 J Clin Aesthet Dermatol. 2023;16(4):32–37.
J Clin Aesthet Dermatol. 2023;16(4):32–37.
by Khaled Gharib, MD; Wael Seoudy, MD; Mahmoud A. Rageh, MD; Sahar Abdelsatar, MSc; and Elsayed Khater, MD
Drs. Gharib and Khater and Ms. Abdelsatar are with the Department of Dermatology, Faculty of Medicine, Zagazig University in Zagazig, Egypt. Dr. Seoudy is with the Department of Dermatology, Faculty of Medicine, Misr University for Science & Technology in 6th of October City, Egypt. Dr. Rageh is with the Department of Dermatology, Faculty of Medicine, Al-Azhar University in Cairo, Egypt.
FUNDING: No funding was provided for this article.
DISCLOSURES: The authors report no conflicts of interest relevant to the contents of this article.
ABSTRACT: Background. Acne scarring is one of the most dramatic consequences of inflammatory acne. It can lead to physical disfigurement and psychological burden on the affected individuals. Many treatment options for post-acne scarring are used, with variable results. Nonablative lasers, such as the 1,064nm neodymium-doped yttrium aluminum garnet (Nd:YAG) laser, are known to ameliorate acne scar appearance by stimulating collagen production and dermal remodeling.
Objectives. We sought to evaluate the clinical efficacy, safety, and long-term effects of long-pulsed and Q-switched 1,064nm Nd:YAG lasers in the treatment of acne scars.
Methods. From March to December 2019, a total of 25 patients with different skin types with acne scars were treated. Patients were divided into two groups. In Group I, 12 patients received a combination of Q-switched 1,064nm Nd:YAG laser, then long-pulsed 1,064nm Nd:YAG laser. In Group II, 13 patients received a combination of long-pulsed 1,064nm Nd:YAG laser, then Q-switched 1,064nm Nd:YAG laser. All patients received a total of six sessions at two-week intervals.
Results. There were no statistically significant differences between the studied groups in skin type, lesions, or scar type. A positive response with either good or excellent results was documented in 43 patients, corresponding to 86. Six percent of the patients included in this study. Excellent response was observed in a total of 17 patients (26.6%). Twenty-six patients (60%) showed a moderate-to-good response, while seven patients (13.4 %) showed a fair response. The majority of patients in this study had an excellent-to-good response, with an 86.6% improvement of post-acne scars after laser sessions.
Conclusion. Q-switched and long-pulsed 1,064nm Nd:YAG lasers are considered an efficient and safe modality for the treatment of mild and moderate post-acne scars. Both lasers can enhance dermal collagen remodeling and spare the epidermis with minimal downtime after the procedure.
Keywords: Scars, acne scars, Q-switched Nd:YAG laser, long-pulsed Nd:YAG laser
Acne occurs when dead skin cells and oil from the skin are clogged with hair follicles. It affects areas of the skin that have a relatively large number of oil glands, such as the ears, upper chest, and back of the skin. Areas of blackheads or whiteheads, pimples, greasy skin, and potential scarring are described in the literature.1,2
For both the patient and the dermatologist, the treatment of facial acne scars remains a great challenge. Over the years, various therapeutic modalities have been used, including chemical peels, surgical excision, punch grafting, dermabrasion, and filler injection, all with varying results. Incomplete scar removal, poor intraoperative visualization, transmission of infectious debris, scar worsening, tissue fibrosis, and permanent pigmentary alteration associated with these therapeutic modalities have been reported.3
Laser use is an effective post-acne scar treatment and is more promising than other modalities. It is helpful to use various laser types, including nonablative and ablative lasers. The mechanism of lasers involves stimulating the fibroblasts to replace the lost collagen and elastin dermal components in order to fill and complete the scar defect.4
The neodymium-doped yttrium-aluminum-garnet (Nd:YAG) laser is a nonablative laser that has been tested in different parameters to manage post-acne atrophic scarring. Its procedure is generally easy, well-tolerated, simple, and safe and triggers continuous collagen remodeling. However, comparative studies on these devices are lacking.5
The aim of this study was to evaluate the clinical efficacy, safety, and long-term effects in the treatment of acne scars using long-pulsed and Q-switched 1,064nm Nd:YAG lasers.
Patients and Methods
Study design and population. This prospective, split-face, comparative study included 25 patients with acne scars who were recruited from the outpatient clinics of the Dermatology, Venereology and Andrology Department at Zagazig University Hospitals, after obtaining the approval of the Institutional Review Board (IRB: 4763)
Patients were divided into two groups. In Group I, 12 patients received a combination of Q-switched 1,064nm Nd:YAG laser, then long-pulsed 1,064nm Nd:YAG laser. In Group II, 13 patients received a combination of long-pulsed 1,064nm Nd:YAG laser, then Q-switched 1,064nm Nd:YAG laser. All patients received a total of six sessions at two-week intervals.
All participants were fully informed about the nature of this research, the anticipated results, and any potential complications before providing written informed consent.
Clinical evaluation. All patients included in the study were subjected to complete history taking thorough general and dermatological examinations and routine laboratory investigations. Examination of post-acne scars to determine the type of the scars and its severity was completed according to the Goodman and Baron global acne scarring classification.
Patients younger than 18 years of age; patients with keloidal tendency, active acne, immunosuppression, history of herpes simplex, concomitant isotretinion use, pregnancy; and patients who were using any topical treatments for acne scars were all excluded from the study. No concomitant cosmetic procedures were allowed between the laser sessions, and no topical drugs were prescribed, except for sunscreens and topical antibiotic creams, in the postprocedure period.
Treatment protocol. In this study, we used a single operator 1,064nm Q-switched Nd:YAG laser (Medlite IV; Continuum, Santa Clara, California, United States) with an average fluence of 3.4J/cm2, a 6mm spot size, a 4 to 6 nanosecond pulse duration, and a repetition rate of 10Hz. Overlapping pulses were delivered until the immediate treatment endpoint of mild-to-moderate erythema was achieved. A total of six treatments at two-week intervals were administered.
We also used a long-pulsed 1,064nm Nd:YAG laser with an average fluence of 14J/cm2, a three millisecond pulse duration, and a repetition rate of 1Hz. Overlapping pulses were delivered until the immediate treatment endpoint of mild-to-moderate erythema was achieved. A total of six treatments at two-week intervals were administered.
The laser parameters were kept identical at each visit. We treated all patients with the same laser fluence and treatment density irrespective of their depth or morphological type. At the outset, the session took about 10 to 15 minutes to be completed. We recommended six sessions to be done two weeks apart.
Skin care after a laser session is critical for achieving successful results. Effective medications and management techniques can help to minimize the expected effects of the procedure, such as crusting, discomfort, pruritus, erythema, and swelling. As known, immediately after the laser, the skin is dry and desquamated, and after some minutes, erythema and edema occur. The patients were instructed to avoid direct sun exposure for the next 4 to 5 days after each procedure, and a topical nonocclusive antibiotic cream formulation (e.g., fusidic acid) was applied twice daily throughout the following three days after the laser session.
The patients were allowed to wash their face gently using glycerin soaps. The patients were also encouraged to use a broad-spectrum sunscreen every morning 30 minutes before going out and repeat application every two hours. Observed adverse effects were not significant, and none of the enrolled patients had any long-term or permanent side effects from the procedure.
Response to treatment. At the three-month follow-up visit after the last laser session, evaluation of the effects of the laser sessions on patients by comparing digital photos taken before and after the laser sessions was done. The response to laser sessions was classified into excellent, good (moderate), and fair response by two independent, nontreating, blinded dermatologists.
Side effects. The patients were followed up by clinic visit, telephone, or email for adverse events or complications during the first week following the laser session.
Erythema, edema, and hyperpigmentation, if present, were recorded and evaluated at each time period. The final therapeutic effect was evaluated at three months following the last laser treatment.
Statistical analysis. Data were analyzed using Statistical Program for Social Science (SPSS) version 25. Appropriate analysis was performed for every variable based on the type of data collected.
Results
Age was distributed as mean and standard deviation (SD) of 29.44±4.03 years, with a minimum age of 23 years and a maximum age of 35 years. The majority of patients (84%) were female. (Table 1).
There were no statistically significant differences between the two groups regarding skin type or grade or type of scars (Table 2).
There was a statistically significant decrease in the frequency of inflammation in Group I, compared to Group II, and there was also a statistically significant increase in the frequency of edema in Group I, compared to Group II (Table 3).
There was no significant difference between groups in scar improvement score, except at the fourth treatment session, as Group I had a significantly higher score than Group II. Both groups experienced a significant decreased in scores by the sixth session (Table 4).
There was no significant difference in improvement of scars between groups, but each group experienced significant differences from sessions 1 to 6 (Table 5).
There was no statistical significance difference in bad response among groups (Table 6). There was no statistical significance difference in satisfaction among the studied groups (Table 7). Younger age was significant in the excellent and good response group in Group I only (Table 8). There were no statistically significant differences in the frequency of male patients in the excellent and good response group among groups (Table 9).
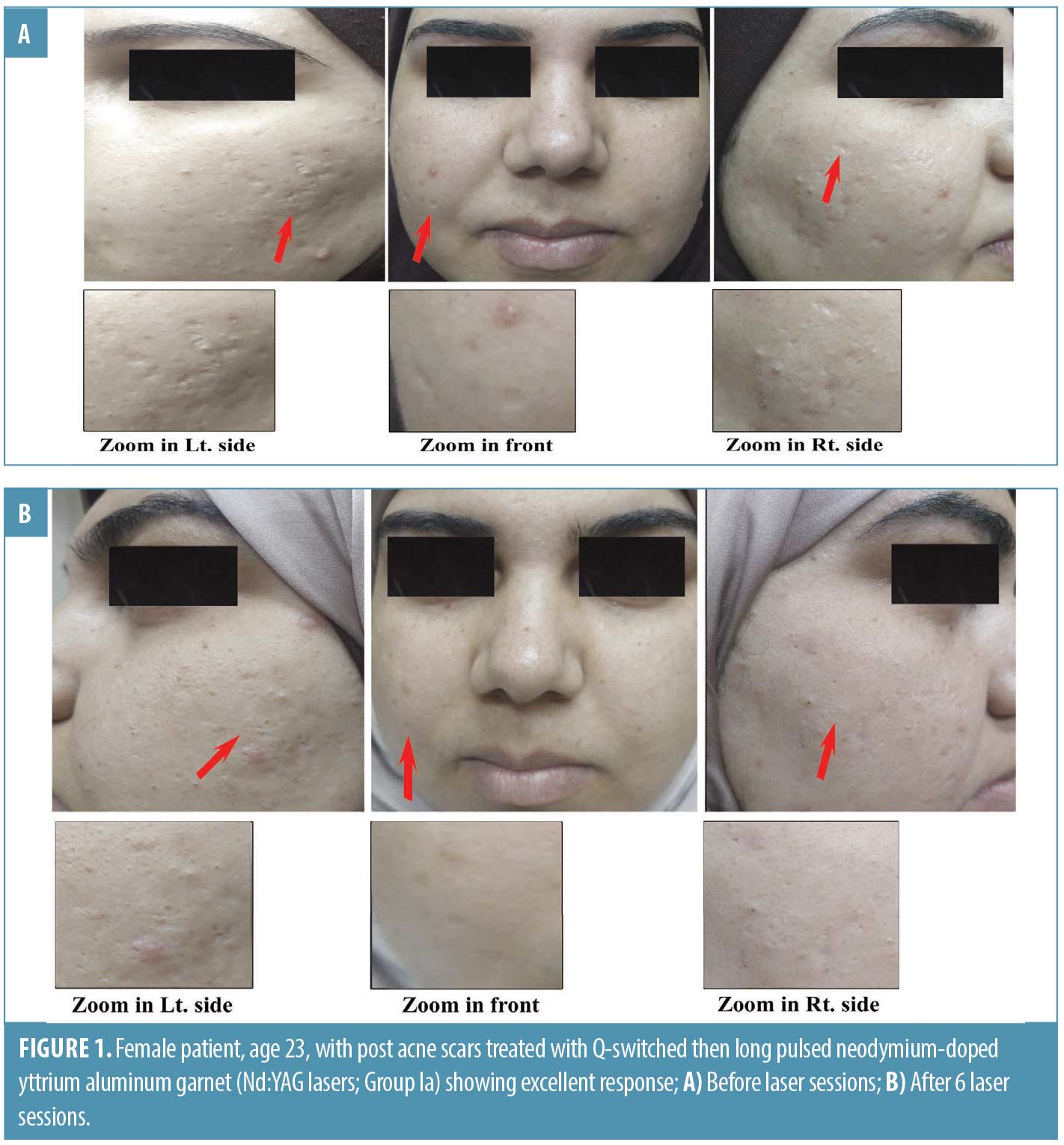
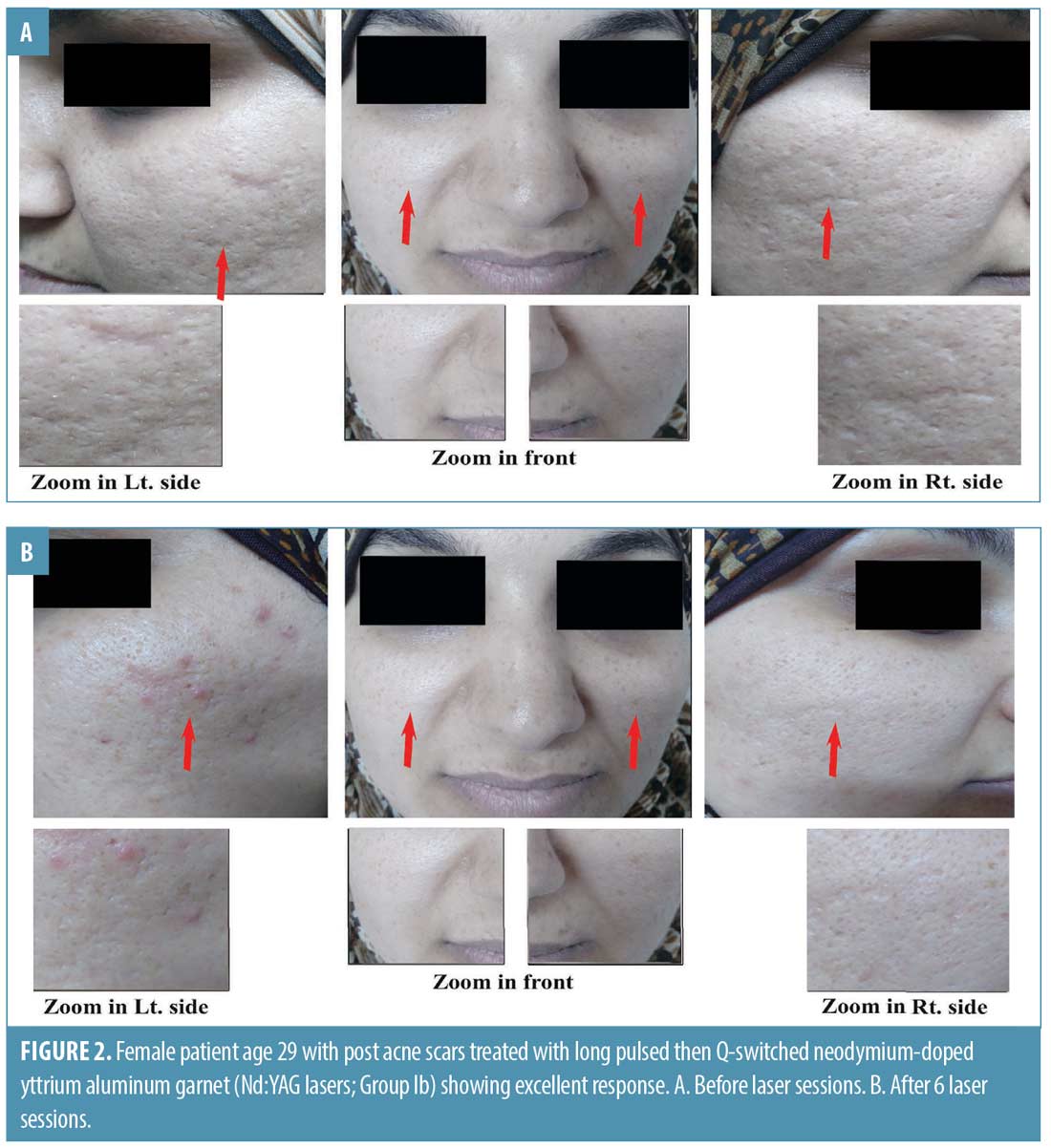
There were no significant associations between treatment response and satisfaction among groups (Table 10). There were no statistically significant associations between the number of sessions and side effects among the studied groups (Table 11 and Figures 1 and 2).
Discussion
Acne vulgaris is a common skin disease that frequently results in scarring. Scars secondary to acne can lead to physical disfigurement, and the psychosocial impact of these acne scars can be profound. Effective treatment of acne is the best means to minimize and prevent acne scarring.6
Treatment of acne scarring creates a challenge for both patients and dermatologists. Each scar type has a different structure needing a personalized treatment approach. The selection of a treatment approach depends upon factors such as the type and degree of acne scarring, patient preference, side effects, cost, and treatment availability. A multimodality approach for scar treatment is necessary to achieve the best cosmetic results.7
Ablative resurfacing lasers are considered an aggressive approach that heat and vaporize superficial skin layers, including the epidermis and upper dermis. The healing process induces collagen remodeling and neocollagenesis, which is responsible for the improved appearance of atrophic scars. Complications include a long recovery period and considerable risk of adverse effects, including infection, dyspigmentation, scarring, discomfort, and prolonged recovery.8
Nonablative lasers (e.g., 585nm pulsed dye laser [PDL], 1,064nm and 1,320nm Nd:YAG laser, and 1,450nm diode laser) are known to ameliorate acne scar appearance by stimulating collagen production and dermal remodeling. Clinical improvements in scar appearances of 40 to 50 percent have been observed following such nonablative laser treatments, and minimal downtime and a low risk of adverse events compensate for the lower efficacies of these modalities.9,10
Nonablative lasers leave the epidermis intact while delivering dermal laser irradiation, with concomitant surface cooling measures. However, the absence of epidermal damage also appears to be associated with the absence of a true wound healing response and therefore, minimal efficacy.11
Results of this study were consistent with those reported by Friedman et al,12 who had reported an 8.9% improvement in roughness analysis at midtreatment (1 month after the third treatment session). This improvement increased to 23.3, 31.6, and 39.2 percent at one, three, and six months after the fifth treatment, respectively. Patients reported mild-to-moderate pain with treatment. The only adverse effects noted were transient erythema and mild pinpoint petechiae.12
Results of this study were also consistent with the study by Friedman et al13 in which 11 patients (8 women, 3 men; age: 28–50 years; skin phototypes I–III) with mild-to-moderate atrophic acne scarring were included; patients showed significant qualitative and quantitative improvements in their facial acne scars. They received five treatment sessions with the Q-switched 1,064nm Nd:YAG laser (3.5J/cm2, 2 fluence, 6mm spot size); improvements increased to a plateau by the six-month evaluation. Continued improvements were observed several months after the last nonablative laser session, suggesting that continued long-term dermal remodeling occurs even after cessation of actual laser treatment.13
A study done in Brazil on the efficacy of 1,064nm Nd:YAG laser for treating atrophic facial scars showed that the 1,064nm Nd:YAG laser was a safe and effective nonablative method for improving atrophic scars, even in darker skin.14
Similarly, an Egyptian study by Sabry et al11 showed that Q-switched 1,064nm Nd: YAG laser could be a promising, safe option for the management of atrophic post-acne scars.11
Min et al15 showed that the long-pulsed Nd:YAG laser improved the appearance of atrophic acne scars with minimal discomfort. Histologic evaluations revealed significantly greater collagen deposition. Conversely, Maluki and Falih16 reported that the efficacy of the Q-switched laser for atrophic acne scars was conflicting, and there were no significant improvements after five treatments with the Q-switched 1,064nm Nd:YAG laser, although it was an easy procedure and well tolerated by the patients.
Nd:YAG lasers are known to induce heat shock protein 70 and procollagen I from scattered dendritic cells in the dermis, which leads to collagen deposition in the papillary dermis.15
We demonstrated that the 1,064nm Nd:YAG laser provides a safe and effective noninvasive treatment for mild-to-moderate facial acne scarring. The results continued well beyond the last treatment, indicating ongoing collagen remodeling after completion of the laser treatment sessions. Nonablative treatment with the Q-switched 1,064nm Nd:YAG laser offers significant advantages to patients in terms of its minimal recovery period and minimal risk of infectious and pigmentary complications.12
Conclusion
In our study, Q-switched and long-pulsed 1,064nm Nd:YAG lasers demonstrated efficiency and safety as a modality for the treatment of mild-to-moderate post-acne facial scars, particularly in patients who were 30 to 40 years of age with skin phototype IV. There was no post-procedure downtime, and daily activity among patients was not disturbed during this study. The side effects of the laser were transient, with low incidence, and self-limited.
References
- Hazarika N. Acne vulgaris: new evidence in pathogenesis and future modalities of treatment. J Dermatolog Treat. 2021;32(3):277–285.
- Moradi Tuchayi S, Makrantonaki E, Ganceviciene R, et al. Acne vulgaris. Nat Rev Dis Primers. 2015;1:15029.
- Rivera AE. Acne scarring: a review and current treatment modalities. J Am Acad Dermatol. 2008;59(4):659–676.
- Cohen BE, Brauer JA, Geronemus RG. Acne scarring: a review of available therapeutic lasers. Lasers Surg Med. 2016;48(2):95–115.
- Feng H, Wu Y, Jiang M, et al. The efficacy and safety of fractional 1064nm Nd:YAG picosecond laser combined with intense pulsed light in the treatment of atrophic acne scar: a split-face study. Lasers Surg Med. 2021;53(10):1356–1363.
- Well D. Acne vulgaris: a review of causes and treatment options. Nurse Pract. 2013;38(10):22–32.
- Zaleski-Larsen LA, Fabi SG, McGraw T, Taylor M. Acne scar treatment: a multimodality approach tailored to scar type. Dermatol Surg. 2016;42 Suppl 2:S139–S149.
- Sobanko JF, Alster TS. Management of acne scarring, part I: a comparative review of laser surgical approaches. Am J Clin Dermatol. 2012;13(5):319–330.
- Alster T, Zaulyanov L. Laser scar revision: a review. Dermatol Surg. 2007;33(2):131–140.
- Lee DH, Choi YS, Min SU, et al. Comparison of a 585-nm pulsed dye laser and a 1064-nm Nd:YAG laser for the treatment of acne scars: a randomized split-face clinical study. J Am Acad Dermatol. 2009;60(5):801–807.
- Sabry HH, Hegazy MS, Ahmed E, Salem RM. Q-switched 1064-nm Nd: YAG laser versus fractional carbon dioxide laser for post acne scarring: a split-face comparative study. Photodermatol Photoimmunol Photomed. 2022;38(5):465–470.
- Friedman PM, Jih MH, Skover GR, et al. Treatment of atrophic facial acne scars with the 1064-nm Q-switched Nd:YAG laser: six-month follow-up study. Arch Dermatol. 2004;140(11):1337–1341.
- Friedman PM, Skover GR, Payonk G, et al. 3D in-vivo optical skin imaging for topographical quantitative assessment of non-ablative laser technology. Dermatol Surg. 2002;28(3):199–204.
- Keller R, Belda Júnior W, Valente NY, Rodrigues CJ. Nonablative 1,064-nm Nd:YAG laser for treating atrophic facial acne scars: histologic and clinical analysis. Dermatol Surg. 2007;33(12):1470–1476.
- Min SU, Choi YS, Lee DH, et al. Comparison of a long-pulse Nd:YAG laser and a combined 585/1,064-nm laser for the treatment of acne scars: a randomized split-face clinical study. Dermatol Surg. 2009;35(11):1720–1727.
- Maluki AH, Mohammad FH. Treatment of atrophic facial scars of acne vulgaris by Q-switched Nd:YAG (Neodymium: Yttrium-Aluminum-Garnet) laser 1064 nm wavelength. J Cosmet Laser Ther. 2012;14(5):224–233.

