J Clin Aesthet Dermatol. 2024;17(7):43–49.
J Clin Aesthet Dermatol. 2024;17(7):43–49.
by Shifa Nurzahra Zaki, MD; Mardyansyah, MD; Caroline Oktarina, MD; Reza Yuridian Purwoko, MD, PhD; and Hans Utama Sutanto, MD
Dr. Zaki is with the Faculty of Medicine at Trisakti University in Jakarta, Indonesia. Dr. Mardyansyah is with the Faculty of Medicine, Trisakti University, Jakarta, Indonesia. Dr. Oktarina is with the Regenerative Medicine and Research Institute at Mandaya Hospital Group in Jakarta, Indonesia. Dr. Purwoko is with the Regenerative Medicine and Research Institute at Mandaya Hospital Group in Jakarta, Indonesia. Dr. Sutanto is with the Regenerative Medicine and Research Institute at Mandaya Hospital Group in Jakarta, Indonesia.
FUNDING: No funding was provided for this article.
DISCLOSURES: The authors have no conflicts of interest relevant to the contents of this article.
ABSTRACT: Objective. Atopic dermatitis (AD) is a chronic inflammatory skin disease which is associated with a significantly decreased quality of life. Overall, the conventional treatment approaches for moderate to severe AD are prone to relapses. Hence, the exploration of new adjuvant therapies, such as the use of platelet-rich plasma (PRP), is expected to enhance the effectiveness of existing interventions, which remain paramount in improving the quality of life for patients with moderate to severe relapsing AD.
Methods. The literature search primarily focused on original English-language articles on PRP as a therapeutic approach for the management of adult AD. Literature reviews, systematic literature, and meta-analyses were excluded. The databases searched include PubMed/Medline, Science Direct, and Cochrane, up to October 2023. Seven articles were reviewed.
Results. PRP is reported to be used as a therapy for AD in both injectable and topical forms. Various studies showed that PRP could significantly reduce free radical accumulation, proinflammatory mediators, provide healing environment, and restore the metabolic activity disruption. Clinically, PRP therapy was reported to improve clinical symptoms, patient’s satisfaction, quality of life, and reduce frequent recurrence. Mild side effects (pain and ecchymosis) due to the injection were reported. Another advantage is that it is safe to be used in pregnant and breastfeeding women.
Limitations. Heterogeneity of methods in preparing PRP and further research with larger scale standardized protocols are warranted.
Conclusion. PRP yields favorable outcomes when used in AD treatment and can serve as an alternative for moderate to severe or refractory AD through its anti-inflammatory and proliferative properties.
Keywords. Platelet-rich plasma, plasma-rich growth factors, atopic dermatitis
Introduction
Atopic dermatitis (AD) is a chronic inflammatory skin disease with the primary symptom being severe itching, which often persists in severe cases, leading to a decreased quality of life including sleep disturbances and psychological disorders. Other symptoms include recurrent eczema lesions.1,2 The prevalence of AD is higher in children than in adults.3 The prevalence of AD varies worldwide and is increasing on most continents.4,5 Atopic dermatitis carries the highest disease burden among all skin conditions. The burden of AD, measured in disability-adjusted life-years (DALYs), corresponds with its prevalence, with countries in the United States and Europe having the highest DALY rates.5,6 In the research conducted by Cheng et al7 an increased prevalence of AD was found in Asian populations of both children and adults worldwide. This study suggests that Asian immigrant children have a higher risk of developing AD. The likely cause of the increased burden of AD among Asian populations is a complex interplay of genetic and environmental factors.
Basic therapy for AD includes appropriate topical treatment with emollients, trigger avoidance, and patient education programs.8 While topical glucocorticoids remain the primary choice for anti-inflammatory therapy in AD treatment, their long-term use can pose problems, as it may lead to skin atrophy, steroid-induced rosacea, discoloration, purpura, and telangiectasia. Topical calcineurin inhibitors, also known as steroid-sparing immunomodulators, may be used as a first-line treatment for moderate to severe AD; however, they are typically used in combination with topical steroids. It is important to note that topical calcineurin inhibitors have an FDA box warning due to a potential association with malignancies. Systemic treatments including glucocorticosteroids should be used only in exceptional cases such as severe flare-ups and for brief periods of time. Systemic immunomodulators should only be used preferably as interval therapy every few months but not for more than two years. Recent research on the treatment of AD including biological agents has been recently approved. However, the majority of these therapies are not yet available in some countries and can be quite expensive for most patients.8,9 Laboratory testing and monitoring are required for the use of biologic agents, and further research on their long-term use is still needed.10
Platelet-rich plasma (PRP), platelet-rich growth factors (GFs), and platelet-rich fibrin (PRF) matrix are components of autologous blood plasma obtained through differential centrifugation with platelet concentrations above baseline (before centrifugation). These growth factors help in stimulating angiogenesis, vascularization, promoting hair growth, and more.11 Platelet-rich plasma (PRP) has long been utilized in the field of dermatology, particularly in the realm of anti-aging, due to its excellent safety profile and cost-effectiveness.12–14 Apart from skin rejuvenation, PRP is reported to be effective in wound healing, scar revision, alopecia areata, pigmentary disorders, and lichen sclerosus therapy.15 Platelet-rich plasma has been reported to be potentially beneficial as a therapy in reducing erythema and edema following fractional carbon dioxide laser treatment.13 The potential of PRP as a therapeutic approach in managing AD is an area of growing research and interest.16,17 This review highlights current information on PRP as a therapeutic approach for AD, especially in adults and discusses innovative clinical application strategies for improving safety and effectiveness in future research.
Methods
The literature review conducted primarily focused on PRP as a therapeutic approach for the management of adult AD. The inclusion criteria were clinical/case study, using PRP as an intervention, and having atopic dermatitis subjects. Other criteria included originally published English-language articles, published in the last ten years from 2013 to 2023. Exclusion criteria were review articles, proceeding, and articles without full-text access, and articles discussing leukocyte-rich platelet-rich plasma (LR-PRP). Non-English articles were evaluated for pertinence. The databases searched include PubMed/Medline, Science Direct, and Cochrane. The following search string was used: [(“platelet-rich plasma” OR “PRP”) AND (“atopic dermatitis” OR “eczema” OR “atopic march”)].
Results
Composition and mechanism of action of PRP. There is no consensus regarding the definition of PRP. PRP is characterized by platelet concentration volume above the baseline (150.000-350.000/mL) or when the platelet concentration fraction is 3 to 8 times greater than normal levels.18,19 The nomenclature of PRP products varies depending on the concentration of platelets, leukocytes, and different growth factors according to the platelets used during preparation. Therefore, there are known variations like plasma-rich growth factors (PRGF), platelet-rich plasma and growth factors (PRPGF), platelet-rich plasma (PRP), and leukocyte-rich platelet-rich plasma (LR-PRP).18
The elevated platelet concentration and plasma proteins in PRP that exceed physiological levels enables an enhancement of tissue regeneration processes. This is because platelets contain growth factors and other bioactive molecules which play a crucial role in tissue healing. In a state of hemostasis, platelets become activated and aggregate following tissue and vascular damage as part of their hemostatic function. This process continues with the secretion of biologically active proteins and molecules, triggering a cascade of healing processes. The aforementioned growth factors, primarily platelet-derived growth factor (PDGF), transforming growth factor (TGF), platelet factor 4 (PF4), interleukin-1 (IL-1), platelet-derived angiogenesis factor (PDAF), vascular endothelial growth factor (VEGF), epidermal growth factor (EGF), platelet-derived endothelial growth factor (PDEGF), epithelial cell growth factor (ECGF), insulin-like growth factor (IGF), and others play a crucial role in local regeneration functions, including cell proliferation, migration, differentiation, and angiogenesis. Other molecules encompass adhesive proteins, fibrinolytic factors, coagulation factors, proteases and antiproteases, chemokines, cytokines, and antimicrobial proteins.18
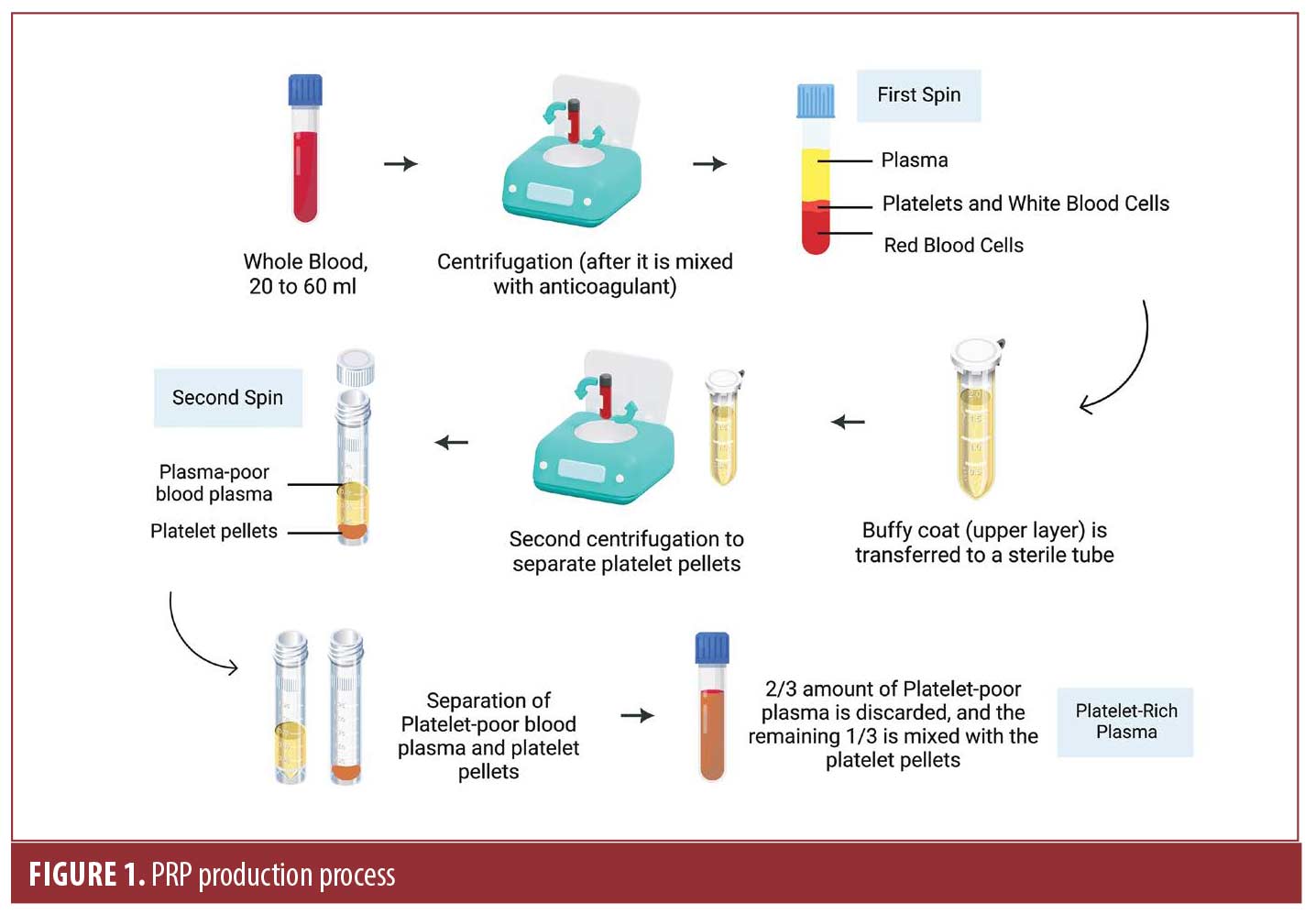
Various techniques are employed to obtain platelet-rich plasma (PRP). Product preparation can begin from scratch or by following the instructions provided by the manufacturers of disposable kits. Typically, 20 to 60mL of fresh blood is used for this purpose.18,20 After obtaining whole blood, it is mixed with citrate in sterilized tubes as an anticoagulant to prevent inadvertent activation before use. These tubes are then subjected to centrifugation, with the speed, duration, and number of spins depending on the chosen method. Usually, this involves at least two rounds of centrifugation. Low-speed centrifugation is recommended to avoid platelet fragmentation and premature protein secretion, which can negatively impact their bioactivity. During centrifugation, three layers with different weights are formed: the bottom layer consists of red blood cells, the middle layer contains platelets and white blood cells, and the top layer is made up of plasma. Depending on the platelet count, the plasma phase can be divided into three different fractions: the platelet-poor fraction, the intermediate fraction, and the platelet-rich fraction. To trigger platelet degranulation and the subsequent release of growth factors and other bioactive molecules, the plasma-rich phase is typically activated, with calcium chloride or thrombin being the most commonly used activators. Degranulation occurs rapidly, so activated PRP must be used immediately after activation. In previous studies, the activated mixture is injected within 10 minutes. PRP can be stored for at least 6 months at a temperature of 70°C without thrombin activation.18–20 Figure 1 describes the process of PRP production.
The use of autologous PRP has been proven to be safe both locally and systemically, with minimal potential for disease transmission because the blood used for the application comes from the individual donor, and there is no evidence of oncogenic potential. If prepared from scratch, sterility testing related to the preparation conditions and product traceability is required. For commercial kits, it is essential to follow the instructions provided by the manufacturer for usage. Additionally, patient follow-up is necessary after its application.18
All of the studies included in this review have generally adhered to the concepts of the methods mentioned. However, depending on the specific method used, the initial blood quantity drawn and the final volume of PRP varies. The lack of standardized methods for preparing PRP itself results in variations in the cellular composition and growth factor concentrations of the PRP used.
PRP therapy in treating AD. Different aspects of PRP application in treating AD. Table 1 summarizes the evidence for the use of PRP in the treatment of AD. Eight studies were found. PRP is reported to be used as a therapy for AD in both injectable and topical forms. Nearly all cases reported the use of PRP in an injectable form.16,17,21–24 Two studies evaluated the use of PRP in topical form25,26 In the ex-vivo study by Anitua et al25 research was conducted to transform the preparation of plasma rich in growth factors (PRGF) into an autologous topical serum (ATS). PRGF is a pioneer in autologous platelet-rich plasma technology.25,27 The ATS preparation process is similar to the PRP preparation process mentioned earlier. After obtaining a volume rich in platelets free of leukocytes at an optimal concentration through centrifugation, the plasma is activated with a PRGF activator to obtain the PRGF supernatant. The remaining plasma was heated in order to provoke plasmatic protein gelation. After vigorously mixing both preparations, the ATS was applied to human organotypic skin explant cultures (hOSECs) that had previously been induced with IL-4 and IL-13 to create a skin model resembling AD. This study reports that ATS formulations yielded a significant improvement in regenerative effects, reducing excessive free radical accumulation, as well as cytokine TNF-α and IL-1β production in the skin during the pathogenesis of AD.25
García-Millan et al26 reported the use of topical Endoret-Serum (ES), that was obtained through autologous PRP, applied twice daily for three months on the faces of subjects with sensitive skin, typically in cases of refractory AD, rosacea, melasma, and seborrheic dermatitis that had previously been prescribed various medications, such as steroid creams, cleansing agents, moisturizer, anti-itching creams, topical antihistamines, and pain relievers. This treatment was found to increase skin hydration and reduce dermal inflammatory infiltrate in some patients, as confirmed by assessments using reflectance confocal microscopic images (RCM). Additionally, it decreased skin inflammation and vascular conditions as observed in topographic images using Reveal. Subject self-assessments indicated improvements in their dermatological condition, satisfaction, and overall quality of life. This is because the presence of growth factors in ES (EGF, IGF-I, PDGF-AB, and TGF-β) was detected using enzyme-linked immunosorbent assay (ELISA) kits.26 These are high-level key proteins involved in skin regeneration.18 The local application of PRP results in supra-physiological concentrations of biologically active substances found in PRP, which modulate pathways related to inflammation and tissue repair.19
The use of PRP in the form of injections can be used as a standalone therapy17,21,24,25 or as an adjuvant in the treatment of AD.16,22 PRP injections can be administered in one to three sessions, with two to four-week intervals. Research in general reports good outcomes for both localized-area AD and AD with broader areas. However, most studies utilize subjective outcome measures. Kauhl et al17 reported that PRP was statistically significant (p < 0.0001) in progressively decreasing lesion size and improving eczema area and severity index (EASI) scores. Half of the patients achieved a complete remission at three months post follow-up. This study involved 40 patients over a period of 53 months, indicating a significant sample size (p < 0.001) and duration that would provide valuable insights into the long-term efficacy and safety of PRP.16,17 Fan et al22 administered PRP through mesotherapy to ensure that PRP was injected into the skin’s superficial dermis layer. Their research has shown that the treatment suggested to improve subjective and objective symptoms in subjects after two mesotherapy sessions. Mesotherapy is an injection technique that employs a mesogun injector machine to inject drugs. PRP is extracted using a specialized syringe attached to a needle. This method aims to modulate drug kinetics and prolong local action by creating nine small holes after a single injection. 22,28 Mesotherapy, as an adjuvant therapy, is also reported to be a favorable method for optimizing the improvement of hyaluronic acid (HA) to restore skin rejuvenation and revitalize the skin.29 Another study by Ghani et al reported that PRP injections successfully reduced all inflammatory biomarkers including (eosinophil, electrocyte sedimentation rate (ESR), C-reactive protein (CRP), and Immunoglobulin E), which showed an improvement in the rash, and effectively controlled itching on patients with chronic AD.24
When used as an adjuvant therapy in cases of moderate to severe AD, PRP suggested a statistically significant improvement in the EASI scores (p<0.001). PRP was reported to be more effective when combined with NB-UVB phototherapy compared to NB-UVB therapy alone in a split-body study.16 This was marked by the gradual decreasing in size and disappearance of skin lesions.16,17 Consequently, the usage of intradermal PRP can reduce the duration of UVB exposures thus resulting in a decrease in cumulative dosage.16 This needs to be taken into account, as NB-UVB has long-term carcinogenic effects per minimal erythema dose (MED), including actinic changes, telangiectasia, lentigines, and basal and squamous cell carcinomas, although the cancer risk associated with UVB is less than 2%. Radiation derived from UVB phototherapy is cumulative with chronic sun exposure. Due to the lack of robust evidence regarding the long-term risk of NB-UVB, the use of PRP as an adjuvant therapy in treating AD might be considered, and further research on the long-term safety of NB-UVB is necessary.30
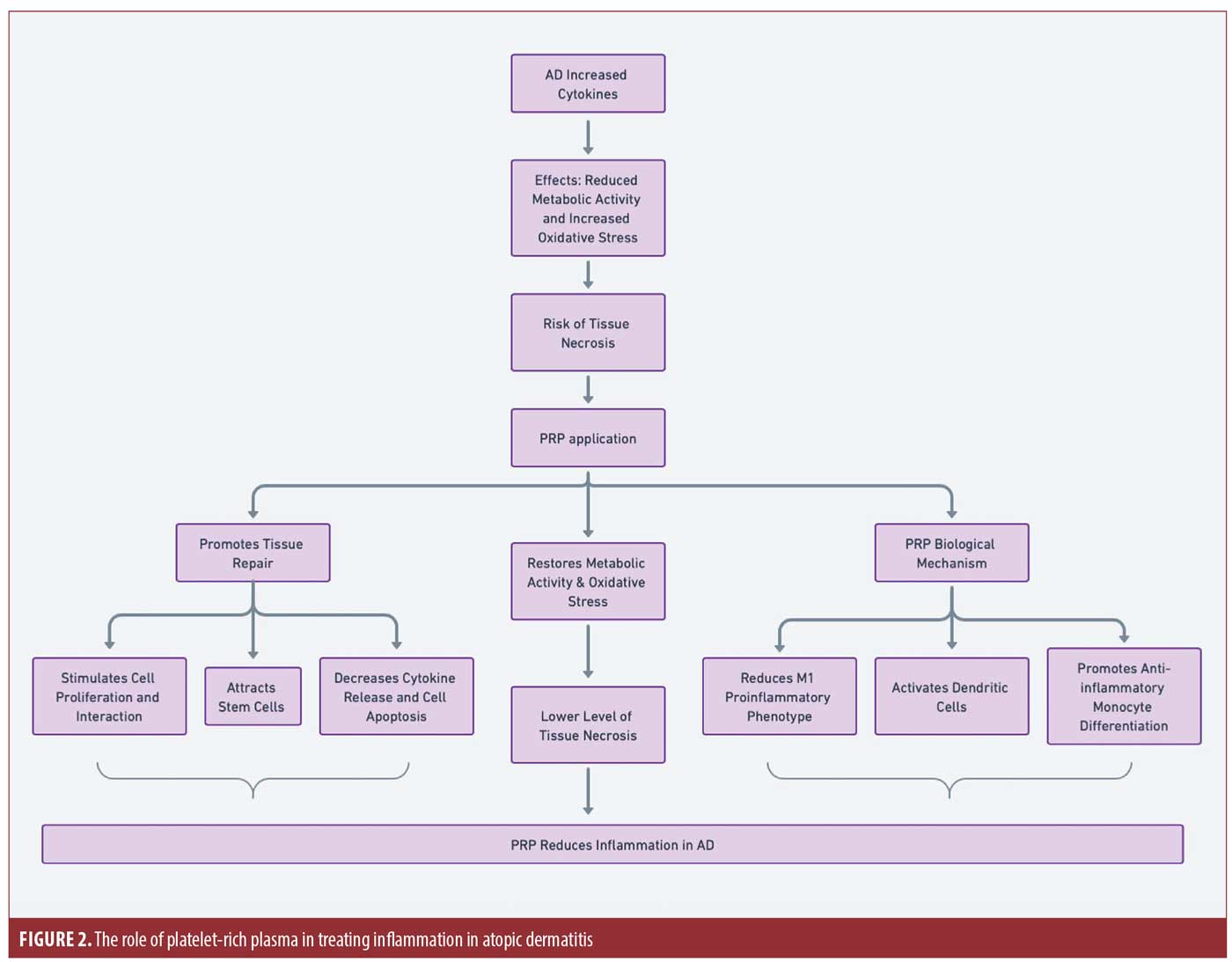
PRP mechanism in treating AD. In AD (Figure 2), there is an increase in cutaneous cytokine production, such as TNF-α and IL-1β. They significantly reduce metabolic activity and increase oxidative stress levels at both 48h and 72h (p=0.000 and 0.037, respectively), which may elevate the risk of tissue necrosis. Intradermal PRGF injection has been reported to restore metabolic activity caused by interleukins and reduce oxidative stress, thereby maintaining tissue necrosis at a lower level.25 The biological mechanism of PRP is also linked to its ability to reduce the macrophage M1 proinflammatory phenotype, activate dendritic cells, and promote monocyte differentiation into an anti-inflammatory cell populations.31,32 These findings suggest that PRP may help reduce inflammation in AD by suppressing the expression of inflammatory genes and promoting tissue repair. PRP plays a role in creating a healing environment by stimulating the proliferation and interaction between keratinocytes and fibroblasts with melanocytes, attracting and stimulating undifferentiated stem cells, and reducing inflammation by decreasing cytokine release, which is followed by a decrease in cell apoptosis in reducing EASI scores in the treatment of AD.16 However, further research is needed to fully understand the mechanism of PRP in treating inflammation in AD.
The advantages and limitations of PRP therapy in treating AD. The management of AD is a complex process that requires adherence to basic therapy in addition to anti-inflammatory measures, such as emollients, trigger avoidance, and patient education programs, including appropriate skin cleansing with the avoidance of strong alkaline detergents and irritating measures.8 A case report published by Vafaei-Nodeh and Kabiri-Abyaneh23 highlights AD as a chronic condition often initiating in childhood but also prevalent in adulthood. In their report, traditional treatments such as moisturizers and topical corticosteroids did not offer adequate disease control, suggesting a potential therapeutic gap that PRP could fill. Furthermore, there were no recurrences of eczematous lesions for two years without the use of topical corticosteroids, a significant observation that underscores the potential of PRP as a standalone therapy.23 The case report finding that PRP can trigger a wound-healing cascade involving inflammation and tissue regeneration aligns well with the known properties of PRP, which includes the release of growth factors from platelets that promote skin health. The absence of AD symptoms for an extended period post-PRP therapy suggests a durable effect of PRP in modulating skin inflammation and repairing the skin barrier, which are central pathological facets of AD.
Nevertheless, in some studies, the recurrence of AD was still observed, albeit over an extended period.16,21,23 Out of the 44 subjects studied, only two subjects who were being treated with the combination of PRP and NB-UVB therapy, experienced a recurrence on their right side whereas a total of six subjects in the control group who received the NB-UVB treatment on the left side of their body experienced a recurrence.16 The use of PRP therapy as an adjuvant treatment in AD has been reported to improve the long-term recurrence of AD in several cases (lasting from months to years). Recurrence has also been reported four months after the combination therapy of NB-UVB and PRP, while those who received only NB-UVB therapy showed symptoms recurring as early as the second month post-treatment. Other studies referenced reported recurrence within one to two years post PRP therapy.16,21,23 Additionally, PRP also improved the symptoms when AD recurred.21 The case study’s findings, with the prolonged remission of AD symptoms following PRP therapy, opens an intriguing avenue for further research into PRP’s role in treating AD and possibly other dermatologic conditions.
Regarding the area treated, whether on the face or body, PRP administration can be effectively performed through both injections and topical applications. There are two studies reporting treatment solely on the patients’ faces. One study22,23 reports the effectiveness of PRP administration through injection, while another study reported its administration through mesotherapy. Mesotherapy treatment on the face was reported to reduce the occurrence of injection pain side effects.33 Typically, this was followed by the use of a sterile face mask.22 García-Millan et al26 reported facial treatment using topical serum. However, for whole body treatment, the majority of studies reported effective results with injections alone.16,17,21,24
The degree of evidence is limited by heterogeneity in PRP preparation and administration, as well as the lack of standardization in outcome measures. Moreover, the duration of the effects of PRP therapy remains unclear. Only one of the studies was randomized, which might have led to an overestimation of effectiveness. Most studies were conducted with a small number of participants. Further large-scale research with a randomized design that includes control groups and blinding is needed to minimize bias and optimize the efficacy of PRP therapy for AD in the future. To ensure that the control group represents the current best practice for AD; consider long-term follow-up to evaluate sustained effects, standardization of the PRP preparation protocol process; and use standardized photographic documentation to evaluate changes in skin lesions. Subgroup analysis may be considered for different age groups and severity of atopic dermatitis. Furthermore, it is important to examine patient adherence to basic therapies such as emollient use, soap-free cleansers, and trigger prevention, as well as determining the optimal number of sessions and intervals between them to achieve the best results.8
Potential side effects and safety of PRP therapy as a therapeutic approach for AD. PRP therapy has been shown to be a safe treatment for a long time.18 When used in the treatment of AD, the use of PRP has been reported to be safe. No adverse events related to the composition of PRP itself were found. Some side effects have been reported with its use through injections, but they are not severe. Yosef et al16 reported that adverse events occurred in 22 out of 44 cases receiving PRP therapy for AD (54.6%). The adverse events were mild, including tolerable pain at the injection site and ecchymosis was reported in three cases.16 The utilization of the mesogun injector machine to administer PRP was minimally invasive and was well-received by all patients during the trial. The negative pressure created during the injection process lifts the skin, separating the injected area from the blood vessels beneath the skin, thus reducing the risk of significant bleeding and hematoma.22 Kauhl et al17 reported that there were no side effects related to PRP injection.
Administering PRP therapy through topical application has caused no notable or significant side effects.25,26 Additionally, this type of therapy can be easily used in the clinical setting.26 Furthermore, Karina et al21 reported that PRP is safe for use in pregnant women. They reported that there were no complications during pregnancy until after the infant was born. Despite the recurrence, it was reported that there were no exacerbation symptoms during pregnancy.21
Conclusion
PRP significantly yields favorable outcomes when used in AD treatment and can serve as an alternative for moderate to severe or refractory AD. PRP can reduce the relapse interval of refractory AD and can enhance patient satisfaction overall through its anti-inflammatory and regenerative properties. Its use in AD treatment has been reported to be safe, even during pregnancy. PRP is recommended for use due to the risk for slight adverse events and the minimal risk of transmissible diseases, as it originates from the patient’s own blood. It is important to note that the varying methods in preparing PRP can yield different clinical outcomes. As there is heterogeneity of methods in preparing PRP, future studies with larger scale standardized protocols are warranted. The limitations of existing research can be further addressed to provide recommendations for future studies.
References
- Simpson EL, Leung DYM, Eichenfield LF, et al. Atopic Dermatitis. In: Fitzpatrick’s Dermatology (Sewon K, Amagai M, Bruckner AL, et al., editors), 9th ed. New York: McGraw Hill Education; 2019:364.
- Weidinger S, Novak N. Atopic dermatitis. Lancet. 2016;387(10023):1109–1122.
- Thyssen JP, Corn G, Wohlfahrt J, et al. Retrospective markers of paediatric atopic dermatitis persistence after hospital diagnosis: a nationwide cohort study. Clin Exp Allergy. 2019;49(11):1455–1463.
- Bylund S, Kobyletzki LB, Svalstedt M, et al. Prevalence and incidence of atopic dermatitis: a systematic review. Acta Derm Venereol. 2020;100(12):320–329.
- Abuabara K, Margolis DJ. Do children really outgrow their eczema, or is there more than one eczema? J Allergy Clin Immunol. 2013;132(5):1139–1140.
- Laughter MR, Maymone MBC, Mashayekhi S, et al. The global burden of atopic dermatitis: lessons from the Global Burden of Disease Study 1990-2017. Br J Dermatol. 2021;184(2):304–309.
- Cheng J, Wu JJ, Han G. Epidemiology and characterization of atopic dermatitis in east asian populations: a systematic review. Dermatol Ther. 2021;11(3):707–717.
- Wollenberg A, Werfel T, Ring J, et al. Atopic dermatitis in children and adults—diagnosis and treatment. Dtsch Arztebl Int. 2023;120:224–234.
- Frazier W, Bhardwaj N. Atopic dermatitis: Diagnosis and treatment. Am Fam Physician. 2020;101(10):590–598.
- Torres AE, Lyons AB, Hamzavi IH, et al. Role of phototherapy in the era of biologics. J Am Acad Dermatol. 2021;84(2):479–485.
- Alves R, Grimalt R. A review of platelet-rich plasma: history, biology, mechanism of action, and classification. Skin Appendage Disord. 2018;4(1):18–24.
- Alam M, Hughart R, Champlain A, et al. Effect of platelet-rich plasma injection for rejuvenation of photoaged facial skin: a randomized clinical trial. JAMA Dermatol. 2018; 154(12):1447–1452.
- Kim H, Gallo J. Evaluation of the effect of platelet-rich plasma on recovery after ablative fractional photothermolysis. JAMA Facial Plast Surg. 2015;17(2):97–102.
- Gawdat HI, Tawdy AM, Hegazy RA, et al. Autologous platelet-rich plasma versus readymade growth factors in skin rejuvenation: a split face study. J Cosmet Dermatol. 2017;16(2):258–264.
- White C, Brahs A, Dorton D, et al. Platelet-rich plasma: A comprehensive review of emerging applications in medical and aesthetic dermatology. J Clin Aesthet Dermatol. 2021;14(11):44–57.
- Yosef A, Elkady N, Khattab F. Possible clinical efficacy and tolerability of platelet-rich plasma with atopic dermatitis. J Cosmet Dermatol. 2021;20(10):3264–3269.
- Kauhl W, Pototschnig H, Paasch U. Can platelet-rich plasma reduce the burden of inflammatory skin diseases such as psoriasis and atopic dermatitis? Cureus. 2021;13(10):e18472.
- Conde Montero E, Fernández Santos ME, Suárez Fernández R. Platelet-rich plasma: applications in dermatology. Actas Dermosifiliográficas. 2015;106(2):104-111.
- Zhang M, Park G, Zhou B, et al. Applications and efficacy of platelet-rich plasma in dermatology: clinical review. J Cosmet Dermatol. 2018;17(5):660–655.
- Lynch MD, Bashir S. Applications of platelet-rich plasma in dermatology: a critical appraisal of the literature. J Dermatolog Treat. 2016;27(3):285–289.
- Karina K, Mahardika A, Krisandi G, et al. The efficacy and safety of autologous activated platelet-rich plasma therapy as adjuvant treatment of atopic dermatitis in pregnant woman. JHSCI. 2023;13(2):129–131.
- Fan X, Yin Y, Dou W, et al. Successful treatment of corticosteroid-induced rosacea-like dermatitis with platelet-rich plasma mesotherapy: report of seven cases. Dermatol Ther. 2021;11(2):615–623.
- Vafaei-Nodeh S, Kabiri-Abyaneh S. Long-term control of atopic dermatitis with platelet-rich plasma. JAAD Case Rep. 2021;7:54–56.
- Ghani R, Hingorjo MR, Fatima U, et al. Platelet-rich plasma use in the treatment of eczema (atopic dermatitis): a case report. Glob Sci J. 2018;6(12):22–31.
- Anitua E, Pino A, Aspe L, et al. Anti-inflammatory effect of different PRGF formulations on cutaneous surface. J Tissue Viability. 2021;30(2):183–189.
- García-Millan C, Pino A, Rodrigues R, et al. An autologous topical serum derived from platelet-rich plasma therapy for the management of sensitive skin alterations: a case series report. Clin Cosmet Investig Dermatol. 2022;15:2077–2086.
- Buzalaf MAR, Levy FM. Autologous platelet concentrates for facial rejuvenation. J Appl Oral Sci. 2022;30:e20220020.
- Mammucari M, Maggiori E, Russo D, et al. Mesotherapy: from historical notes to scientific evidence and future prospects. ScientificWorldJournal. 2020;2020:1–9.
- Iranmanesh B, Khalili M, Mohammadi S, et al. Employing hyaluronic acid-based mesotherapy for facial rejuvenation. J Cosmet Dermatol. 2022;21(12):6605–6618.
- Chen X, Yang M, Cheng Y, et al. Narrow-band ultraviolet B phototherapy versus broad-band ultraviolet B or psoralen-ultraviolet A photochemotherapy for psoriasis. Cochrane Database Syst Rev. 2013;10:CD009481.
- Zhang J, Yin C, Zhao Q, et al. Anti-inflammation effects of injectable platelet-rich fibrin via macrophages and dendritic cells. J Biomed Mater Res A. 2020;108(1):61–68.
- Papait A, Cancedda R, Mastrogiacomo M, et al. Allogeneic platelet-rich plasma affects monocyte differentiation to dendritic cells causing an anti-inflammatory microenvironment, putatively fostering wound healing. J Tissue Eng Regen Med. 2018;12(1):30–43.
- Gowda A, Healey B, Ezaldein H, et al. A systematic review examining the potential adverse effects of microneedling. J Clin Aesthet Dermatol. 2021; 14(1): 45–54.