 J Clin Aesthet Dermatol. 2021;14(9):45–49.
J Clin Aesthet Dermatol. 2021;14(9):45–49.
by Mona Soliman, MD; Hanaa Abdel Aal, Msc; Ahmed M. Sadek, PhD; and Abeer Attia Tawfik, PhD
All authors are with the Dermatology Unit, Medical Applications at the Laser National institute of Laser Enhanced Sciences, at Cairo University in Cairo , Egypt. Ms. Aal is also with the Cairo Hospital for Dermatology and Venereology in Cairo, Egypt.
FUNDING: No funding was provided for this article.
DISCLOSURES: The authors report no conflicts of interest relevant to the content of this article.
ABSTRACT: Background. Intralesional injection of corticosteroid (ILIS) and pulsed-dye laser (PDL) have been used in nail psoriasis treatment with variable outcomes.
Objective. We sought to compare the efficacy of ILIS to PDL for the treatment of psoriatic fingernails using a dermoscope in the assessment and follow-up.
Methods. This study included 30 patients with bilateral nail psoriasis. The fingernails of one hand were treated with PDL, whereas ILIS was used to treat the fingernails of the other hand. One psoriatic nail was left alone as a control. Every patient received four treatment sessions once every month. Efficacy was recorded clinically using the Nail Psoriasis Severity Index (NAPSI) and by a dermoscope before treatment (baseline) and at eight, 24, and 36 weeks after treatment.
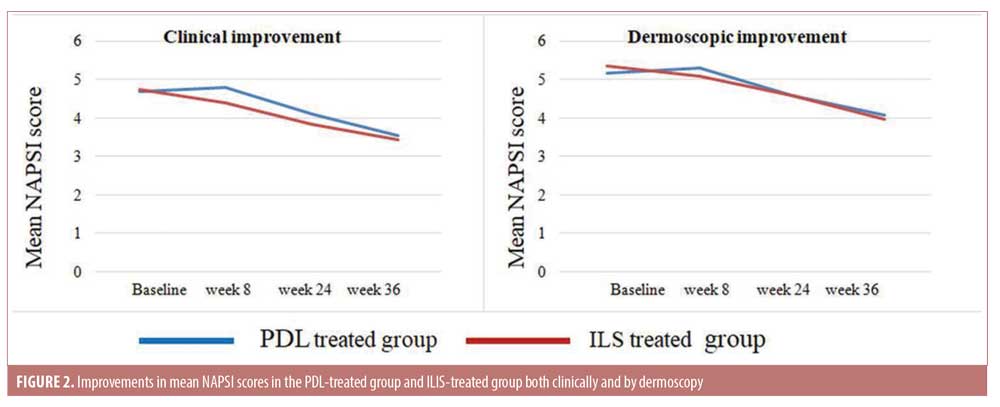
Results. The assessment by NAPSI revealed improvements of 22.24% and 24.11% occurred in the laser group and the intralesional steroid group, respectively. Also, the dermoscopic assessments revealed an improvement of 18.33% in the laser group versus that of 21.69% in the ILES. No significant difference was found between the two groups.
Conclusion. Both PDL and ILIS are considered safe treatments for nail psoriasis, yielding nearly equal results. The dermoscope is a reliable tool for the diagnosis and follow-up of nail psoriasis treatment.
Keywords: Nail psoriasis, PDL, intralesion steroid, NAPSI, dermoscope
Psoriasis is a chronic inflammatory disease affecting up to 3% of the general population.1 Nail psoriasis affects 50% of psoriatic patients.2 Pitting, onycholysis, and salmon-colored patches on the nail bed are the main signs of nail psoriasis. Other signs may be seen, such as splinter hemorrhages, nail bed hyperkeratosis, nail thickening and crumbling, paronychia, leukonychia, trachyonychia, and erythema of the lanula.3 There is no standardized regimen for the treatment of nail psoriasis, and the choice of therapy depends on the patient’s history, clinical manifestations, and concomitant diseases.4 The success of topical therapy (e.g., steroid, tazarotene, 5-fluorouracil, calcipotriol) is limited by the difficulty in achieving adequate antipsoriatic concentrations at the inflammatory sites.5 On the other hand, systemic therapy (e.g., methotrexate, cyclosporine, and retinoids) has moderate efficacy, infrequent complete clearance, and a declining effect over time.6 In the past few years, pulsed-dye laser (PDL) therapy has been used for treating psoriasis because of the highly vascular nature of psoriatic lesions. Aside from the destruction of blood vessels, PDL can reduce the number of helper T-cells in the dermis and cytotoxic T-cells in the epidermis and normalize epidermal proliferation and abnormal keratinization.7 Oram et al8 found that onycholysis and subungual hyperkeratosis demonstrated the earliest response to treatment. Meanwhile, to assess the efficacy of using different pulse durations, Treewittayapoom et al9 compared the efficacy of different pulse durations of PDL in the treatment of nail psoriasis where they stated that there was a significant reduction in the Nail Psoriasis Severity Index (NAPSI) score in both groups. Intralesional corticosteroid injection (ILIS) is considered to be a standard treatment for nail psoriasis.10 Triamcinolone acetonide (TAC) is the most commonly used intralesional corticosteroid at a concentration of 2.5 to 10 mg/mL.11
Dermoscopy is considered a good tool for detecting signs of nail psoriasis and can help with the early detection of nail affection.12 During the last few years, dermoscopy has become widely used as an effective tool in the diagnosis of nail diseases.13
The first goal of this work was to compare the therapeutic effect of PDL versus that of ILIS in the treatment of nail psoriasis. The second one was to assess the role of dermoscopy in the diagnosis of nail psoriasis and in the follow-up of the outcomes.
Methods
This randomized, intrapatient comparative, controlled study was approved by the National institute of Laser Enhanced Sciences ethical board, and informed written consent forms were signed by the included patients. The study was also conducted according to the Declaration of Helsinki.
Thirty patients were enrolled in this study. Patients who participated had bilateral nail psoriasis affecting at least three nails and no history of previous topical systemic therapy for psoriasis or ILIS treatment within the previous two months. Patients were excluded from the study for any of the following reasons: younger than 12 years of age, pregnancy, and presence of onychomycosis (excluded by KOH and dermoscopy).
Treatment protocol. The psoriatic nails of one hand were treated by PDL and the fingernails of the other hand were treated by ILIS. Four treatment sessions were applied at four-week intervals. One nail was left as a control nail on each hand. Randomization was completed via the envelope method. The psoriatic nails were divided into three groups as follows:
In Group 1 (treated by PDL), the psoriatic nails were treated with 585-nm PDL on the proximal and lateral nail folds (Cynergy; Cynosure, Westford, MA, USA). The fluence used ranged from 8.0 to 10.0 J/cm2, with a 1.5-ms pulse duration and 7-mm spot size. An air-cooling device was used (Zimmer MedizinSystems, Irvine, CA, USA).
In Group 2 (treated by ILIS), in this group, the psoriatic nails were treated with ILIS by TAC in a concentration of 5 mg/mL. Specifically, they were injected using a needle-free device (MadaJet; Mada Medical, Carlstadt, NJ, USA) in the proximal and distal nail folds with 1 cm between every two injection sites.
In the control group (no treatment), psoriatic nails in each hand were left without treatment to serve as controls.
Evaluation methods. The total NAPSI score was identified and recorded for each nail, both clinically and by dermoscopy, before treatment (baseline) and at eight, 24, and 36 weeks after the start of treatment.
NAPSI was used to evaluate the psoriatic findings in the nail before treatment, after treatment, and during follow-up, with a score assigned to each nail for both the nail bed and nail matrix psoriasis. The nail plate was divided into four quadrants by imaginary longitudinal and horizontal lines. Nail matrix psoriasis was assessed for by the presence of nail pitting, leukonychia, red spots in the lanula, and crumbling in each quadrant of the nail. Nail bed psoriasis was assessed for by the presence of onycholysis, oil drop (salmon patch) dyschromia, splinter hemorrhages, and nail bed hyperkeratosis in each quadrant of the nail. If the score was 0, this meant that no findings of interest were present; conversely, A score of 1 denoted that findings were present in one quadrant of the nail, a score of 2 meant that findings were present in two quadrants of a nail, and so forth. Thus, each nail had a matrix score of 0 to 4 and a nail bedscore of 0 to 4, with a total nail score that was the sum of the nail bedand nail matrix scores (0–8 points). The sum of the total score of all involved fingernails is the total NAPSI score for that patient at that time.14
Clinical evaluation. All fingernails were photographed using a Samsung Galaxy Note 2 (Samsung, Suwon-si, Korea) camera with eight megapixels and a resolution of 3,264 × 2,448 pixels.
Dermoscopic evaluation. A dermoscopic evaluation of the nail bedand matrix psoriasis signs was completed for each nail before treatment, after treatment, and during follow-up (Dermlite 3Gen; Dermlite, San Juan Capistrano, CA, USA) with a magnification of 10×.
Patient satisfaction. Patients were asked to rate their satisfaction with each treatment modality as satisfied, partially satisfied, or not satisfied. They were asked to report any side effect.
Statistical analysis. Data were summarized and analyzed using the Statistical Package for the Social Sciences version 17 (IBM Corporation, Armonk, NY, USA), Microsoft Excel 2013 (Microsoft Corp., Redmond, WA, USA), and Medcalc version 15.8 (MedCalc Software, Flanders, Belgium). Data distribution was assessed for normality by using the Kolmogorov–Smirnov test. Normally distributed numerical data were presented as mean±standard deviation values. A comparison of mean values was performed using the student’s t-test. Categorical data are presented as frequencies and compared using the chi-squared test. In all statistical tests, the level of significance was fixed at the 5% level. A probability (p)-value of greater than 0.05 indicated no statistically significant difference, while that of less than 0.05 indicated a statistically significant difference. Correlation was performed using Pearson’s method test.
Results
A total of 192 psoriatic nails were treated by PDL or ILIS in 25 patients. Fifty nails were left without treatment as a control group. Five patients discontinued study involvement after the first session due to inconvenience of the treatment results. Fifteen patients presented with associated skin psoriasis (50%), whereas the other 15 patients had isolated nail psoriasis (50%). Patient ages ranged from 12 to 65 years (32.6±18 years), and disease duration ranged from six to 180 months (16.9±31.6 months).
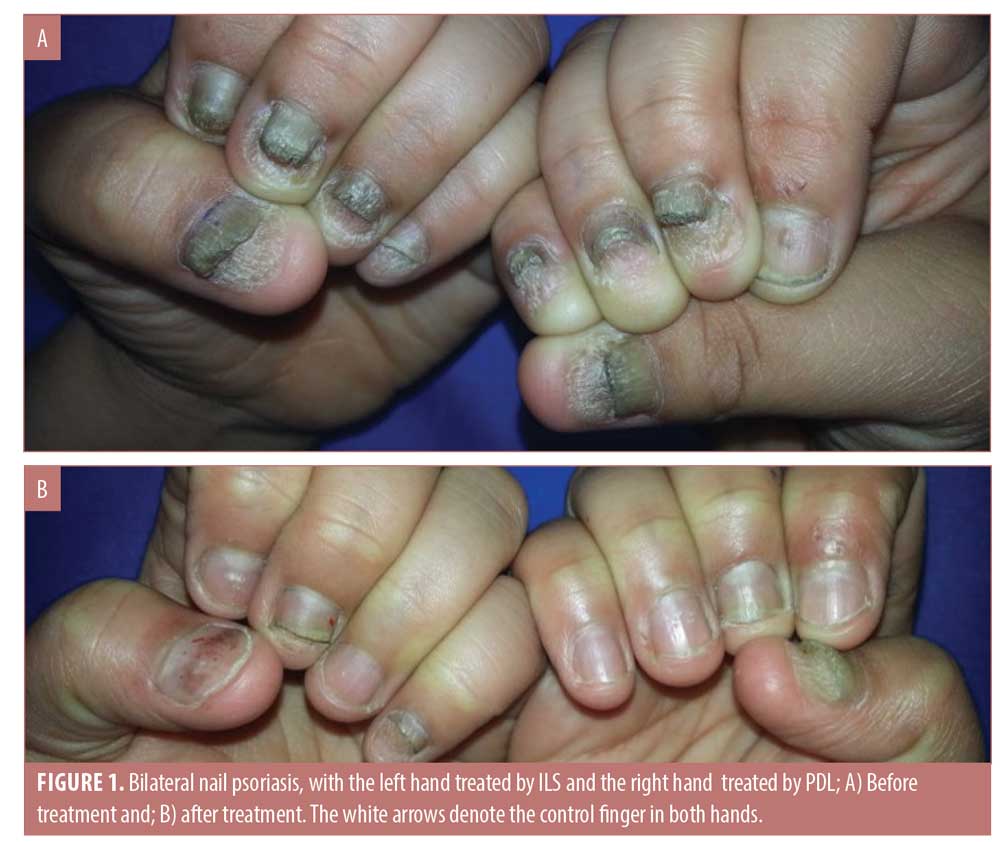
Both treatment modalities triggered variable degrees of improvement; however, there was no significant difference between the groups. In the PDL-treated group (Group 1), a significant decrease in the mean NAPSI score at Week 36 was noticed (p<0.02), with a median improvement of 22.24%. The p-value was not significant in the control group. On the other hand, the ILIS-treated group (Group 2) showed earlier improvements in NAPSI score at Week 24 with statistical significance (p<0.03) (Figures 1 and 2).
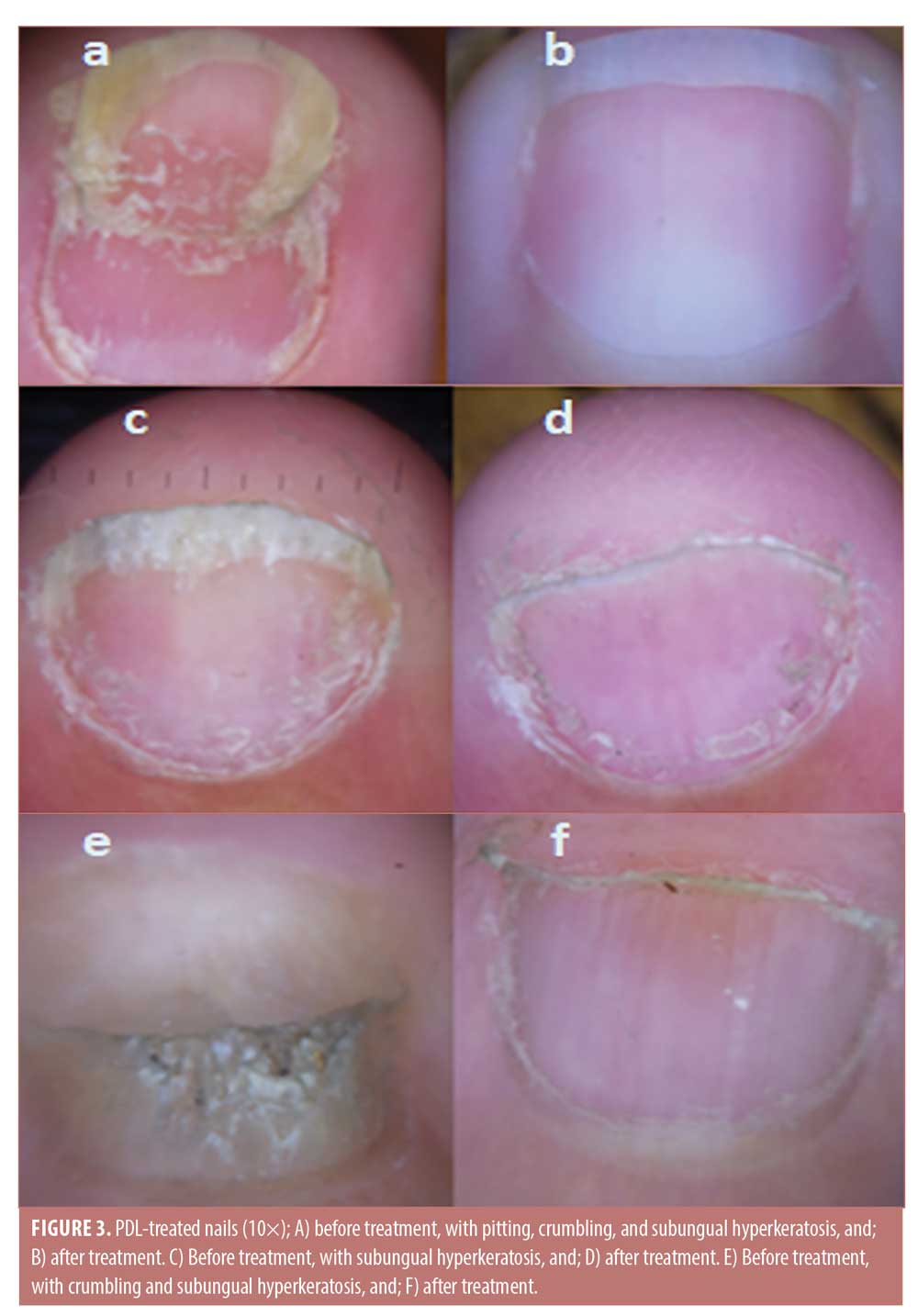
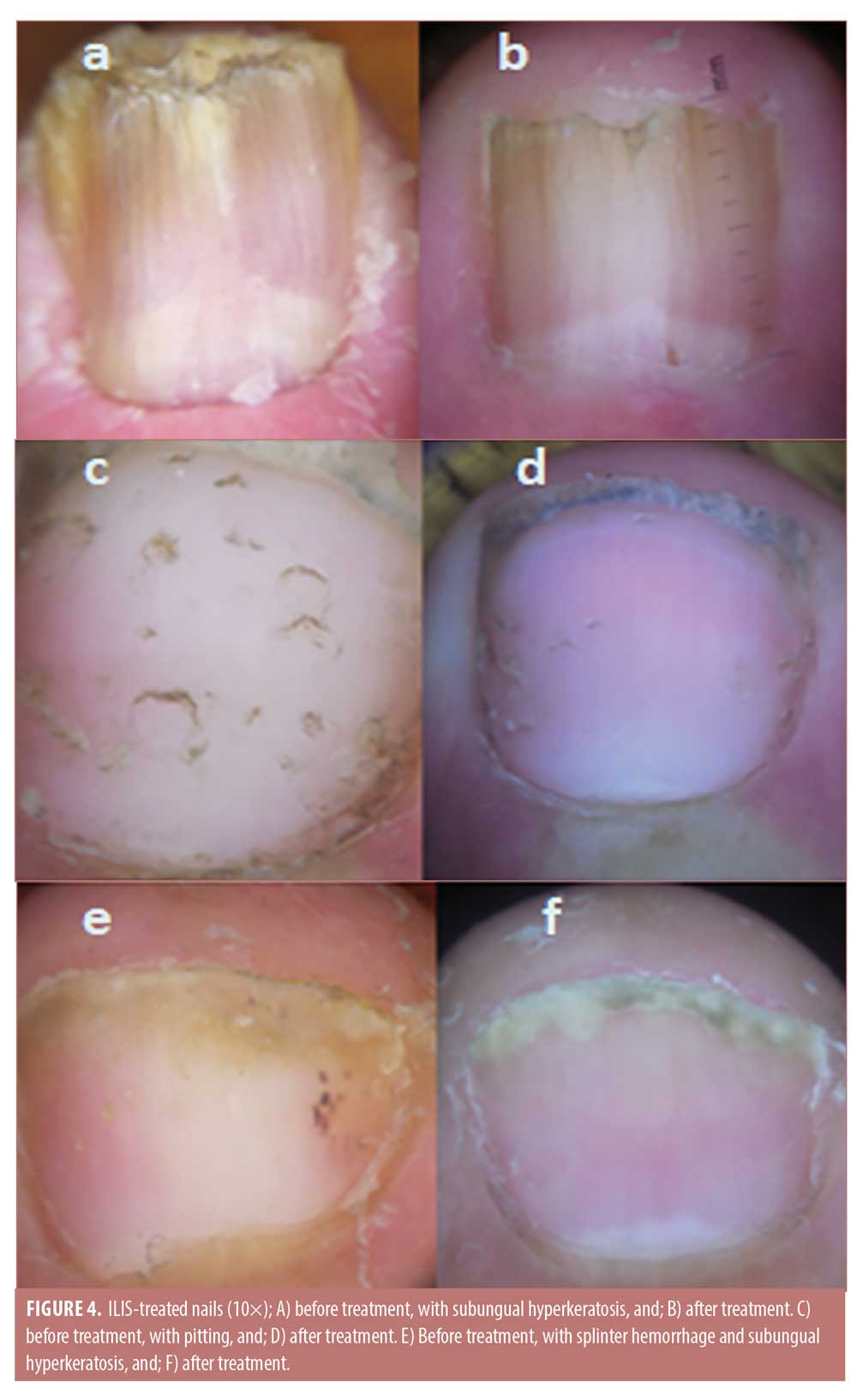
Dermoscopic findings. Excellent improvement was seen in splinter hemorrhage and onycholysis. Moderate improvement was seen with pitting and crumbling. Finally, the least improvement was observed in subungual hyperkeratosis (Figures 3 and 4).
Patient satisfaction. Twelve (48%) of the study participants were satisfied with their ILIS treatment outcomes. On the other hand, nine (36%) patients were satisfied with their PDL outcomes. Six (24%) patients were satisfied with the results of both methods equally. Four patients (16%) expressed their dissatisfaction with both treatments.
Side effects. The ILIS-treated group experienced mild pain and pinpoint bleeding at injection sites that stopped spontaneously. In the PDL-treated group, transient petechiae were noticed in some patients along with mild purpura that resolved within one week.
Discussion
Both PDL and ILIS have been used with different success rates in the treatment of nail psoriasis. In this study, no significant difference was found between the outcomes of the ILIS and PDL groups. However, patients recognized earlier improvement with ILIS, which was significantly detected at the 24th week, whereas the PDL improvement appeared at the 36th week. This might be attributed to the mechanism of action of ILIS, which has anti-inflammatory, antiproliferative, vasoconstrictive, and immunosuppressive properties,15 whereas PDL acts mainly according to the concept of selective photothermolysis, leading to photocoagulation of smaller blood vessels,16 in addition to the immunomodulatory mechanism.17
With both modalities, good results were seen in terms of splinter hemorrhage, crumbling, pitting, and onycholysis, while improvements in subungual hyperkeratosis were limited. Other signs, such as oil drop and leukonychia, were markedly improved.
PDL is less painful and easy to apply but more expensive. On the other hand, ILIS is cheap and more affordable but also more painful.
Many studies have used PDL in the treatment of nail psoriasis. Fernández-Guarino et al18 were the first to use PDL for the treatment of nail psoriasis by comparing the efficacy of PDL versus PDT (using PDL as a light source). These authors treated 61 nails with PDT and 60 nails with PDL in 14 patients with nail psoriasis. Sessions were conducted monthly for six months, and clinical evaluations were performed at baseline and after three and six months according to NAPSI scores. A decrease in NAPSI scores was observed with both treatments and for both the nail matrix and nailbed.18
On the contrary, Al-Mutairi et al19 found that the best results were obtained in subungual hyperkeratosis and onycholysis when they treated 304 psoriatic nails, including 148 with an excimer laser twice weekly and 156 with PDL once every four weeks, for a total of 12 weeks in 42 patients. NAPSI scores were recorded clinically at baseline and Weeks 4, 8, 12, and 24. The improvement in NAPSI score was significantly greater in the PDL group than the excimer laser group.19 In the current study, the earliest and best results were obtained in splinter hemorrhage and onycholysis and, although subungual hyperkeratosis showed clinical improvement, the dermoscopic assessment revealed the scope of improvement was more limited This may be attributed to the precise assessment of the dermoscope.
In agreement with the obtained results in this study, Nantel-Battista et al20 treated 17 patients with nail psoriasis with triamcinolone acetonide needle-free injection. Four treatments sessions were scheduled every 4±1 weeks. Clinical efficacy was evaluated according to the NAPSI score of the target nail before and after the treatment. There was a significant difference in the mean NAPSI scores before and after treatment.20
The use of a dermoscope for the evaluation of the signs of nail psoriasis, such as pitting, onycholysis, splinter hemorrhages, and oil drop sign, has been reported by Yadav and Khopkar12 in a cross-sectional study where 68 patients with chronic plaque psoriasis were compared with an equal number of age- and sex-matched healthy volunteers. Dermoscopic findings of interest were found in 46 patients, while 22 patients were free from such. Hashimoto et al21 used a dermoscope to clarify the features of nail psoriasis during biologic treatment of psoriasis; six patients with psoriatic nails underwent two dermoscopic examinations 17 to 42 weeks apart. They used the modified NAPSI score to assess dermoscopic features of nail psoriasis, which was improved in two patients and unchanged in four patients. They concluded that dermoscopy can detect nail changes during psoriasis treatment and should be used to evaluate treatment success.
We used the NAPSI score to identify and assess dermoscopic features of nail psoriasis. A significant improvement in NAPSI score was noticed in the PDL-treated group (p=0.03), while a more significant improvement was apparent in the ILIS-treated group (p=0.01).
To the best of our knowledge, no study has yet compared these modalities so far, which was the main goal of our work. Moreover, the dermoscope, which is a reliable objective method, was used in diagnosis and follow-up to guarantee better assessments.
A limitation of this study was the short follow-up period. Further intra-individual studies with longer follow-up periods are recommended to obtain optimal results.
Conclusion
This prospective, randomized, controlled study is the only study known to have compared the effects of PDL and ILIS in the treatment of nail psoriasis. It demonstrated that both PDL and ILIS are safe methods in the treatment of nail psoriasis, with minimal side effects. We found that dermoscopy is a good and easy tool for diagnosis and assessment of nail psoriasis treatment.
References
- Ventura A, Mazzeo M, Gaziano R, et al. New insight into. The pathogenesis of nail psoriasis and overview of treatment strategies. Drug Des Devel Ther. 2017;11:2527–2535.
- Haneke E. Nail psoriasis: clinical features, pathogenesis, differential diagnoses and management. Psoriasis (Auckl). 2017;7:51–63.
- Piraccini BM, Strace M. Optimal management of nail disease in patients with psoriasis. Psoriasis (Auckl). 2015;5:25–33.
- Radtke MA, Beikert FC, Augustin M. Nail psoriasis—a treatment challenge. J Dtsch Dermatol Ges. 2013;11 (3):203–219.
- Hern S, Stanton AWB, Mellor RH, et al. In vivo qualification of the structural abnormalities in psoriatic micro vessels before and after pulsed-dye laser treatment. Br J Dermatol. 2005;152(3):505–511.
- Yin N, Choudhary S, Nouri K. Pulsed dye laser for the treatment of nail psoriasis. Cutis. 2013;92(3):129–135.
- Rikihisa N, Wantanabe S, Saito Y, et al. Artificial red blood cells as potential photosensitizers in dye laser treatment against port-wine stains. J Funct Biomater. 2017;8(2):14.
- Oram Y, Akkaya AD. Treatment of nail psoriasis: common concepts and new trends. Dermatol Res Pract. 2013:2013;180496.
- Treewittayapoom C, Singvahanont P, Chanprapaph K, et al. The effect of different pulse durations in the treatment of nail psoriasis with 595-nm pulsed-dye laser: a randomized, double-blind, intrapatient left-to-right study. J Am Acad Dermatol. 2012;66(5):807–812.
- Boontaveeyuwat E, Sipa-Archa N, Danchaivijitar N, et al. Randomized comparison of efficacy and safety of intralesional triamcinolone injection and clobetasol propionate ointment for psoriatic nails. J Dermatolog Treat. 2019;30(2):117–122.
- Coppola MM, Salzillo R, Segreto F, Persichetti P. Triamcinolone acetenoide intralesional injection for the treatment of keloid scar: patient selection and perspectives. Clin Cosmet Investig Dermatol. 2018;11:387–396.
- Yadav TA, Khopkar US. Dermoscopy to detect signs of subclinical nail involvement in chronic plaque psoriasis: a study of 68 patients. Indian J Dermatol. 2015;60(3):272–275.
- Yorulmaz A, Artuz F. A study of dermoscopic features of nail psoriasis. Postepy Dermatol Alergol. 2017;34(1):28–35.
- Rich P, Scher RK. Nail Psoriasis Severity Index: a useful tool for evaluation of nail psoriasis. J Am Acad Dermatol. 2003;49(2):206–212.
- Uva L, Miguel D, Pinheiro C, et al. Mechanisms of action of topical corticosteroids in psoriasis. Int J Endocrinol. 2012;2012:561018.
- Babilas P, Shafirstein G, Bäumler W, et al. Selective photothermolysis of blood vessels following flashlamp-pumped pulsed-dye laser irradiation: in vivo results and mathematical modelling are in agreement. J Invest Dermatol. 2005;125(2):343–352.
- Zhang P, Wu MX. A clinical review of phototherapy for psoriasis. Lasers Med Sci. 2018;33(1)173–180.
- Fernández-Guarino M, Harto A, Sánchez-Ronco M, et al. Pulsed dye laser vs. photodynamic therapy in the treatment of refractory nail psoriasis: a comparative pilot study. J Eur Acad Dermatol Venereol. 2009;23(8):891–895.
- Al-Mutairi N, Noor T, Al-Haddad A. Single blinded left- to- right comparison study of excimer laser versus pulsed-dye laser for the treatment of nail psoriasis. Dermatol Ther (Heidelb). 2014;4(2):197–205.
- Nantel-Battista M, Richer V, Marcil I, et al. Treatment of nail psoriasis with intralesional triamcinolone acetonide using a needle-free jet injector: a prospective trial. J Cutan Med Surg. 2014;18(1):38–42.
- Hashimoto Y, Uyama M, Takada Y, et al. Dermoscopic features of nail psoriasis treated with biologics. J Dermatol. 2017;44(5):538–541.

