J Clin Aesthet Dermatol. 2023;16(8):44-46.
J Clin Aesthet Dermatol. 2023;16(8):44-46.
by Joseph Masison, PhD; Vijay Kodumudi, MD, MBA, MPH; Eric J. Beltrami, MD; and Hao Feng, MD, MHS
Drs. Masison and Beltrami are with the University of Connecticut School of Medicine in Farmington, Connecticut. Dr. Kodumudi is with the Internal Medicine Department at Waterbury Hospital, and the Yale School of Medicine in New Haven, Connecticut. Dr. Feng is with the Department of Dermatology at the University of Connecticut Health Center in Farmington, Connecticut.
FUNDING: No funding was provided for this article.
DISCLOSURES: Dr. Feng has consulted for Cytrellis Biosystems, Inc. and Soliton, Inc. All other authors report no conflicts of interest relevant to this article.
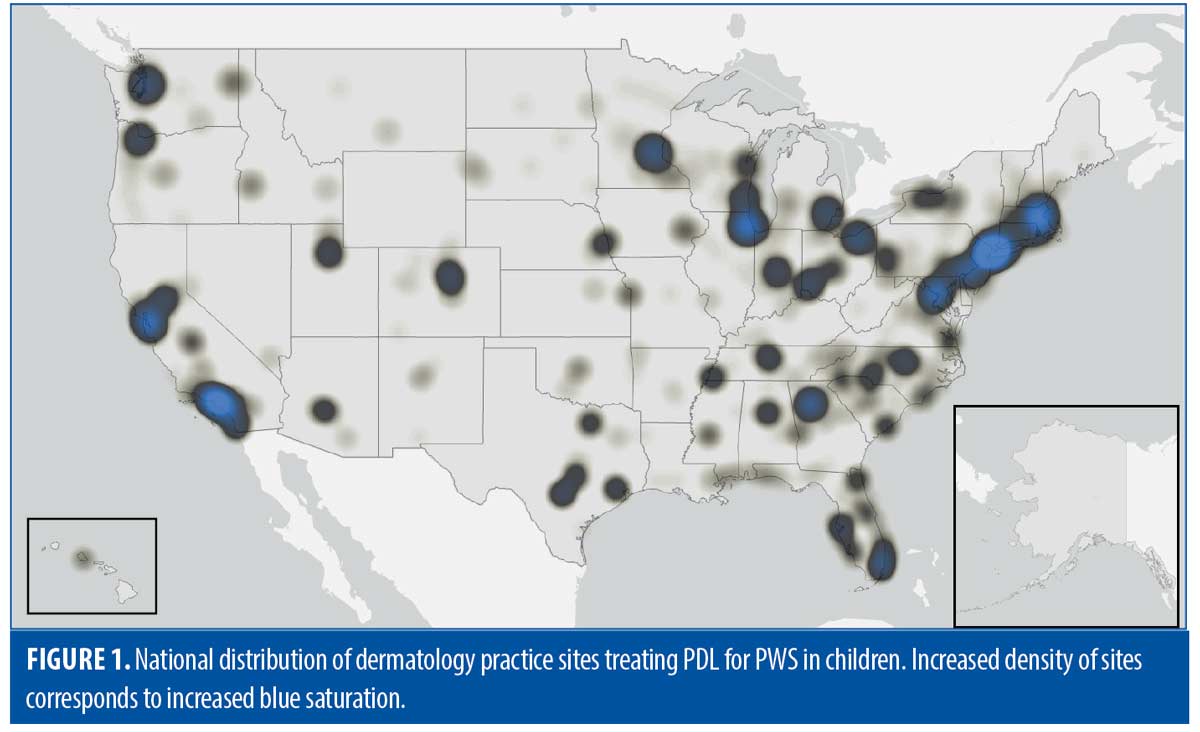
ABSTRACT: Prior research has demonstrated that early treatment of port-wine birthmark (PWB) with pulsed dye laser (PDL) yields optimal patient outcomes. Given the known variations in practice patterns among dermatologists offering PDL, we conducted a cross-sectional analysis in order to determine the travel distance and time to practice locations offering PDL therapy for PWB among the pediatric population. We determined the travel time and distance from each county population center in the United States to the nearest PDL site using ArcGIS and linked the data to demographic characteristics in each census tract. 1,243 practice sites were identified that offer PDL treatment for PWB for patients under the age of 18. Children living in urban areas were found to have a significantly shorter median travel time and distance to PDL sites (6.1 miles, 11.8 minutes) compared to children living in rural areas (60.9 miles, 66.7 minutes). Additionally, uninsured children were found to travel longer average distances (32.2 miles) than insured children (24.2 miles). These findings suggest that certain socioeconomically disadvantaged groups have increased travel burden when obtaining PDL treatment for PWB. Transportation resources and support may need to be given to certain patients to ensure timely and effective PDL treatment.
Keywords: Pulsed dye laser, port-wine birthmark, pediatrics, distance, travel, disparities, access, demographics
Pulsed dye laser (PDL) has a critical role in pediatric dermatology as the gold-standard treatment for port-wine birthmark (PWB). Delayed access to treatment, particularly after infancy, leads to suboptimal medical and psychosocial outcomes for patients.1,2 Given known variations in practice patterns among dermatologists offering PDL,2 this study sought to characterize travel distance and time to PDL sites in the pediatric population considering population and geographic characteristics.
Methods
The Physician Finder tool from Candela Medical was used to identify practices that own a Vbeam, the most commonly used PDL device in the United States.3 Practices were phoned in order to determine their minimum age of treatment for PDL. We determined travel time and distance from each county population center (n=3,143) in the United States to the nearest PDL site using ArcGIS, parameterized to quickest driving route assuming normal traffic patterns. Travel estimates were linked to demographic characteristics in each census tract based on the 2020 American Community Survey. Statistical analyses were performed using SciPy v1.9.0.
Results
We identified 1,243 practice sites that treated patients under the age of 18. The national median distance and time traveled to reach a PDL site were 7.8 miles and 14.1 minutes, respectively (Table 1). Children living in urban areas were significantly more likely to travel shorter median travel time and distance (6.1 miles, 11.8 minutes) compared to rural residence (60.9 miles, 66.7 minutes) (p<0.001). Site density is highest in the Northeast and lowest in the Midwest (median distance 5.4 miles and 10.1 miles respectively) (Figure 1). Uninsured children travel longer average distances (32.2 miles) than insured children (24.2 miles). Modest, but statistically significant, differences in travel distance and time exist based on race and age.
Discussion
This study reveals that the majority of children in the United States have limited travel burden in reaching PDL sites. Notably, the varying minimum age requirements of practices do not appear to drive practically significant travel differences among age groups. However, these findings do reveal significant inequities for certain pediatric sub-populations. Rural pediatric populations in particular have a markedly increased travel burden than populations located in urban areas, and these distance discrepancies are likely further exacerbated by the fact that optimal PDL treatment requires multiple treatment sessions at scheduled intervals.4 For population characteristics with modest intergroup distance differences, such as race and insurance status, it is important to note that these disparities are likely amplified by socioeconomic factors influencing the ability of children to obtain transportation to PDL sites. Groups from low-income, uninsured, and racially disadvantaged background have all been shown to face significant barriers to obtaining consistent transport for medical appointments.5
This study is limited by incomplete capture of dermatologists using other PDL devices, exclusion of non-dermatologist physicians who provide PDL treatment, and simplification of heterogeneous population distributions by using population centers. These results underscore the need for greater pediatric PDL access in rural localities and for children’s transportation circumstances to be considered as an important component of their PDL care plan.
References
- Minkis K, Geronemus RG, Hale EK. Port Wine Stain Progression: A Potential Consequence of Delayed and Inadequate Treatment? Lasers Surg Med. 2009;41(6):423.
- Lederhandler MH, Pomerantz H, Orbuch D, et al. Treating pediatric port-wine stains in aesthetics. Clin Dermatol. 2022;40(1):11–18
- Physician Finder. Candela Medical North America. https://candelamedical.com/na/physician-finder. Accessed September 05, 2021.
- Solomon EM, Wing H, Steiner JF, et al. Impact of Transportation Interventions on Health Care Outcomes: A Systematic Review. Med Care. 2020;58(4):384–391.
- Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. J Community Health. 2013;38(5):976–993.