular microvesicle cytokines secreted from bone marrow mesenchymal cells mediate proliferative and survival advantage in acute myeloid leukaemia. Blood. 2018;132:2744.
- Schurch CM, Riether C, Ochsenbein AF. Cytotoxic CD8+ T cells stimulate hematopoietic progenitors by promoting cytokine release from bone marrow mesenchymal stromal cells. Cell Stem Cell. 2014;14(4):460–472.
- Sansone P, Storci G, Tavolari S, et al. IL-6 triggers malignant features in mammospheres from human ductal breast carcinoma and normal mammary gland. J Clin Invest. 2007;117(12):3988–4002.
- Nishi Y, Murakami A, Murayama Y, et al. Adipose tissue-derived mesenchymal stem cells ameliorate bone marrow aplasia related with graft-versus-host disease in experimental murine models. Transpl Immunol. 2019;S0966-3274(18): 30181–30183.
- Tozawa K, Ono-Uruga Y, Yazawa M, et al. Manufacture of platelets from human adipose tissue-derived mesenchymal stromal/stem cells: functional comparison to concentrate platelets. Blood. 2016;133(7):633–643.
- Andreeva E, Andrianova I, Sotnezova E, et al. Hematopoiesis-supportive function of growth-arrested human adipose-tissue stromal cells under physiological hypoxia. J Biosci Bioeng. 2019;127(5):647–654.

